Sunday Poster Session
Category: IBD
P1247 - An Atypical Presentation of Ulcerative Colitis in a Patient with Active Non-Steroidal Anti-Inflammatory Drug (NSAID) Use
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Landys Z. Guo, MSc
College of Medicine, University of Kentucky
Lexington, KY
Presenting Author(s)
Landys Z. Guo, MSc, Ren Bryant, DO, Krista L. Perry, DO
College of Medicine, University of Kentucky, Lexington, KY
Introduction: The differential from hematochezia can range from drug-induced or infectious colitis to IBD. Colonoscopy is considered as a definitive mode of diagnosis, providing gross/microscopic data. But histological similarities are observed among NSAID-induced colitis, Crohn's disease (CD) and infectious colitis. NSAIDs direct link to inflammatory colitis is still unclear. The IBD-serology, genetic, inflammatory (IBD-SGI) panel is a novel, noninvasive blood-based diagnostic tool that may be a decisive factor for those with various risks of IBD.
Case Description/
Methods: A 39 yo male with history of external hemorrhoids presented with a chief complaint of hematochezia, increased stool frequency, bloating, cramping and loose stools. Due to recent MSK injury, patient (pt) used high-dose NSAID daily. Physical exams and initial labs (tissue transglutaminase-IgA, CRP, ESR, B12, folate, iron and total iron binding capacity) were normal. CBC revealed a new mild anemia with low ferritin. Fecal calprotectin was markedly elevated. Colonoscopy found 3 pedunculated polyps and continuous, circumferential inflammation up to the splenic flexure (Figs 1-6). Biopsies of the inflamed area showed crypt disarray, rare crypt abscesses, Paneth cell metaplasia, and eosinophilic cryptitis, consistent with focal colitis. Further evaluation with the IBD-SGI panel suggested ulcerative colitis (UC). Pt began treatment for anemia secondary to hematochezia and biologic therapy for UC.
Discussion: This case of UC conflicted with pathology interpretation. Paneth cell metaplasia is known to have a correlation with chronic inflammation, including IBD. Eosinophilic infiltration is rare in IBD but more commonly found with inflammation from NSAIDs use. Mucosal barrier reduction from NSAID may cause imbalance with the intestine’s microbiome leading to dysbiosis and inflammation. The IBD SGI panel is highly specific, sensitive in distinguishing non-IBD vs IBD and UC vs CD (Table 1). The serological test detects loss of tolerance to bacterial proteins and flagella and indicates reactivity to endogenous microbiome patterns found in IBD pathologies (Fig 7). We report a case of UC with inconclusive biopsies given pt’s history of chronic NSAID use in which IBD-SGI panel was used to tie a clear link between pt’s symptoms and markers with a diagnosis of UC, indicating that IBD-SGI panel provides great insight to rule out differentials and reduce delayed diagnoses in pts with multiple risk factors for IBD, thus may be a great aid for precise diagnosis.
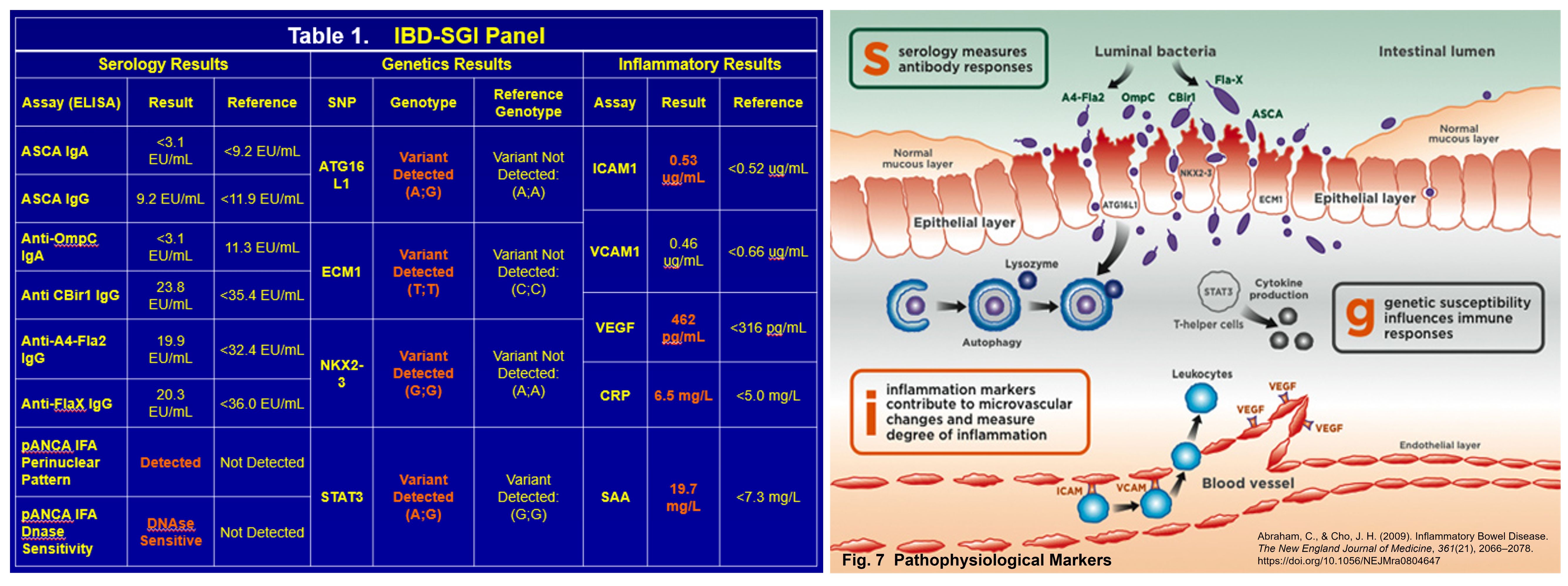
Figure: Colonoscopy Results
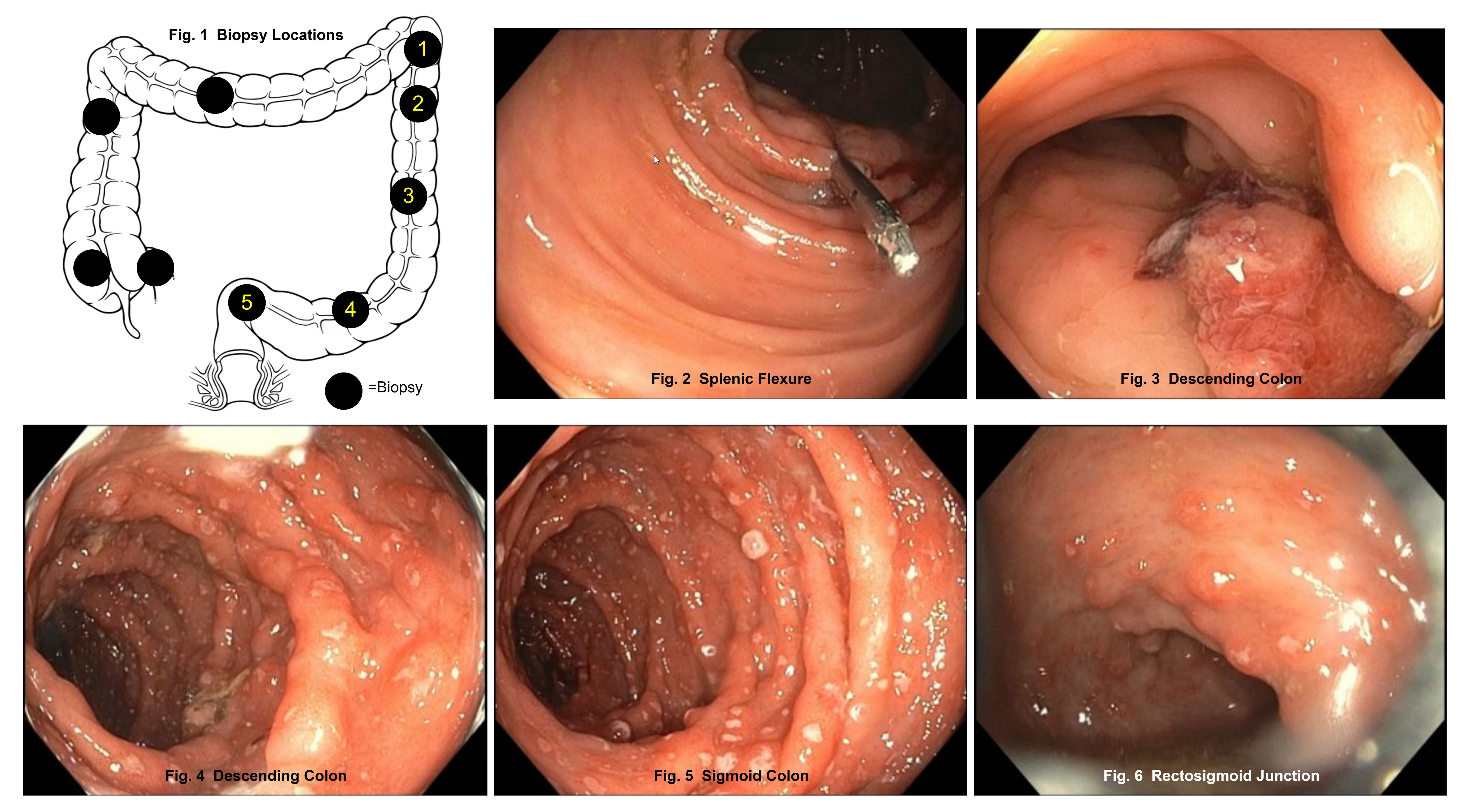
Figure: Results from IBD-SGI Panel and Mechanisms of Pathophysiological Markers
Disclosures:
Landys Guo indicated no relevant financial relationships.
Ren Bryant indicated no relevant financial relationships.
Krista Perry indicated no relevant financial relationships.
Landys Z. Guo, MSc, Ren Bryant, DO, Krista L. Perry, DO. P1247 - An Atypical Presentation of Ulcerative Colitis in a Patient with Active Non-Steroidal Anti-Inflammatory Drug (NSAID) Use, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
College of Medicine, University of Kentucky, Lexington, KY
Introduction: The differential from hematochezia can range from drug-induced or infectious colitis to IBD. Colonoscopy is considered as a definitive mode of diagnosis, providing gross/microscopic data. But histological similarities are observed among NSAID-induced colitis, Crohn's disease (CD) and infectious colitis. NSAIDs direct link to inflammatory colitis is still unclear. The IBD-serology, genetic, inflammatory (IBD-SGI) panel is a novel, noninvasive blood-based diagnostic tool that may be a decisive factor for those with various risks of IBD.
Case Description/
Methods: A 39 yo male with history of external hemorrhoids presented with a chief complaint of hematochezia, increased stool frequency, bloating, cramping and loose stools. Due to recent MSK injury, patient (pt) used high-dose NSAID daily. Physical exams and initial labs (tissue transglutaminase-IgA, CRP, ESR, B12, folate, iron and total iron binding capacity) were normal. CBC revealed a new mild anemia with low ferritin. Fecal calprotectin was markedly elevated. Colonoscopy found 3 pedunculated polyps and continuous, circumferential inflammation up to the splenic flexure (Figs 1-6). Biopsies of the inflamed area showed crypt disarray, rare crypt abscesses, Paneth cell metaplasia, and eosinophilic cryptitis, consistent with focal colitis. Further evaluation with the IBD-SGI panel suggested ulcerative colitis (UC). Pt began treatment for anemia secondary to hematochezia and biologic therapy for UC.
Discussion: This case of UC conflicted with pathology interpretation. Paneth cell metaplasia is known to have a correlation with chronic inflammation, including IBD. Eosinophilic infiltration is rare in IBD but more commonly found with inflammation from NSAIDs use. Mucosal barrier reduction from NSAID may cause imbalance with the intestine’s microbiome leading to dysbiosis and inflammation. The IBD SGI panel is highly specific, sensitive in distinguishing non-IBD vs IBD and UC vs CD (Table 1). The serological test detects loss of tolerance to bacterial proteins and flagella and indicates reactivity to endogenous microbiome patterns found in IBD pathologies (Fig 7). We report a case of UC with inconclusive biopsies given pt’s history of chronic NSAID use in which IBD-SGI panel was used to tie a clear link between pt’s symptoms and markers with a diagnosis of UC, indicating that IBD-SGI panel provides great insight to rule out differentials and reduce delayed diagnoses in pts with multiple risk factors for IBD, thus may be a great aid for precise diagnosis.
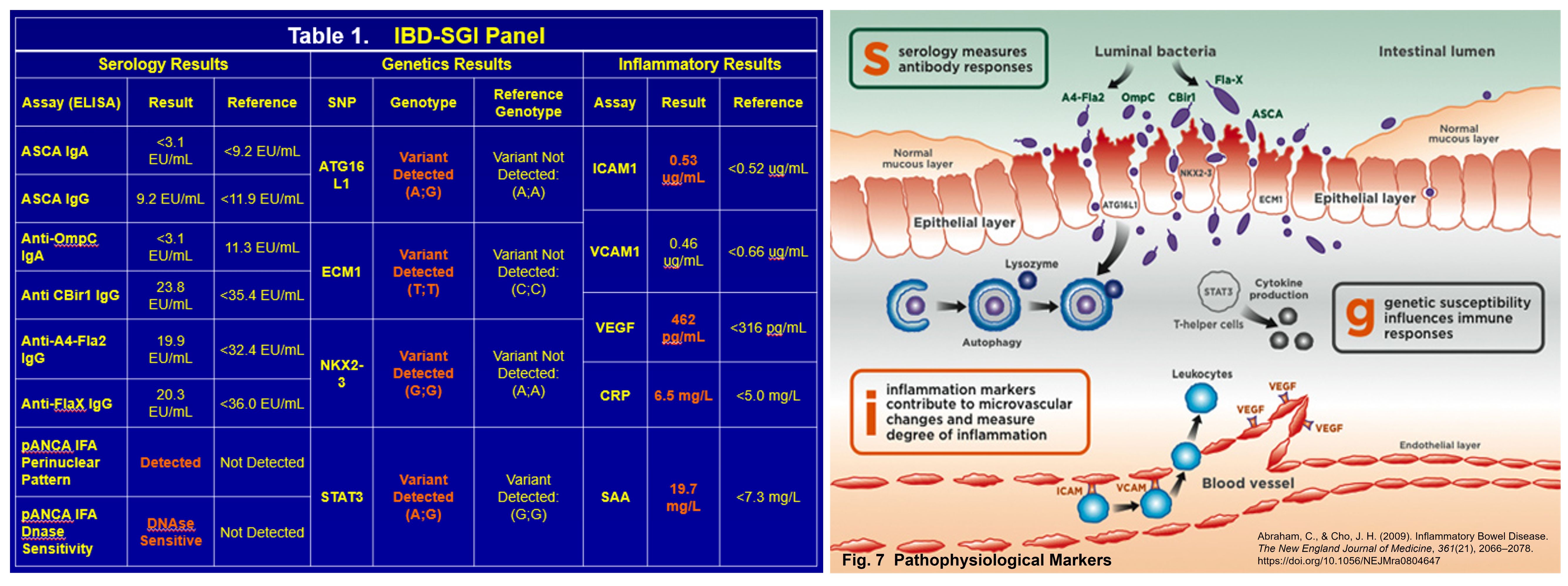
Figure: Colonoscopy Results
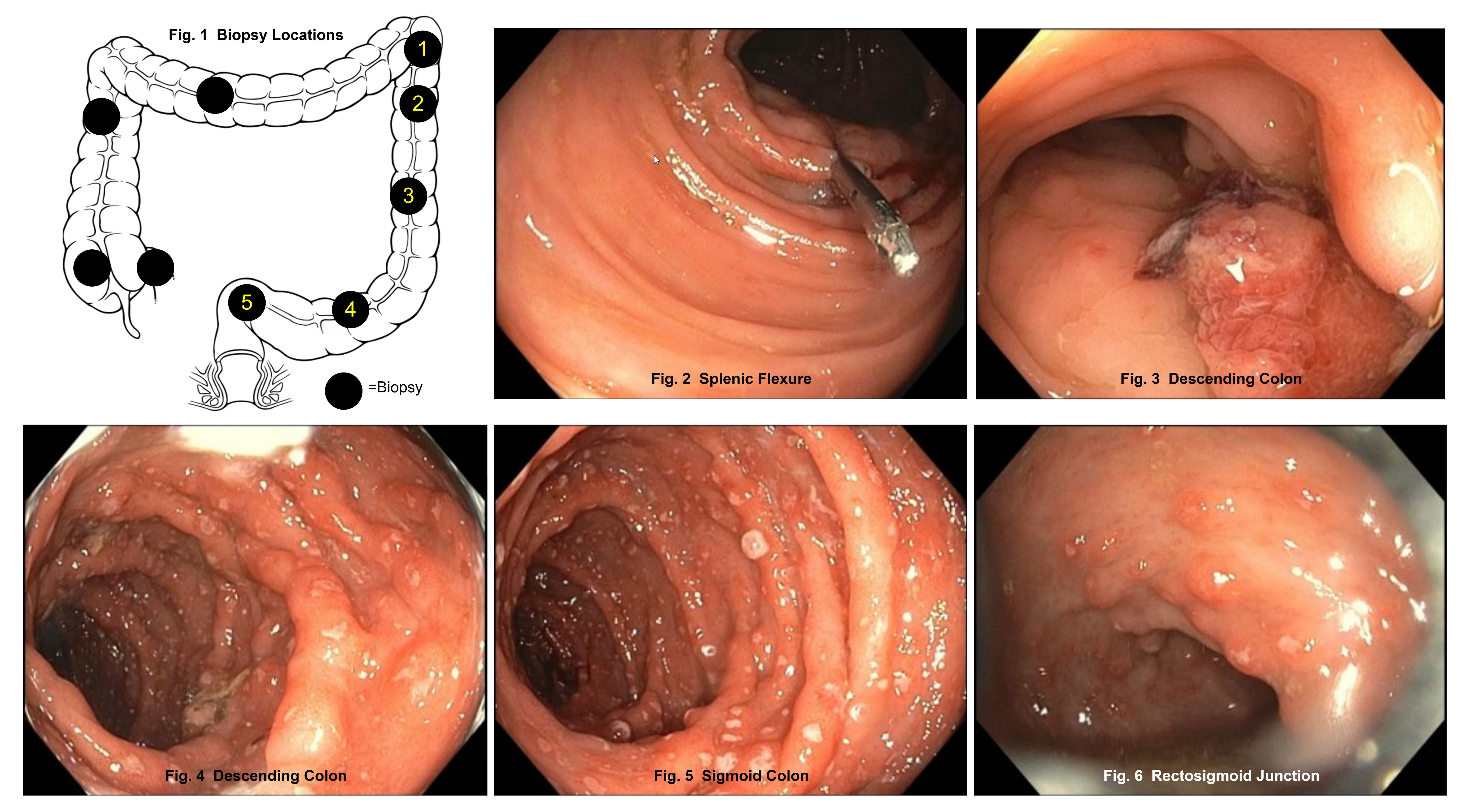
Figure: Results from IBD-SGI Panel and Mechanisms of Pathophysiological Markers
Disclosures:
Landys Guo indicated no relevant financial relationships.
Ren Bryant indicated no relevant financial relationships.
Krista Perry indicated no relevant financial relationships.
Landys Z. Guo, MSc, Ren Bryant, DO, Krista L. Perry, DO. P1247 - An Atypical Presentation of Ulcerative Colitis in a Patient with Active Non-Steroidal Anti-Inflammatory Drug (NSAID) Use, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
