Sunday Poster Session
Category: Infections and Microbiome
P1327 - Gastrointestinal Tuberculosis Presenting as a Massive Lower GI Bleed in a Patient With Newly Diagnosed HIV/AIDS
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- HS
Hamzah Shariff, MD
Thomas Jefferson University Hospital
Philadelphia, PA
Presenting Author(s)
Kevan Josloff, MD, MPH1, Hamzah Shariff, MD1, Kathleen Spritzer, BS2, Wei Jiang, MD1, Anna Chen, MD1, Leo Katz, MD, FACG1
1Thomas Jefferson University Hospital, Philadelphia, PA; 2Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA
Introduction: Gastrointestinal Tuberculosis (GI TB) is an uncommon sequela of TB, occurring in approximately 3% of all TB cases worldwide. In the United States, many cases are seen in migrant populations or in immunocompromised individuals. The classic presentation of GI TB is non-specific abdominal pain not typically associated with significant bleeding. We present a case of GI TB complicated by life-threatening lower GI bleed requiring vasopressor support in a patient with newly diagnosed HIV/AIDS.
Case Description/
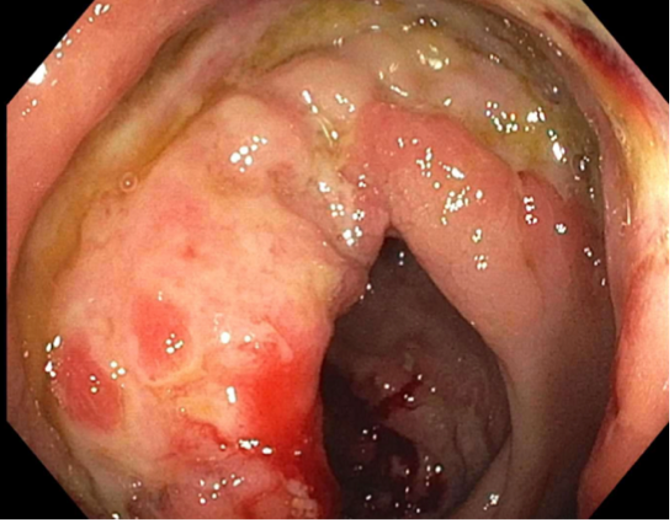
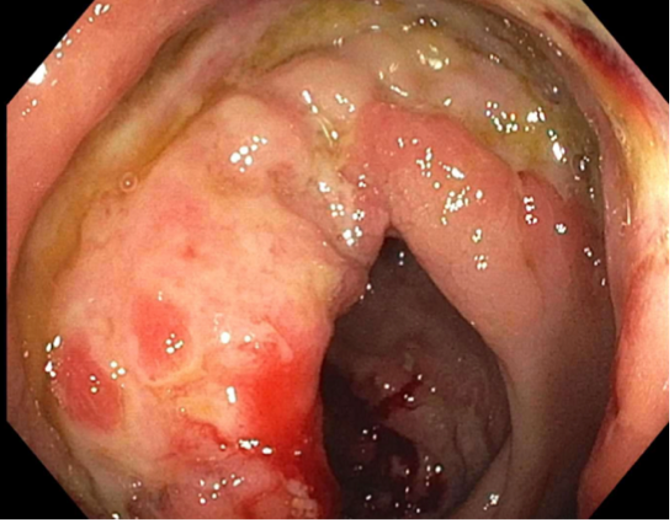
Methods: A 25-year-old male who recently immigrated to the Unites States from Peru presented with several weeks of abdominal pain and scant bright red blood per rectum. On presentation his hemoglobin was 7.6, and he was also found to have a new diagnosis of HIV with viral load 2.87 million copies and CD4+ count of 128. CT abdomen pelvis showed circumferential wall thickening of the cecum and proximal ascending colon, with extensive necrotizing lymphadenopathy throughout the mesentery (Figure 1). Quantiferon gold testing was positive, and the patient was started on empiric anti-TB therapy for concern for disseminated TB. Shortly after admission, the patient had two large episodes of hematochezia with a 2.5 g drop in his hemoglobin and resultant hemodynamic instability requiring vasopressor support in the ICU. Following stabilization, colonoscopy revealed heaped-up margins of erythematous mucosa in the ascending colon and cecum (Figure 2). Biopsies showed granulomatous colitis with mycobacterial organisms positive for acid-fast bacilli, confirming GI TB. The patient was continued on anti-TB and antiretroviral therapy and was discharged in stable condition.
Discussion: Although TB is prominent globally, GI TB remains a rare occurrence. While the classic presentation of GI TB is non-specific abdominal pain without significant bleeding, there are some scattered case reports of severe bleeding. There are even fewer instances in the literature where major GI TB bleed is seen in patients with HIV/AIDS. It is plausible to consider that our patient's degree of immunosuppression may have predisposed him to more severe infection and bleed. GI TB is generally responsive to standard anti-TB therapy, and in the absence of life-threatening bleed, usually does not confer worse mortality rates. This case highlights the importance of routine TB and HIV screening in vulnerable populations and highlights a quite rare cause of life-threatening GI bleed.

Figure: Figure 1 – CT Abdomen showing cecal wall thickening and abdominal lymphadenopathy
Disclosures:
Kevan Josloff indicated no relevant financial relationships.
Hamzah Shariff indicated no relevant financial relationships.
Kathleen Spritzer indicated no relevant financial relationships.
Wei Jiang indicated no relevant financial relationships.
Anna Chen indicated no relevant financial relationships.
Leo Katz indicated no relevant financial relationships.
Kevan Josloff, MD, MPH1, Hamzah Shariff, MD1, Kathleen Spritzer, BS2, Wei Jiang, MD1, Anna Chen, MD1, Leo Katz, MD, FACG1. P1327 - Gastrointestinal Tuberculosis Presenting as a Massive Lower GI Bleed in a Patient With Newly Diagnosed HIV/AIDS, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Thomas Jefferson University Hospital, Philadelphia, PA; 2Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA
Introduction: Gastrointestinal Tuberculosis (GI TB) is an uncommon sequela of TB, occurring in approximately 3% of all TB cases worldwide. In the United States, many cases are seen in migrant populations or in immunocompromised individuals. The classic presentation of GI TB is non-specific abdominal pain not typically associated with significant bleeding. We present a case of GI TB complicated by life-threatening lower GI bleed requiring vasopressor support in a patient with newly diagnosed HIV/AIDS.
Case Description/
Methods: A 25-year-old male who recently immigrated to the Unites States from Peru presented with several weeks of abdominal pain and scant bright red blood per rectum. On presentation his hemoglobin was 7.6, and he was also found to have a new diagnosis of HIV with viral load 2.87 million copies and CD4+ count of 128. CT abdomen pelvis showed circumferential wall thickening of the cecum and proximal ascending colon, with extensive necrotizing lymphadenopathy throughout the mesentery (Figure 1). Quantiferon gold testing was positive, and the patient was started on empiric anti-TB therapy for concern for disseminated TB. Shortly after admission, the patient had two large episodes of hematochezia with a 2.5 g drop in his hemoglobin and resultant hemodynamic instability requiring vasopressor support in the ICU. Following stabilization, colonoscopy revealed heaped-up margins of erythematous mucosa in the ascending colon and cecum (Figure 2). Biopsies showed granulomatous colitis with mycobacterial organisms positive for acid-fast bacilli, confirming GI TB. The patient was continued on anti-TB and antiretroviral therapy and was discharged in stable condition.
Discussion: Although TB is prominent globally, GI TB remains a rare occurrence. While the classic presentation of GI TB is non-specific abdominal pain without significant bleeding, there are some scattered case reports of severe bleeding. There are even fewer instances in the literature where major GI TB bleed is seen in patients with HIV/AIDS. It is plausible to consider that our patient's degree of immunosuppression may have predisposed him to more severe infection and bleed. GI TB is generally responsive to standard anti-TB therapy, and in the absence of life-threatening bleed, usually does not confer worse mortality rates. This case highlights the importance of routine TB and HIV screening in vulnerable populations and highlights a quite rare cause of life-threatening GI bleed.

Figure: Figure 1 – CT Abdomen showing cecal wall thickening and abdominal lymphadenopathy
Disclosures:
Kevan Josloff indicated no relevant financial relationships.
Hamzah Shariff indicated no relevant financial relationships.
Kathleen Spritzer indicated no relevant financial relationships.
Wei Jiang indicated no relevant financial relationships.
Anna Chen indicated no relevant financial relationships.
Leo Katz indicated no relevant financial relationships.
Kevan Josloff, MD, MPH1, Hamzah Shariff, MD1, Kathleen Spritzer, BS2, Wei Jiang, MD1, Anna Chen, MD1, Leo Katz, MD, FACG1. P1327 - Gastrointestinal Tuberculosis Presenting as a Massive Lower GI Bleed in a Patient With Newly Diagnosed HIV/AIDS, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
