Sunday Poster Session
Category: Infections and Microbiome
P1325 - Invasive Intestinal Spirochetosis Mimicking IBD: A Rare Etiology of Chronic Abdominal Pain and Watery Diarrhea in a Patient With HIV
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- AW
Abdul Wasay, MD
University of Tennessee
Knoxville, TN
Presenting Author(s)
Abdul Wasay, MD, Nasir Notta, MD, Thomas Young, MD
University of Tennessee, Knoxville, TN
Introduction: Intestinal spirochetosis (IS) is a rare disorder defined by the presence of spirochetes on the colonic epithelial surface. The debate over whether IS a commensal or pathogenic process continues, primarily due rarity of cases. However, recent evidence supports the idea that IS can be invasive and highly pathogenic in both immunocompromised and immunocompetent individuals. Herein we report a case of chronic abdominal pain and watery diarrhea in a patient with HIV, where the presence of spirochetes was confirmed in colonic biopsy specimens.
Case Description/
Methods: A 57-year-old homosexual male presented with a two-month history of watery diarrhea and a skin rash. He reported a Bristol stool scale rating of 6-7, along with a painless, non-itchy rash located on his bilateral upper extremities, chest, and trunk. Additionally, he mentioned experiencing right lower abdominal pain for many years. The patient is HIV positive, with a recent CD4 count more than 100, a positive RPR, and a recent treatment history for gonorrhea. He denied any fever, night sweats, or significant weight loss. He was prescribed initially clindamycin and prednisone without significant improvement in his symptoms. He underwent skin punch biopsy, which showed a significant infiltration of plasma cells.
Decision was made perform a colonoscopy, which identified two aphthous ulcerations with friable mucosa and exudate in colon. Biopsies were obtained, and immunohistochemical staining was performed, which confirmed the presence of spirochetes. Subsequently, the patient received treatment with metronidazole, leading to significant improvement in his rash and diarrhea.
Discussion: Review of the literature indicates that IS is a cause of chronic diarrhea in men who have sex with men, with 92% of patients having reported HIV infection risk factors. Most of these patients are not severely immunosuppressed, as 70% have CD4 lymphocyte counts above 200/microL. Colonoscopy results often show normal mucosal appearance. Immunohistochemistry is effective in diagnosis of IS as it highlights spiral organisms within mucus or crypts that are invisible in routine histology. When intestinal spirochetosis is diagnosed as the sole intestinal pathology in symptomatic individuals, it is essential to treat the infection with metronidazole and to perform a follow-up colonoscopy and biopsy for those with persistent symptoms.
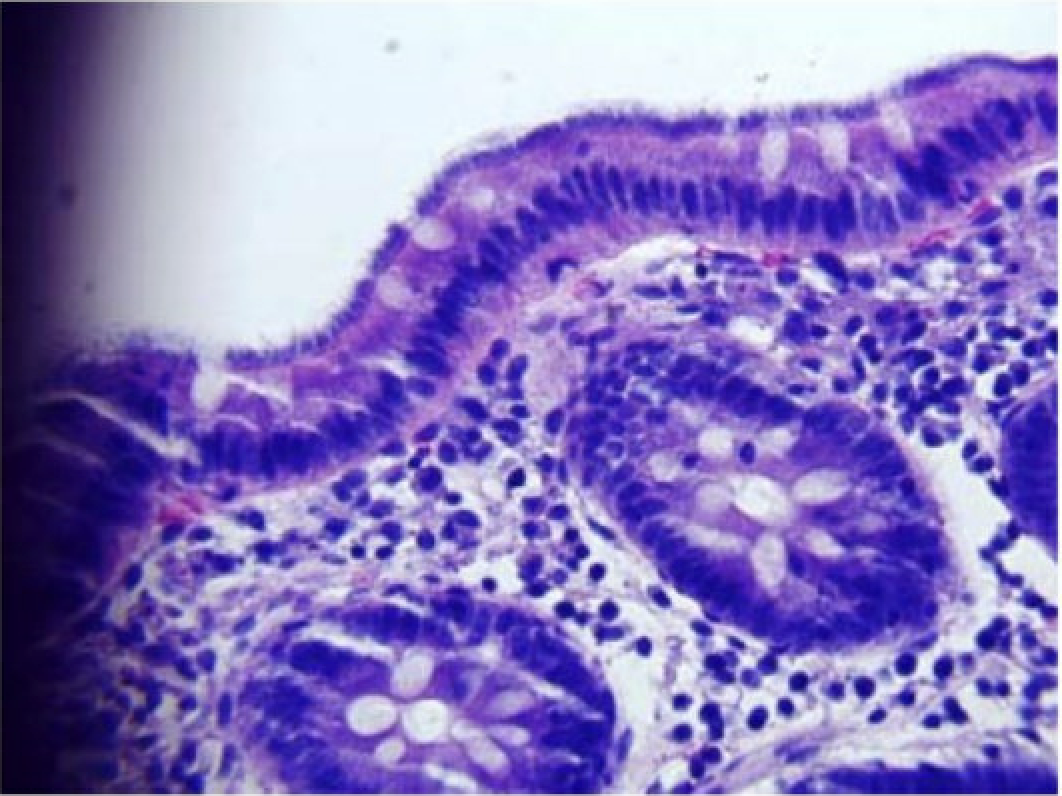
Figure: Intestinal spirochetosis seen on biopsy sample through gross microscopic evaluation.
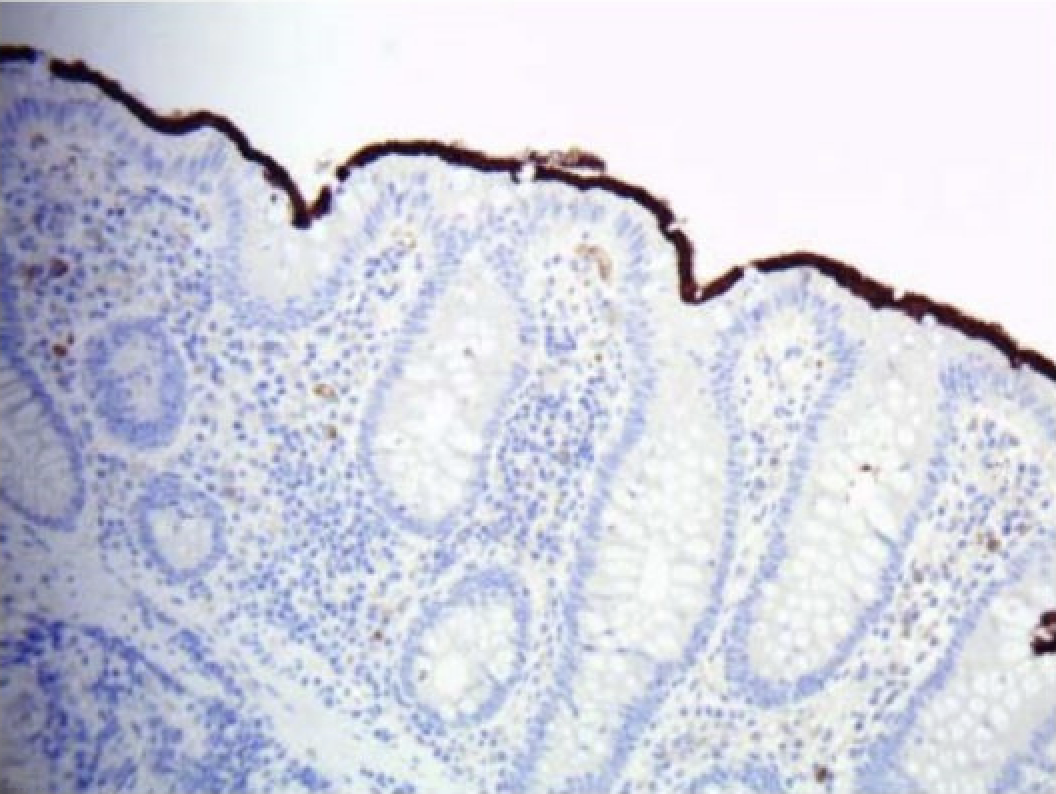
Figure: Intestinal spirochetosis confirmed from biopsy sample with immunochemistry stain.
Disclosures:
Abdul Wasay indicated no relevant financial relationships.
Nasir Notta indicated no relevant financial relationships.
Thomas Young indicated no relevant financial relationships.
Abdul Wasay, MD, Nasir Notta, MD, Thomas Young, MD. P1325 - Invasive Intestinal Spirochetosis Mimicking IBD: A Rare Etiology of Chronic Abdominal Pain and Watery Diarrhea in a Patient With HIV, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Tennessee, Knoxville, TN
Introduction: Intestinal spirochetosis (IS) is a rare disorder defined by the presence of spirochetes on the colonic epithelial surface. The debate over whether IS a commensal or pathogenic process continues, primarily due rarity of cases. However, recent evidence supports the idea that IS can be invasive and highly pathogenic in both immunocompromised and immunocompetent individuals. Herein we report a case of chronic abdominal pain and watery diarrhea in a patient with HIV, where the presence of spirochetes was confirmed in colonic biopsy specimens.
Case Description/
Methods: A 57-year-old homosexual male presented with a two-month history of watery diarrhea and a skin rash. He reported a Bristol stool scale rating of 6-7, along with a painless, non-itchy rash located on his bilateral upper extremities, chest, and trunk. Additionally, he mentioned experiencing right lower abdominal pain for many years. The patient is HIV positive, with a recent CD4 count more than 100, a positive RPR, and a recent treatment history for gonorrhea. He denied any fever, night sweats, or significant weight loss. He was prescribed initially clindamycin and prednisone without significant improvement in his symptoms. He underwent skin punch biopsy, which showed a significant infiltration of plasma cells.
Decision was made perform a colonoscopy, which identified two aphthous ulcerations with friable mucosa and exudate in colon. Biopsies were obtained, and immunohistochemical staining was performed, which confirmed the presence of spirochetes. Subsequently, the patient received treatment with metronidazole, leading to significant improvement in his rash and diarrhea.
Discussion: Review of the literature indicates that IS is a cause of chronic diarrhea in men who have sex with men, with 92% of patients having reported HIV infection risk factors. Most of these patients are not severely immunosuppressed, as 70% have CD4 lymphocyte counts above 200/microL. Colonoscopy results often show normal mucosal appearance. Immunohistochemistry is effective in diagnosis of IS as it highlights spiral organisms within mucus or crypts that are invisible in routine histology. When intestinal spirochetosis is diagnosed as the sole intestinal pathology in symptomatic individuals, it is essential to treat the infection with metronidazole and to perform a follow-up colonoscopy and biopsy for those with persistent symptoms.
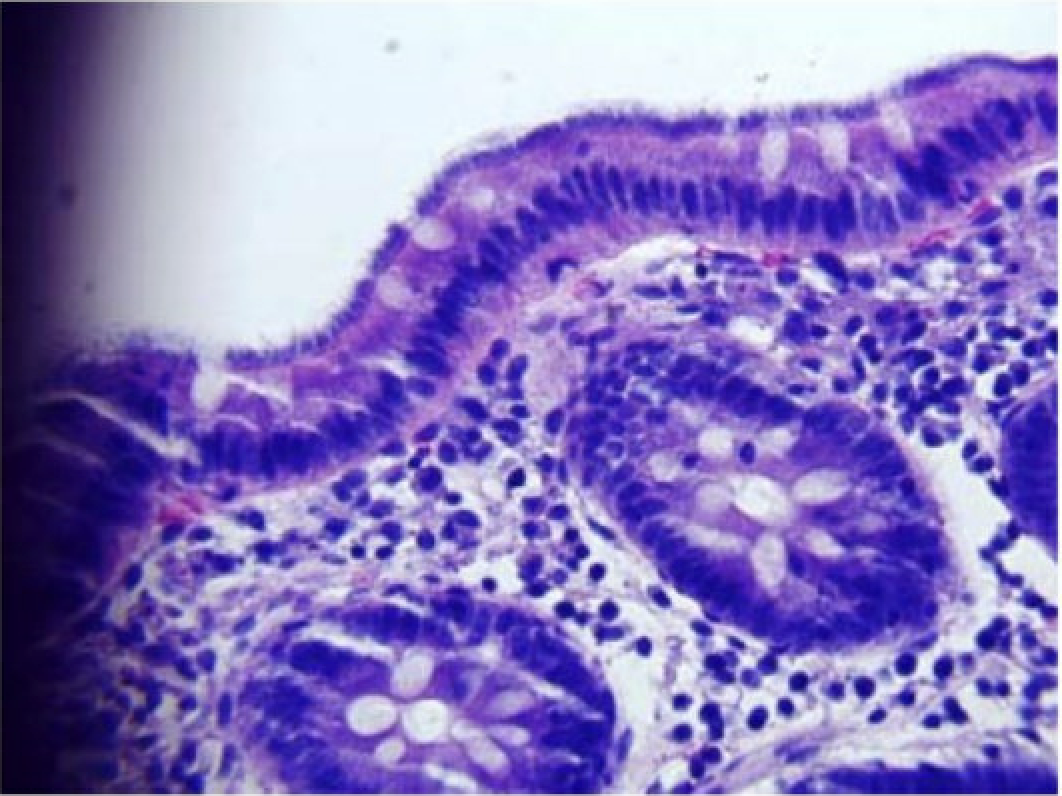
Figure: Intestinal spirochetosis seen on biopsy sample through gross microscopic evaluation.
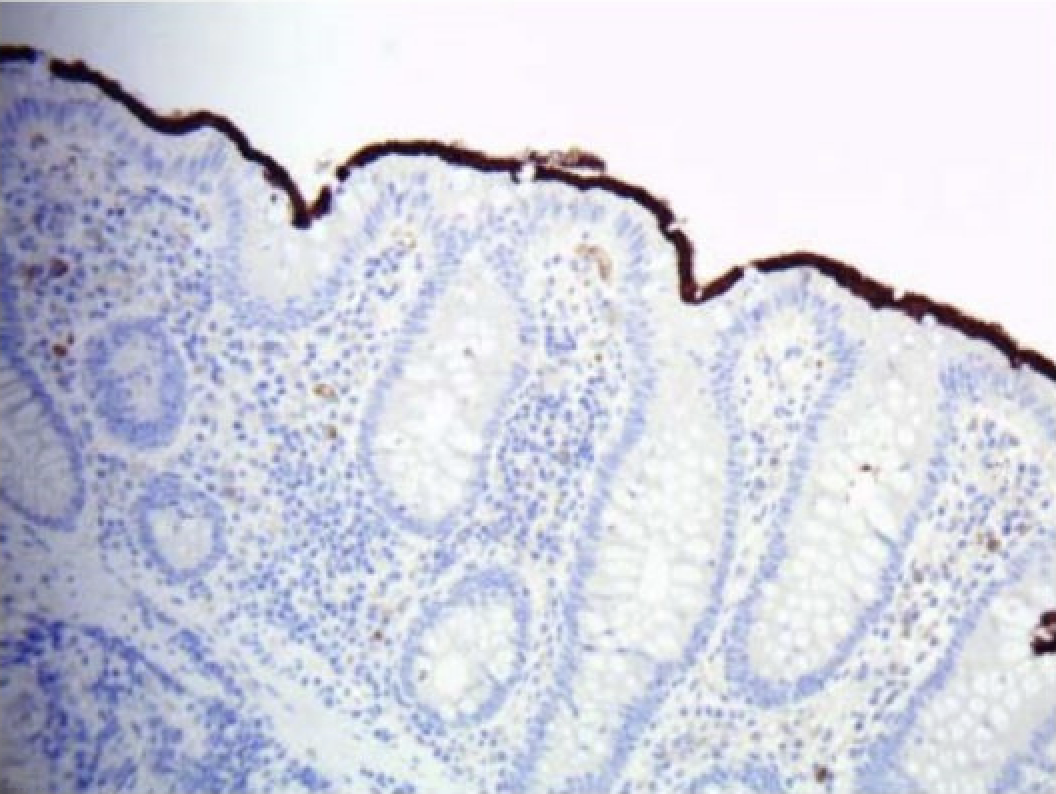
Figure: Intestinal spirochetosis confirmed from biopsy sample with immunochemistry stain.
Disclosures:
Abdul Wasay indicated no relevant financial relationships.
Nasir Notta indicated no relevant financial relationships.
Thomas Young indicated no relevant financial relationships.
Abdul Wasay, MD, Nasir Notta, MD, Thomas Young, MD. P1325 - Invasive Intestinal Spirochetosis Mimicking IBD: A Rare Etiology of Chronic Abdominal Pain and Watery Diarrhea in a Patient With HIV, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
