Sunday Poster Session
Category: Interventional Endoscopy
P1388 - Short Term Outcomes of Endoscopic Submucosal Dissection (ESD) vs Endoscopic Mucosal Resection (EMR) in Patients With Cirrhosis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- AC
Arjun Chatterjee, MD (he/him/his)
Cleveland Clinic Foundation
Cleveland, OH
Presenting Author(s)
Andrew Ford, MD1, Arjun Chatterjee, MD2, Ridhima Kaul, MD2, Renan Prado, MD2, Rajat Garg, MD2, Prabhleen Chahal, MD, FACG3, Matheus Franco, MD, MSc, PhD3
1Case Western Reserve University / MetroHealth, Cleveland, OH; 2Cleveland Clinic Foundation, Cleveland, OH; 3University of Texas Health San Antonio, San Antonio, TX
Introduction: Endoscopic Submucosal Dissection (ESD) and Endoscopic Mucosal Resection (EMR) are endoscopic techniques utilized for managing gastrointestinal lesions. In cirrhotic patients, procedural safety is a significant concern. This study compares short-term outcomes between ESD and EMR in cirrhotic patients using real-world data from a global health research network.
Methods: We used the TriNetX database, a global federated network with data from numerous healthcare organizations. We identified cirrhotic patients with ESD and EMR using CPT and ICD-10 codes and excluded those with same day endoscopic management of gastrointestinal bleeding (GIB). We identified 391 patients in ESD cohort and 1279 patients in the EMR cohort. We then performed 1:1 propensity matching for demographics (age, sex, race, and ethnicity); co-morbidities (diabetes, heart failure, COPD, and chronic kidney disease); MELD labs; Medications use (anticoagulants, anti-platelets, beta blockers use). Table 1
Co-primary outcomes included perforation, ICU Transfer, GIB, blood transfusions.
Odds ratios (ORs) with 95% confidence intervals (CIs) were obtained for all outcomes save for mortality, for which Cox regression analysis was done to obtain hazard ratio (HR) at two years.
Results: After propensity score matching, each group contained 286 patients on both groups with a median 30 days follow up. The matched cohorts were predominantly white and male. Both groups had similar number of patients with medical co-morbidities and had similar labs. Table 1.
Perforation occurred in 0% of patients in the ESD cohort compared to 3.5% in the EMR cohort (risk difference: -0.035, p = 0.001). There were no ICU transfers in either cohort. GIB occurred during the 30 day follow up in 3.5% of patients in both cohorts (p = 1). Blood transfusion was required in 0% of ESD patients versus 3.5% in the EMR group (risk difference: -0.035, p = 0.001).
Discussion: In cirrhotic patients, ESD appears to have a comparable or slightly safer short-term safety profile compared to EMR, with significantly fewer cases of perforation and transfusion. These findings support the consideration of ESD as a safe therapeutic option in appropriately selected cirrhotic patients.
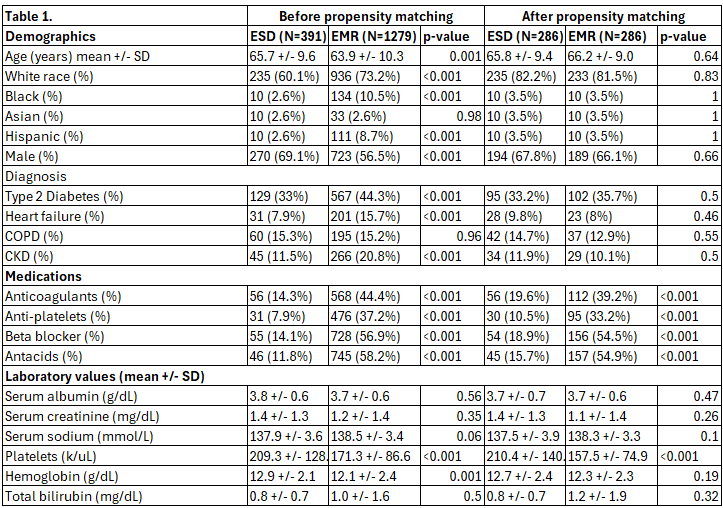
Figure: Table1. Cohort descriptive analysis before and after propensity match
Disclosures:
Andrew Ford indicated no relevant financial relationships.
Arjun Chatterjee indicated no relevant financial relationships.
Ridhima Kaul indicated no relevant financial relationships.
Renan Prado indicated no relevant financial relationships.
Rajat Garg indicated no relevant financial relationships.
Prabhleen Chahal indicated no relevant financial relationships.
Matheus Franco indicated no relevant financial relationships.
Andrew Ford, MD1, Arjun Chatterjee, MD2, Ridhima Kaul, MD2, Renan Prado, MD2, Rajat Garg, MD2, Prabhleen Chahal, MD, FACG3, Matheus Franco, MD, MSc, PhD3. P1388 - Short Term Outcomes of Endoscopic Submucosal Dissection (ESD) vs Endoscopic Mucosal Resection (EMR) in Patients With Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Case Western Reserve University / MetroHealth, Cleveland, OH; 2Cleveland Clinic Foundation, Cleveland, OH; 3University of Texas Health San Antonio, San Antonio, TX
Introduction: Endoscopic Submucosal Dissection (ESD) and Endoscopic Mucosal Resection (EMR) are endoscopic techniques utilized for managing gastrointestinal lesions. In cirrhotic patients, procedural safety is a significant concern. This study compares short-term outcomes between ESD and EMR in cirrhotic patients using real-world data from a global health research network.
Methods: We used the TriNetX database, a global federated network with data from numerous healthcare organizations. We identified cirrhotic patients with ESD and EMR using CPT and ICD-10 codes and excluded those with same day endoscopic management of gastrointestinal bleeding (GIB). We identified 391 patients in ESD cohort and 1279 patients in the EMR cohort. We then performed 1:1 propensity matching for demographics (age, sex, race, and ethnicity); co-morbidities (diabetes, heart failure, COPD, and chronic kidney disease); MELD labs; Medications use (anticoagulants, anti-platelets, beta blockers use). Table 1
Co-primary outcomes included perforation, ICU Transfer, GIB, blood transfusions.
Odds ratios (ORs) with 95% confidence intervals (CIs) were obtained for all outcomes save for mortality, for which Cox regression analysis was done to obtain hazard ratio (HR) at two years.
Results: After propensity score matching, each group contained 286 patients on both groups with a median 30 days follow up. The matched cohorts were predominantly white and male. Both groups had similar number of patients with medical co-morbidities and had similar labs. Table 1.
Perforation occurred in 0% of patients in the ESD cohort compared to 3.5% in the EMR cohort (risk difference: -0.035, p = 0.001). There were no ICU transfers in either cohort. GIB occurred during the 30 day follow up in 3.5% of patients in both cohorts (p = 1). Blood transfusion was required in 0% of ESD patients versus 3.5% in the EMR group (risk difference: -0.035, p = 0.001).
Discussion: In cirrhotic patients, ESD appears to have a comparable or slightly safer short-term safety profile compared to EMR, with significantly fewer cases of perforation and transfusion. These findings support the consideration of ESD as a safe therapeutic option in appropriately selected cirrhotic patients.
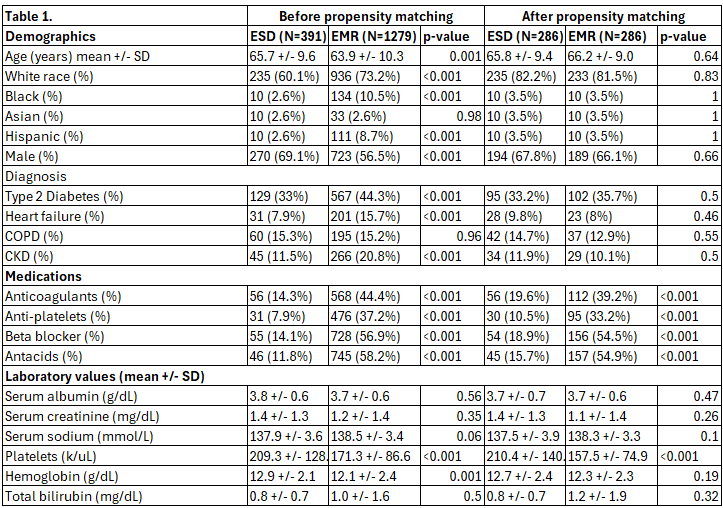
Figure: Table1. Cohort descriptive analysis before and after propensity match
Disclosures:
Andrew Ford indicated no relevant financial relationships.
Arjun Chatterjee indicated no relevant financial relationships.
Ridhima Kaul indicated no relevant financial relationships.
Renan Prado indicated no relevant financial relationships.
Rajat Garg indicated no relevant financial relationships.
Prabhleen Chahal indicated no relevant financial relationships.
Matheus Franco indicated no relevant financial relationships.
Andrew Ford, MD1, Arjun Chatterjee, MD2, Ridhima Kaul, MD2, Renan Prado, MD2, Rajat Garg, MD2, Prabhleen Chahal, MD, FACG3, Matheus Franco, MD, MSc, PhD3. P1388 - Short Term Outcomes of Endoscopic Submucosal Dissection (ESD) vs Endoscopic Mucosal Resection (EMR) in Patients With Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
