Sunday Poster Session
Category: Interventional Endoscopy
P1385 - Rigidizing the Path to Precision: A Randomized Controlled Trial Evaluating a Novel Overtube for Colonic Endoscopic Submucosal Dissection: Feasibility, Safety, and Efficacy Outcomes
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Tara Keihanian, MD, MPH
Baylor College of Medicine
Houston, TX
Presenting Author(s)
Award: ACG Outstanding Research Award in the Interventional Endoscopy Category
Award: ACG Presidential Poster Award
Tara Keihanian, MD, MPH, Fares Ayoub, MD, Mai Khalaf, MD, Ghena Khasawneh, MD, Haydee Rochits Cueto, MD, MPH, Salmaan A.. Jawaid, MD, Mohamed O.. Othman, MD
Baylor College of Medicine, Houston, TX
Introduction: Colonic endoscopic submucosal dissection (ESD) could be challenging due to the tortuous and redundant anatomy of the colon, which can compromise scope maneuverability and stability. The use of a rigidizing overtube may improve scope stability and enhance procedural efficiency. This study assesses the feasibility, safety, and efficacy of a novel rigidizing overtube in colonic ESD.
Methods: This is a single-center, randomized, controlled trial assessing the efficacy of a rigidizing overtube in colonic ESD. Between 2023 and 2024, patients referred for advanced polyp resection were randomized (1:1) to either conventional ESD (C) or overtube-assisted ESD (O), performed by three endoscopists with varying levels of expertise. Exclusion criteria included polyps located in the ileocecal valve or appendix, or failure to meet inclusion criteria (granular lateral spreading tumors [GLST] ≥3 cm or non-GLST ≥20 mm). The primary outcome was procedure speed; secondary outcomes included en bloc and R0 resection rates, dissection and closure speeds, and adverse events.
Results: Overall, 66 randomized patients were included. The rigidizing overtube significantly improved scope stability (O: 63.6% vs. C: 24.2%, p = 0.003) and retroflexion capability (O: 69.7% vs. C: 51.5%, p = 0.028). In contrast, the C group required more frequent use of a scope stiffener (51.5% vs. 15.2%, p = 0.006) and manual abdominal pressure (33.3% vs. 12.1%, p = 0.038). The dissection speed was numerically greater in the O group (18.33 ± 14.19 mm²/min) compared to the C group (16.78 ± 8.59 mm²/min), though not statistically significant (p = 0.277). En bloc resection rates (C: 97%, O: 93.9%, p = 1.0) and R0 resection rates (C: 87.9%, O: 84.8%, p = 1.0) were similar in the intention-to-treat analysis. Four patients crossed from the C to the O group, with three completed en bloc. One patient crossed from the O to the C group and was resected piecemeal. Per-protocol analysis did not show significant differences in dissection speed (p = 0.956), closure speed (p = 0.432), or R0 resection rates (C: 90% vs. O: 83.3%, p = 0.494). Rates of intra- and post-procedural adverse events were comparable across both groups.
Discussion: The use of a novel rigidizing overtube in colonic ESD significantly improved scope stability and retroflexion, while reducing reliance on adjunctive maneuvers such as stiffeners and manual compression. The device offers procedural advantages that may enhance procedural efficiency in selected cases.
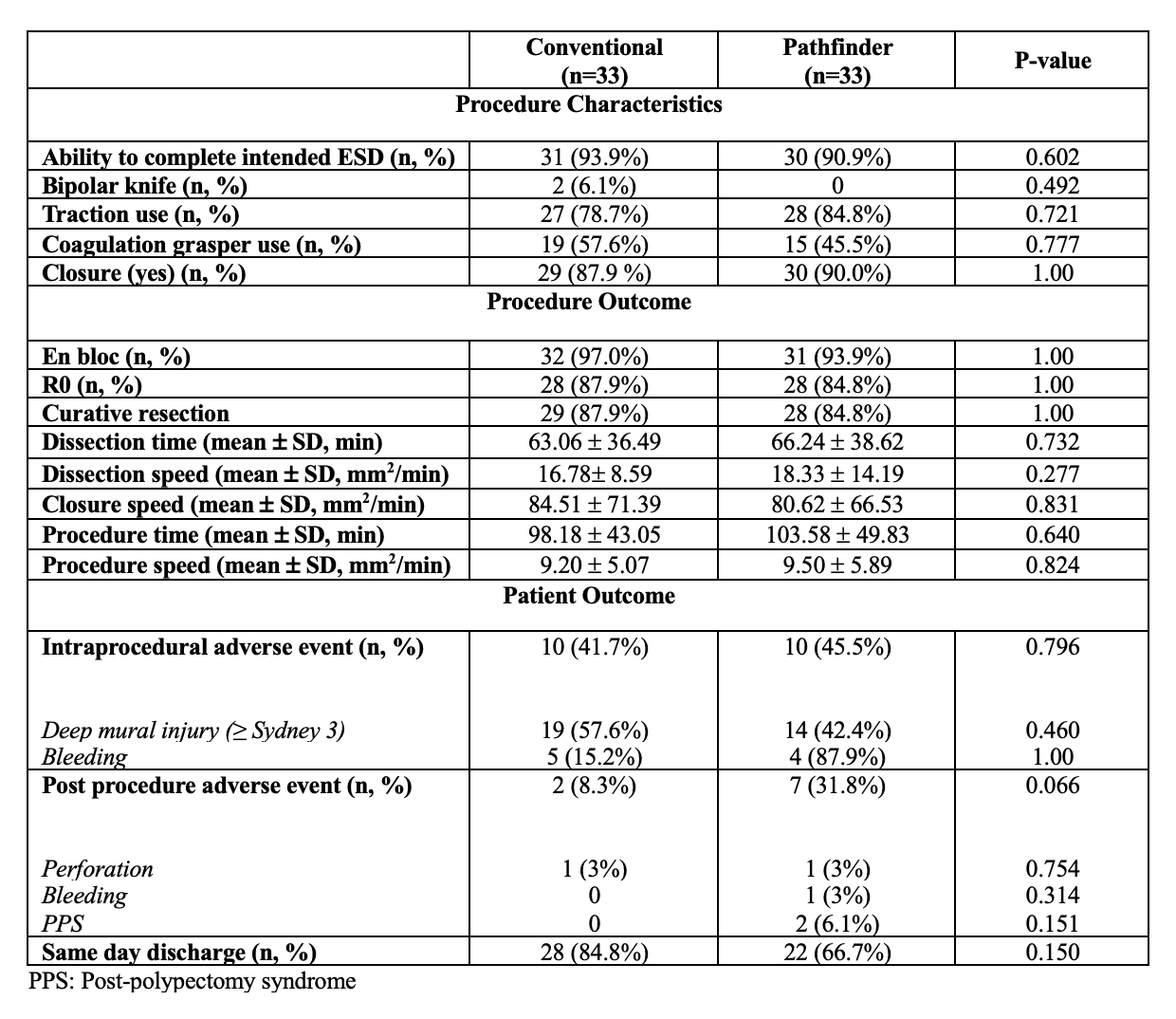
Figure: Table 1- Patient demographics, polyp characteristics, and Scope Stabilization (Intention-to-treat analysis)
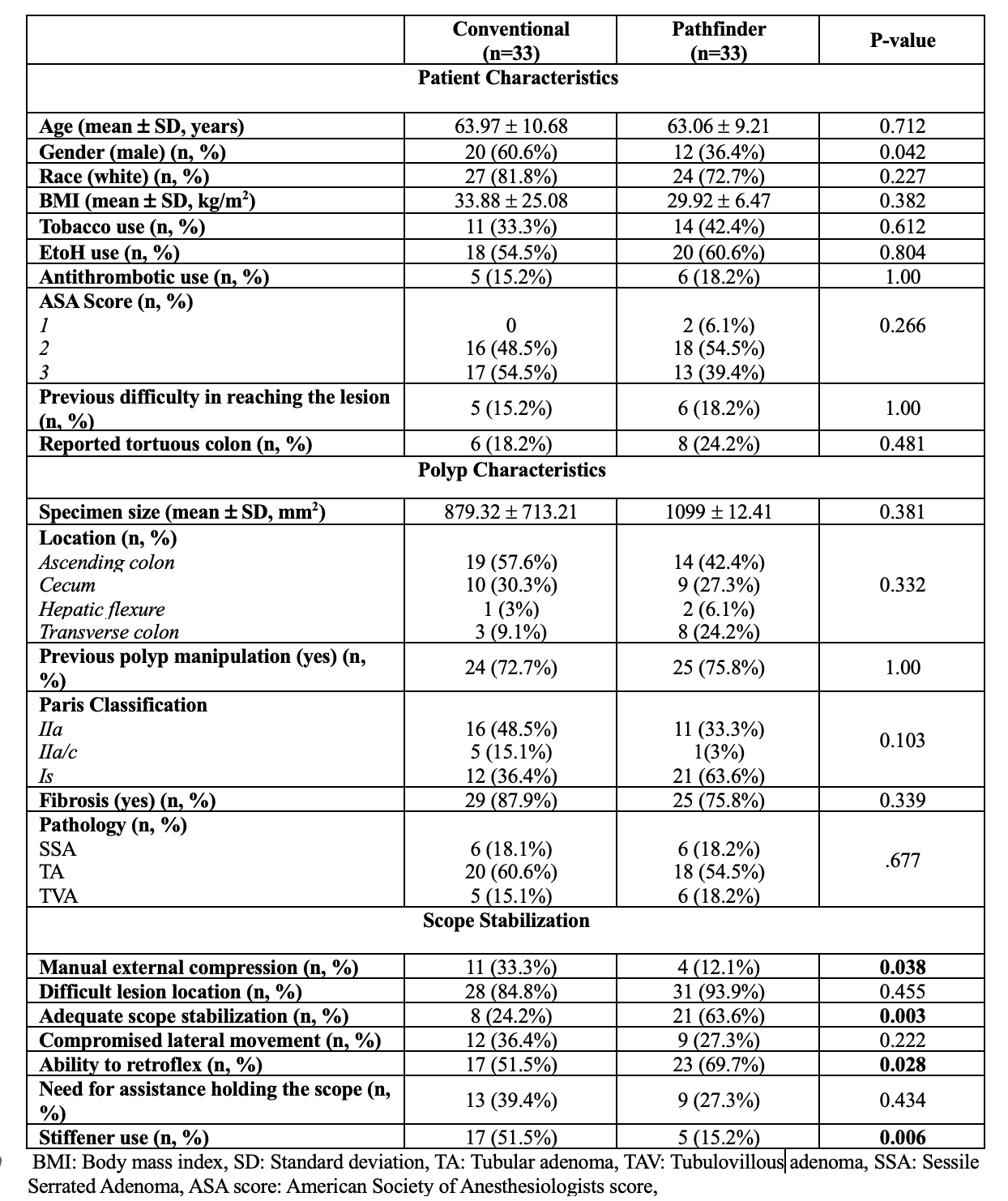
Figure: Table 2- Procedure characteristics, procedure outcome, and patient outcome (intention-to-treat analysis)
Disclosures:
Tara Keihanian: Boston Scientific – Consultant. ConMed – Consultant. Microtech – Consultant.
Fares Ayoub indicated no relevant financial relationships.
Mai Khalaf indicated no relevant financial relationships.
Ghena Khasawneh indicated no relevant financial relationships.
Haydee Rochits Cueto indicated no relevant financial relationships.
Salmaan Jawaid: 3D Matrix – Consultant. Boston Scientific – Consultant. ConMed – Consultant. Creo Medical – Consultant. Microtech – Consultant.
Mohamed Othman: Abbvie – Consultant. Boston Scientific – Consultant. ConMed – Consultant. Microtech – Consultant.
Tara Keihanian, MD, MPH, Fares Ayoub, MD, Mai Khalaf, MD, Ghena Khasawneh, MD, Haydee Rochits Cueto, MD, MPH, Salmaan A.. Jawaid, MD, Mohamed O.. Othman, MD. P1385 - Rigidizing the Path to Precision: A Randomized Controlled Trial Evaluating a Novel Overtube for Colonic Endoscopic Submucosal Dissection: Feasibility, Safety, and Efficacy Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Award: ACG Presidential Poster Award
Tara Keihanian, MD, MPH, Fares Ayoub, MD, Mai Khalaf, MD, Ghena Khasawneh, MD, Haydee Rochits Cueto, MD, MPH, Salmaan A.. Jawaid, MD, Mohamed O.. Othman, MD
Baylor College of Medicine, Houston, TX
Introduction: Colonic endoscopic submucosal dissection (ESD) could be challenging due to the tortuous and redundant anatomy of the colon, which can compromise scope maneuverability and stability. The use of a rigidizing overtube may improve scope stability and enhance procedural efficiency. This study assesses the feasibility, safety, and efficacy of a novel rigidizing overtube in colonic ESD.
Methods: This is a single-center, randomized, controlled trial assessing the efficacy of a rigidizing overtube in colonic ESD. Between 2023 and 2024, patients referred for advanced polyp resection were randomized (1:1) to either conventional ESD (C) or overtube-assisted ESD (O), performed by three endoscopists with varying levels of expertise. Exclusion criteria included polyps located in the ileocecal valve or appendix, or failure to meet inclusion criteria (granular lateral spreading tumors [GLST] ≥3 cm or non-GLST ≥20 mm). The primary outcome was procedure speed; secondary outcomes included en bloc and R0 resection rates, dissection and closure speeds, and adverse events.
Results: Overall, 66 randomized patients were included. The rigidizing overtube significantly improved scope stability (O: 63.6% vs. C: 24.2%, p = 0.003) and retroflexion capability (O: 69.7% vs. C: 51.5%, p = 0.028). In contrast, the C group required more frequent use of a scope stiffener (51.5% vs. 15.2%, p = 0.006) and manual abdominal pressure (33.3% vs. 12.1%, p = 0.038). The dissection speed was numerically greater in the O group (18.33 ± 14.19 mm²/min) compared to the C group (16.78 ± 8.59 mm²/min), though not statistically significant (p = 0.277). En bloc resection rates (C: 97%, O: 93.9%, p = 1.0) and R0 resection rates (C: 87.9%, O: 84.8%, p = 1.0) were similar in the intention-to-treat analysis. Four patients crossed from the C to the O group, with three completed en bloc. One patient crossed from the O to the C group and was resected piecemeal. Per-protocol analysis did not show significant differences in dissection speed (p = 0.956), closure speed (p = 0.432), or R0 resection rates (C: 90% vs. O: 83.3%, p = 0.494). Rates of intra- and post-procedural adverse events were comparable across both groups.
Discussion: The use of a novel rigidizing overtube in colonic ESD significantly improved scope stability and retroflexion, while reducing reliance on adjunctive maneuvers such as stiffeners and manual compression. The device offers procedural advantages that may enhance procedural efficiency in selected cases.
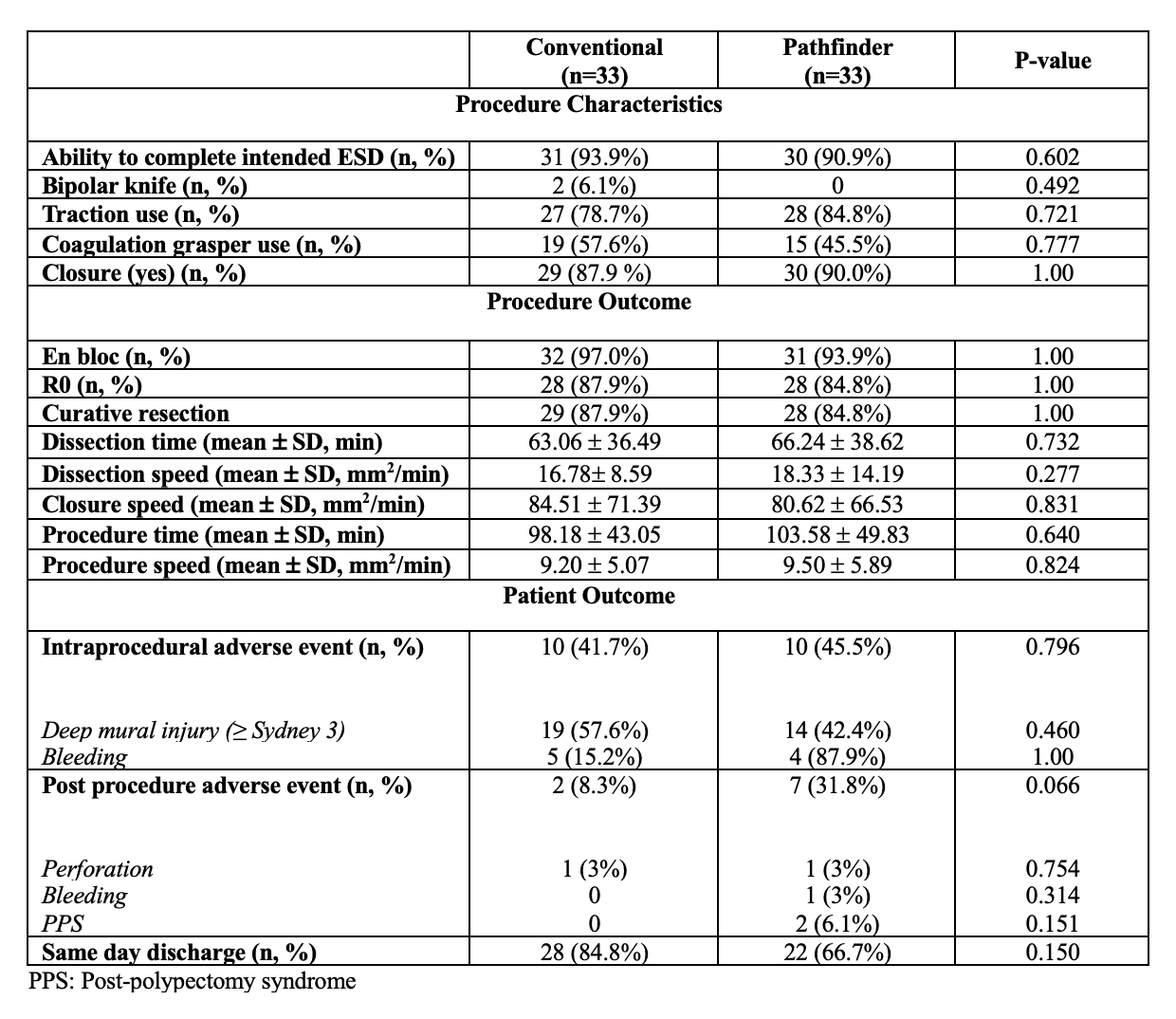
Figure: Table 1- Patient demographics, polyp characteristics, and Scope Stabilization (Intention-to-treat analysis)
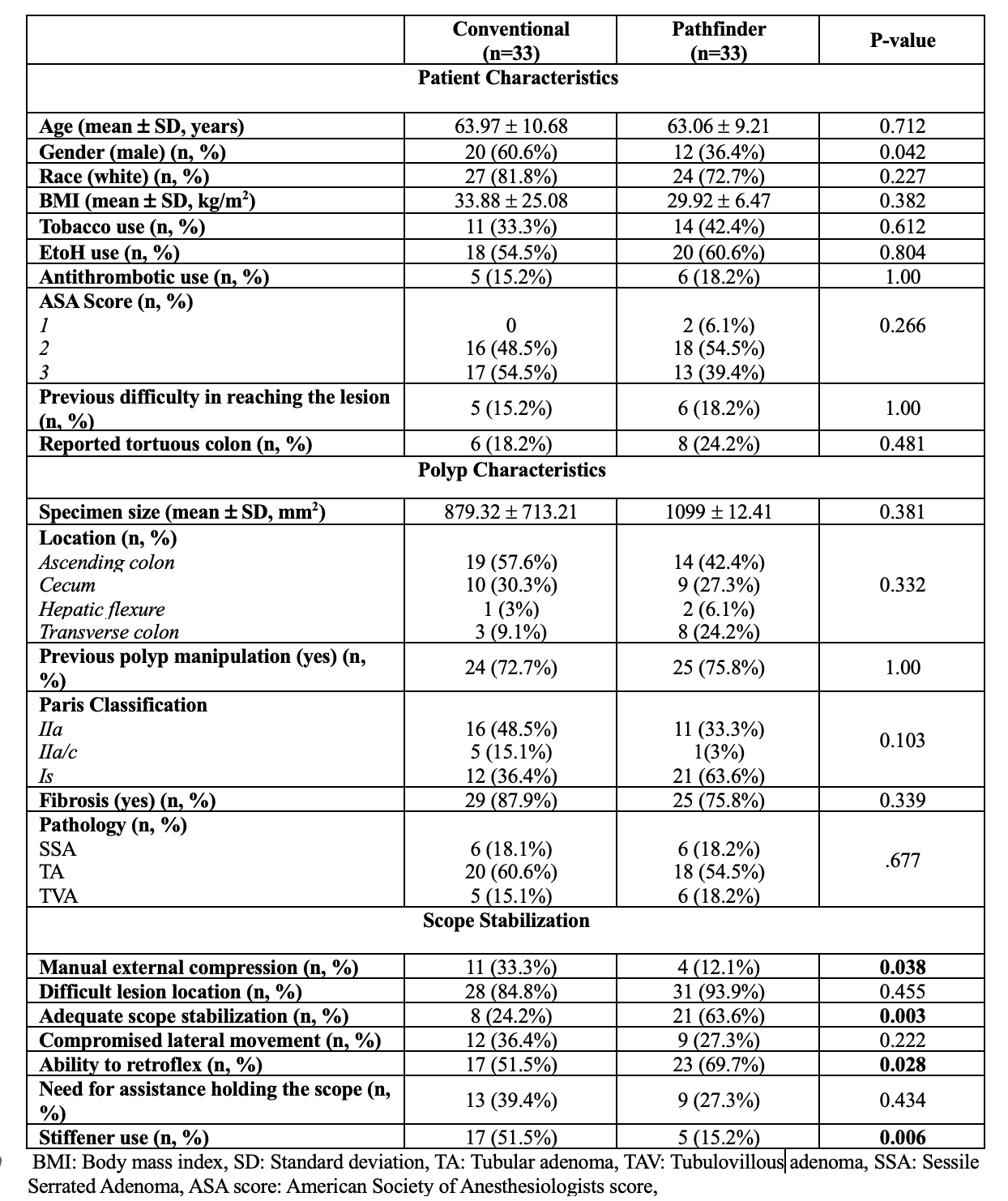
Figure: Table 2- Procedure characteristics, procedure outcome, and patient outcome (intention-to-treat analysis)
Disclosures:
Tara Keihanian: Boston Scientific – Consultant. ConMed – Consultant. Microtech – Consultant.
Fares Ayoub indicated no relevant financial relationships.
Mai Khalaf indicated no relevant financial relationships.
Ghena Khasawneh indicated no relevant financial relationships.
Haydee Rochits Cueto indicated no relevant financial relationships.
Salmaan Jawaid: 3D Matrix – Consultant. Boston Scientific – Consultant. ConMed – Consultant. Creo Medical – Consultant. Microtech – Consultant.
Mohamed Othman: Abbvie – Consultant. Boston Scientific – Consultant. ConMed – Consultant. Microtech – Consultant.
Tara Keihanian, MD, MPH, Fares Ayoub, MD, Mai Khalaf, MD, Ghena Khasawneh, MD, Haydee Rochits Cueto, MD, MPH, Salmaan A.. Jawaid, MD, Mohamed O.. Othman, MD. P1385 - Rigidizing the Path to Precision: A Randomized Controlled Trial Evaluating a Novel Overtube for Colonic Endoscopic Submucosal Dissection: Feasibility, Safety, and Efficacy Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.


