Sunday Poster Session
Category: Interventional Endoscopy
P1471 - When Guidelines Fall Short: Necrotizing Pancreatitis After Gastric Bypass Sparks Debate
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Karan J. Yagnik, MD (he/him/his)
Monmouth Medical Center, Robert Wood Johnson Medical School of Rutgers University
Long Branch, NJ
Presenting Author(s)
Karan J.. Yagnik, MD1, Suryansh Atreya, MD1, FNU Payal, MD1, Mitsu Patel, BA2, Jilliane Unas, MD1, Nishtha Nigam, MD1, Anirudh Kulkarni, BS2, Dhramesh Kaswala, MD1, Anish V. Patel, MD2, Wael Ghali, MD1
1Monmouth Medical Center, Robert Wood Johnson Medical School of Rutgers University, Long Branch, NJ; 2Robert Wood Johnson Medical School, Rutgers University, New Brunswick, NJ
Introduction: We present a case of post-Roux-en-Y gastric bypass (RYGB) acute pancreatitis rapidly progressing to necrosis, ascites, sepsis, and respiratory failure, requiring prolonged hospitalization and complex interventions due to altered anatomy.
Case Description/
Methods: A female in her early 50s, with RYGB performed 2.5 months prior, presented with acute abdominal pain, nausea, and vomiting. Labs revealed markedly elevated amylase, lipase. Initial CT abdomen/pelvis showed acute pancreatitis without gallstones or biliary dilation. She was admitted for supportive care. Overnight, she developed worsening abdominal distension, obstipation, guarding, hypoactive bowel sounds, and rising hematocrit with elevated bladder pressure. Repeat CT showed necrotizing pancreatitis, large loculated ascites and bilateral pleural effusions. Bedside ultrasound revealed cholelithiasis. She was intubated for respiratory distress and transferred to a tertiary center.
At the tertiary center, EUS was performed, but an EDGE procedure was deferred to preserve pancreatic drainage pathways. Later, EUS-guided cystogastrostomy was attempted but failed due to solid collection; the stent was removed and closed with an over-the-scope clip. The patient developed sepsis, requiring ICU care, vasopressors, broad-spectrum antibiotics, and IR-guided JP drain placement. CT imaging showed extensive necrosis into the pelvis, despite some improvement in prior collections. A multidisciplinary team proceeded with EDGE using a LAMS via a gastro-gastric fistula. Persistent undrained necrosis prompted endoscopic necrosectomy and pigtail stent placement.
Discussion: Gallstones are the most common risk factor for necrotizing pancreatitis. Rapid weight loss post-RYGB increases gallstone formation. Although post-RYGB pancreatitis is often mild, altered anatomy can complicate its course and limit traditional management options. Current guidelines recommend moderately aggressive fluid resuscitation and early enteral nutrition, with delayed interventions (ideally ≥4 weeks) for necrosis. However, in this case, worsening clinical status prompted earlier intervention.
The RYGB anatomy likely impaired peripancreatic drainage, contributing to sepsis and prolonged illness. It underscores the importance of individualized decision-making in post-bariatric patients and raises the question of whether earlier intervention may benefit select high-risk cases. Further studies are needed to assess outcomes of early endoscopic intervention in patients with altered anatomy.

Figure: CT scan showing pancreatic necrosis (Yellow arrow).
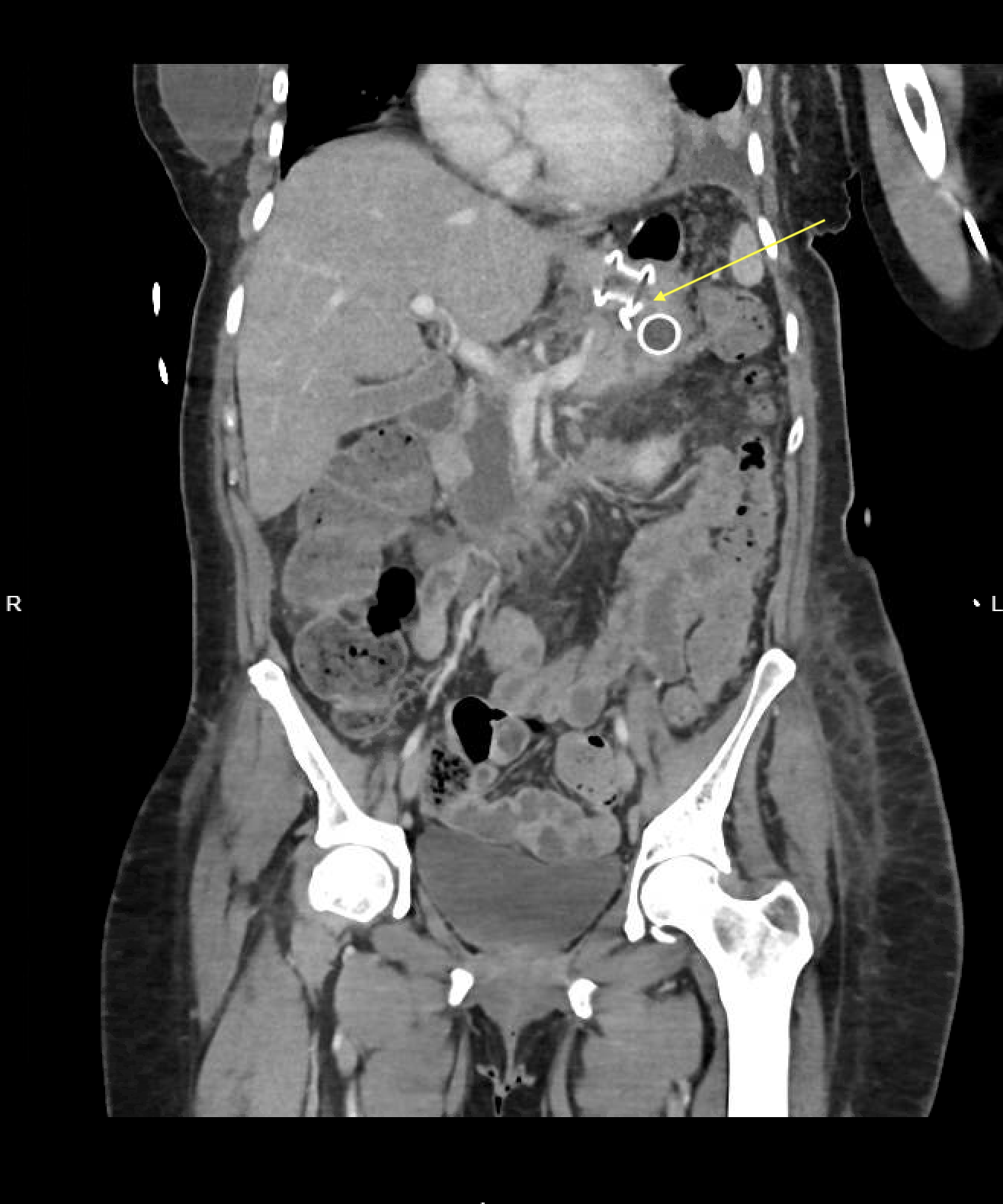
Figure: CT image with necrotizing pancreatitis and lumen-apposing metal stent (LAMS) at a cysto-gastrostomy (Yellow arrow).
Disclosures:
Karan Yagnik indicated no relevant financial relationships.
Suryansh Atreya indicated no relevant financial relationships.
FNU Payal indicated no relevant financial relationships.
Mitsu Patel indicated no relevant financial relationships.
Jilliane Unas indicated no relevant financial relationships.
Nishtha Nigam indicated no relevant financial relationships.
Anirudh Kulkarni indicated no relevant financial relationships.
Dhramesh Kaswala indicated no relevant financial relationships.
Anish Patel indicated no relevant financial relationships.
Wael Ghali indicated no relevant financial relationships.
Karan J.. Yagnik, MD1, Suryansh Atreya, MD1, FNU Payal, MD1, Mitsu Patel, BA2, Jilliane Unas, MD1, Nishtha Nigam, MD1, Anirudh Kulkarni, BS2, Dhramesh Kaswala, MD1, Anish V. Patel, MD2, Wael Ghali, MD1. P1471 - When Guidelines Fall Short: Necrotizing Pancreatitis After Gastric Bypass Sparks Debate, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Monmouth Medical Center, Robert Wood Johnson Medical School of Rutgers University, Long Branch, NJ; 2Robert Wood Johnson Medical School, Rutgers University, New Brunswick, NJ
Introduction: We present a case of post-Roux-en-Y gastric bypass (RYGB) acute pancreatitis rapidly progressing to necrosis, ascites, sepsis, and respiratory failure, requiring prolonged hospitalization and complex interventions due to altered anatomy.
Case Description/
Methods: A female in her early 50s, with RYGB performed 2.5 months prior, presented with acute abdominal pain, nausea, and vomiting. Labs revealed markedly elevated amylase, lipase. Initial CT abdomen/pelvis showed acute pancreatitis without gallstones or biliary dilation. She was admitted for supportive care. Overnight, she developed worsening abdominal distension, obstipation, guarding, hypoactive bowel sounds, and rising hematocrit with elevated bladder pressure. Repeat CT showed necrotizing pancreatitis, large loculated ascites and bilateral pleural effusions. Bedside ultrasound revealed cholelithiasis. She was intubated for respiratory distress and transferred to a tertiary center.
At the tertiary center, EUS was performed, but an EDGE procedure was deferred to preserve pancreatic drainage pathways. Later, EUS-guided cystogastrostomy was attempted but failed due to solid collection; the stent was removed and closed with an over-the-scope clip. The patient developed sepsis, requiring ICU care, vasopressors, broad-spectrum antibiotics, and IR-guided JP drain placement. CT imaging showed extensive necrosis into the pelvis, despite some improvement in prior collections. A multidisciplinary team proceeded with EDGE using a LAMS via a gastro-gastric fistula. Persistent undrained necrosis prompted endoscopic necrosectomy and pigtail stent placement.
Discussion: Gallstones are the most common risk factor for necrotizing pancreatitis. Rapid weight loss post-RYGB increases gallstone formation. Although post-RYGB pancreatitis is often mild, altered anatomy can complicate its course and limit traditional management options. Current guidelines recommend moderately aggressive fluid resuscitation and early enteral nutrition, with delayed interventions (ideally ≥4 weeks) for necrosis. However, in this case, worsening clinical status prompted earlier intervention.
The RYGB anatomy likely impaired peripancreatic drainage, contributing to sepsis and prolonged illness. It underscores the importance of individualized decision-making in post-bariatric patients and raises the question of whether earlier intervention may benefit select high-risk cases. Further studies are needed to assess outcomes of early endoscopic intervention in patients with altered anatomy.

Figure: CT scan showing pancreatic necrosis (Yellow arrow).
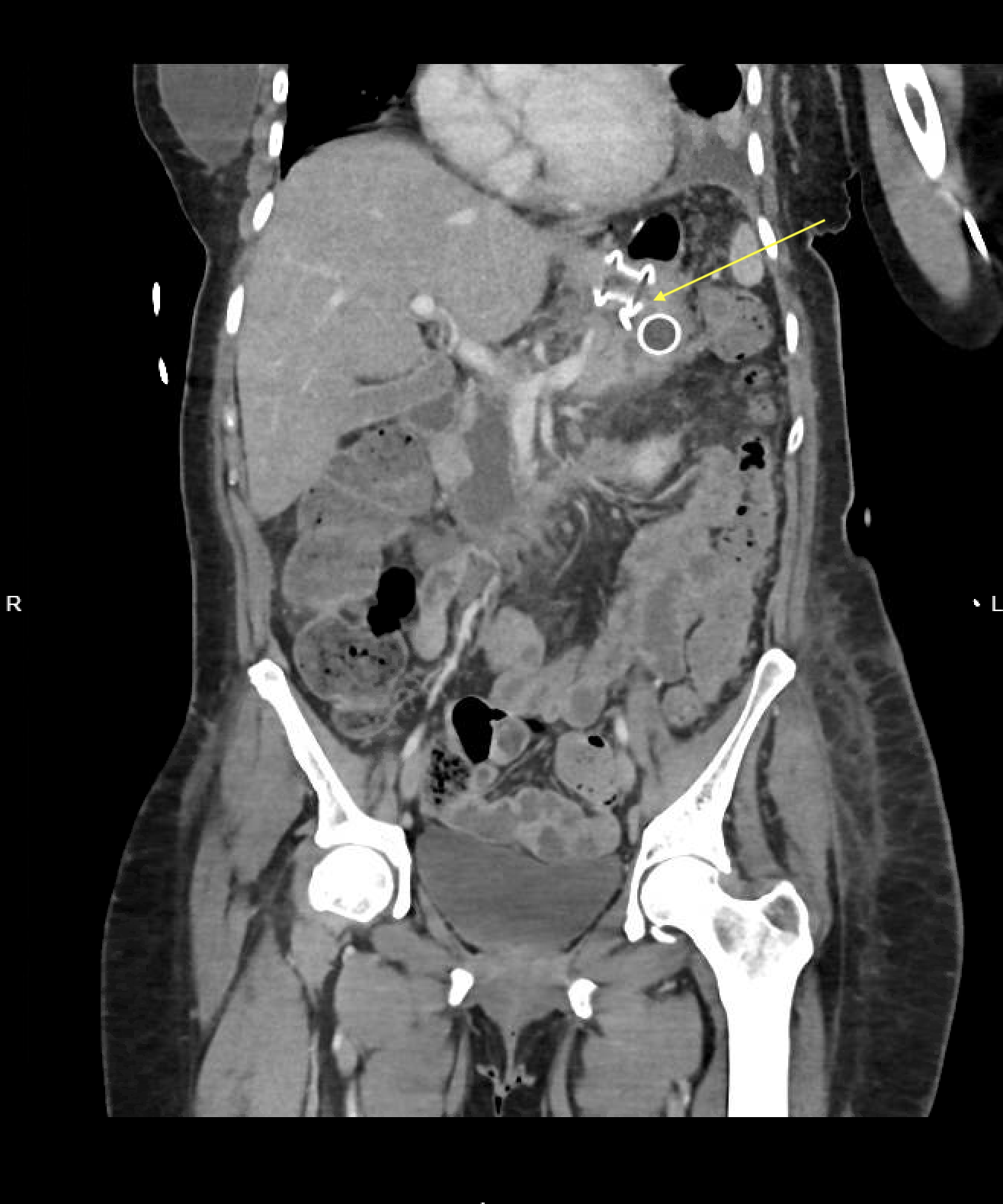
Figure: CT image with necrotizing pancreatitis and lumen-apposing metal stent (LAMS) at a cysto-gastrostomy (Yellow arrow).
Disclosures:
Karan Yagnik indicated no relevant financial relationships.
Suryansh Atreya indicated no relevant financial relationships.
FNU Payal indicated no relevant financial relationships.
Mitsu Patel indicated no relevant financial relationships.
Jilliane Unas indicated no relevant financial relationships.
Nishtha Nigam indicated no relevant financial relationships.
Anirudh Kulkarni indicated no relevant financial relationships.
Dhramesh Kaswala indicated no relevant financial relationships.
Anish Patel indicated no relevant financial relationships.
Wael Ghali indicated no relevant financial relationships.
Karan J.. Yagnik, MD1, Suryansh Atreya, MD1, FNU Payal, MD1, Mitsu Patel, BA2, Jilliane Unas, MD1, Nishtha Nigam, MD1, Anirudh Kulkarni, BS2, Dhramesh Kaswala, MD1, Anish V. Patel, MD2, Wael Ghali, MD1. P1471 - When Guidelines Fall Short: Necrotizing Pancreatitis After Gastric Bypass Sparks Debate, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
