Sunday Poster Session
Category: Interventional Endoscopy
P1470 - PTBD-EDGE Rendezvous for Malignant Biliary Obstruction and Afferent Loop Syndrome in Surgically Altered Anatomy After Failure of Conventional Approaches
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Esma Zeynep Kizilaslan, MD (she/her/hers)
University Hospital Düsseldorf
Düsseldorf, Nordrhein-Westfalen, Germany
Presenting Author(s)
Esma Zeynep Kizilaslan, MD, Sven Heiko Loosen, MD, Christoph Roderburg, MD, Tom Luedde, PhD, Jennis Kandler, MD
University Hospital Düsseldorf, Düsseldorf, Nordrhein-Westfalen, Germany
Introduction: Pancreatic cancer, particularly borderline resectable pancreatic head carcinoma, poses major challenges due to its aggressiveness, anatomical complexity, and frequent complications. We present a complex case illustrating the use of a PTBD-EDGE rendezvous, a rarely described approach for achieving biliary access and internal drainage.
Case Description/
Methods: A 68-year-old male with borderline resectable pancreatic head carcinoma underwent neoadjuvant chemotherapy. The patient developed malignant gastric outlet obstruction (MGOO), requiring a Roux-en-Y gastrojejunostomy. Due to tumor progression, chemotherapy was switched to palliative regimen. Exploratory laparotomy revealed unresectability.
Upon further progression, the tumor infiltrated the gastroenterostomy and led to superior mesenteric vein thrombosis, causing recurrent MGOO and portocaval collateral formation with repeated upper GI bleeding. A partial gastrectomy, revision of the gastrojejunostomy, and creation of a splenorenal (Warren) shunt were performed. Intensive systemic therapy was resumed.
Three years later, malignant distal biliary obstruction (MDBO) occurred. Endoscopic ultrasound-guided biliary drainage (EUS-BD) was not feasible due to perigastric collaterals. Enteroscopic ERCP (E-ERCP) failed due to adhesions and an inaccessible afferent loop. Thus, percutaneous transhepatic biliary drainage (PTBD) with same-session uncovered metal stent (UCSEMS) placement was initiated.
Fluoroscopy during PTBD revealed an afferent loop syndrome, making standard stenting ineffective due to impaired aboral bile flow. A percutaneous drain was placed, and the afferent loop filled with water to facilitate endoscopic ultrasound-guided gastroenterostomy (EUS-GE) using an electrocautery-enhanced lumen-apposing metal stent (ECE-LAMS, HotAxios 15×10 mm).
Via this access, a transgastric ERCP (EDGE) with PTBD rendezvous (PTBD-EDGE) enabled successful UC-SEMS placement (Wallflex Biliary RX, 10×60 mm) for definitive biliary decompression.
Eleven months later, stent dysfunction due to tumor ingrowth was effectively managed by EDGE-assisted intraductal radiofrequency ablation (id-RFA, Habib EndoHPB probe, 10 W, 90 s, bipolar soft mode).
Discussion: This case underscores the importance of individualized, multidisciplinary care in advanced pancreatic cancer. Combined percutaneous and advanced endoscopic techniques can provide effective palliation, even in highly complex clinical situations.
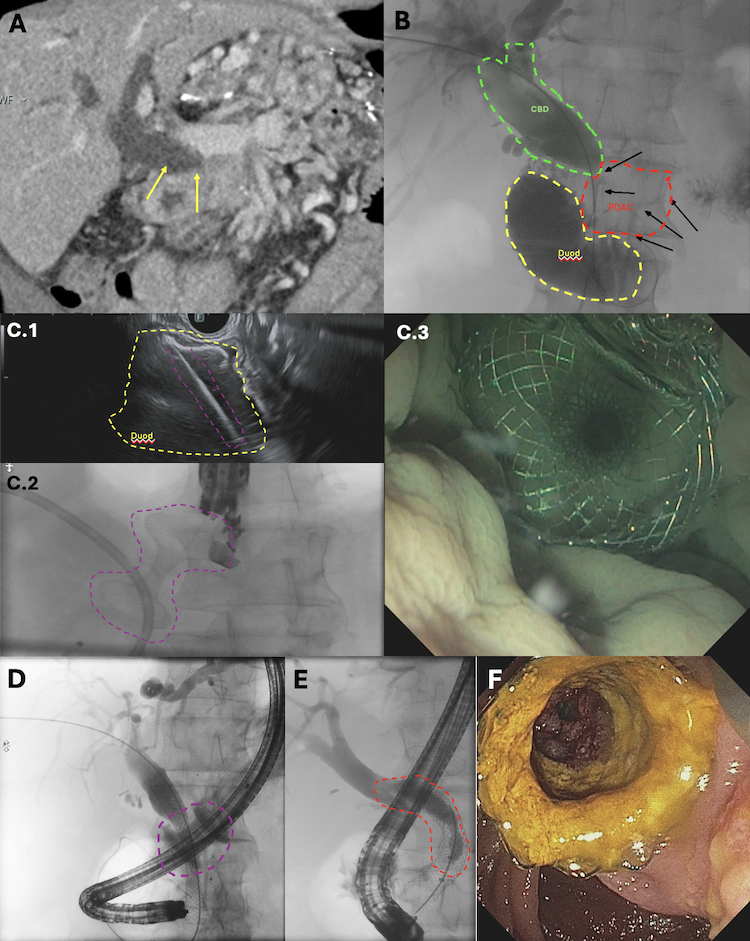
Figure: Fig. 1.: Multimodal imaging and procedural sequence illustrating the management of malignant biliary obstruction and afferent loop syndrome in a patient with advanced pancreatic head carcinoma. Cross-sectional and fluoroscopic imaging confirmed combined afferent limb and biliary obstruction due to tumor progression. Definitive drainage was achieved through a stepwise approach: PTBD insertion, creation of a gastroenterostomy via EUS-guided LAMS placement, followed by a PTBD-EDGE rendezvous procedure enabling transgastric biliary stenting. Recurrent biliary obstruction was successfully managed with intraductal radiofrequency ablation and stent-in-stent placement.
A: Contrast-enhanced CT image demonstrating intra- and extrahepatic cholestasis with marked upstream dilation of the common bile duct (CBD, yellow arrows). A hypodense mass consistent with the known pancreatic head carcinoma is visible, causing compression of the distal CBD and duodenum B. Fluoroscopic image illustrating severe dilation of the CBD (green outline) and afferent loop syndrome (yellow outline) with fluid-filled, distended duodenum secondary to obstructive growth of the pancreatic head tumor (red outline), correlating with findings in Figure A. C1. EUS-guided puncture of the fluid-distended afferent limb (yellow outline), previously infused with saline via PTBD, to create a gastroenterostomy. A 15 × 10 mm electrocautery-enhanced lumen-apposing metal stent (ECE-LAMS) was deployed for access. C2 Fluoroscopic confirmation of successful EUS-guided gastroenterostomy (EUS-GE) C3 White-light endoscopic image of the newly created gastroenterostomy showing effective drainage of indigo carmine–stained saline, confirming proper flow from the afferent limb D. Fluoroscopic view of a duodenoscope being advanced through the GE tract (indicated by purple dashed line) toward the papilla. A PTBD-EDGE randevouz was performed, allowing successful placement of an uncovered self-expandable metal stent (UC-SEMS, 10 × 60 mm) in the CBD with immediate biliary decompression E. Follow-up fluoroscopic image eleven months later showing a contrast defect within the previously placed UC-SEMS, consistent with tumor ingrowth and biliary obstruction recurrence F. White-light endoscopic view of the UC-SEMS obstruction, with visible yellowish fibrotic tumor ingrowth. The stent was successfully recanalized using intraductal radiofrequency ablation (id-RFA, two cycles of 90 seconds, 10W, bipolar mode).
Disclosures:
Esma Zeynep Kizilaslan indicated no relevant financial relationships.
Sven Heiko Loosen indicated no relevant financial relationships.
Christoph Roderburg indicated no relevant financial relationships.
Tom Luedde indicated no relevant financial relationships.
Jennis Kandler indicated no relevant financial relationships.
Esma Zeynep Kizilaslan, MD, Sven Heiko Loosen, MD, Christoph Roderburg, MD, Tom Luedde, PhD, Jennis Kandler, MD. P1470 - PTBD-EDGE Rendezvous for Malignant Biliary Obstruction and Afferent Loop Syndrome in Surgically Altered Anatomy After Failure of Conventional Approaches, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University Hospital Düsseldorf, Düsseldorf, Nordrhein-Westfalen, Germany
Introduction: Pancreatic cancer, particularly borderline resectable pancreatic head carcinoma, poses major challenges due to its aggressiveness, anatomical complexity, and frequent complications. We present a complex case illustrating the use of a PTBD-EDGE rendezvous, a rarely described approach for achieving biliary access and internal drainage.
Case Description/
Methods: A 68-year-old male with borderline resectable pancreatic head carcinoma underwent neoadjuvant chemotherapy. The patient developed malignant gastric outlet obstruction (MGOO), requiring a Roux-en-Y gastrojejunostomy. Due to tumor progression, chemotherapy was switched to palliative regimen. Exploratory laparotomy revealed unresectability.
Upon further progression, the tumor infiltrated the gastroenterostomy and led to superior mesenteric vein thrombosis, causing recurrent MGOO and portocaval collateral formation with repeated upper GI bleeding. A partial gastrectomy, revision of the gastrojejunostomy, and creation of a splenorenal (Warren) shunt were performed. Intensive systemic therapy was resumed.
Three years later, malignant distal biliary obstruction (MDBO) occurred. Endoscopic ultrasound-guided biliary drainage (EUS-BD) was not feasible due to perigastric collaterals. Enteroscopic ERCP (E-ERCP) failed due to adhesions and an inaccessible afferent loop. Thus, percutaneous transhepatic biliary drainage (PTBD) with same-session uncovered metal stent (UCSEMS) placement was initiated.
Fluoroscopy during PTBD revealed an afferent loop syndrome, making standard stenting ineffective due to impaired aboral bile flow. A percutaneous drain was placed, and the afferent loop filled with water to facilitate endoscopic ultrasound-guided gastroenterostomy (EUS-GE) using an electrocautery-enhanced lumen-apposing metal stent (ECE-LAMS, HotAxios 15×10 mm).
Via this access, a transgastric ERCP (EDGE) with PTBD rendezvous (PTBD-EDGE) enabled successful UC-SEMS placement (Wallflex Biliary RX, 10×60 mm) for definitive biliary decompression.
Eleven months later, stent dysfunction due to tumor ingrowth was effectively managed by EDGE-assisted intraductal radiofrequency ablation (id-RFA, Habib EndoHPB probe, 10 W, 90 s, bipolar soft mode).
Discussion: This case underscores the importance of individualized, multidisciplinary care in advanced pancreatic cancer. Combined percutaneous and advanced endoscopic techniques can provide effective palliation, even in highly complex clinical situations.
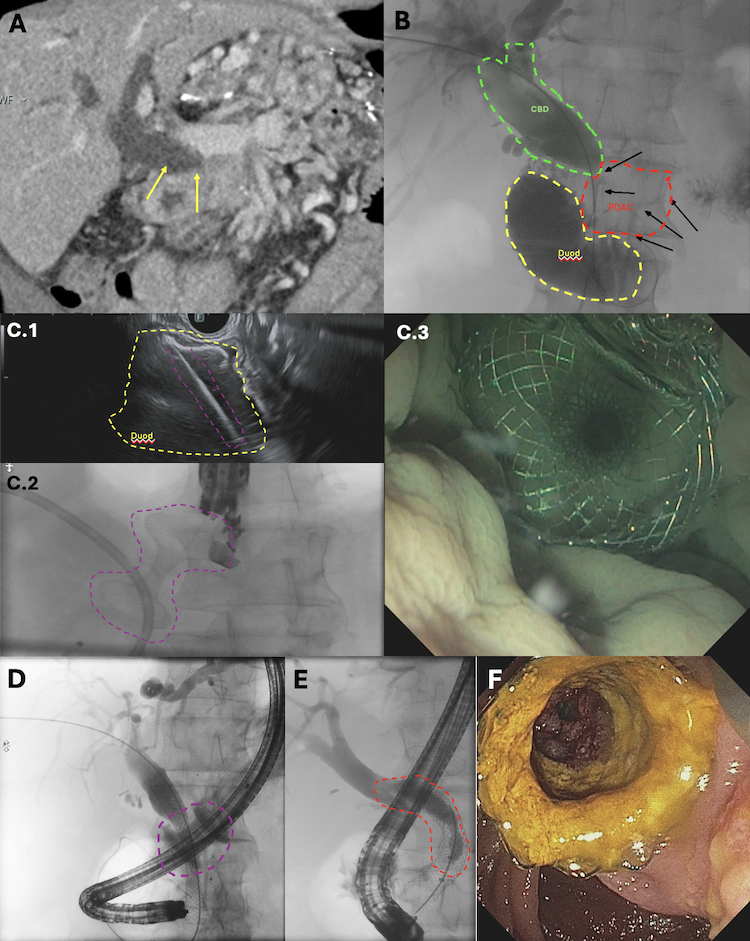
Figure: Fig. 1.: Multimodal imaging and procedural sequence illustrating the management of malignant biliary obstruction and afferent loop syndrome in a patient with advanced pancreatic head carcinoma. Cross-sectional and fluoroscopic imaging confirmed combined afferent limb and biliary obstruction due to tumor progression. Definitive drainage was achieved through a stepwise approach: PTBD insertion, creation of a gastroenterostomy via EUS-guided LAMS placement, followed by a PTBD-EDGE rendezvous procedure enabling transgastric biliary stenting. Recurrent biliary obstruction was successfully managed with intraductal radiofrequency ablation and stent-in-stent placement.
A: Contrast-enhanced CT image demonstrating intra- and extrahepatic cholestasis with marked upstream dilation of the common bile duct (CBD, yellow arrows). A hypodense mass consistent with the known pancreatic head carcinoma is visible, causing compression of the distal CBD and duodenum B. Fluoroscopic image illustrating severe dilation of the CBD (green outline) and afferent loop syndrome (yellow outline) with fluid-filled, distended duodenum secondary to obstructive growth of the pancreatic head tumor (red outline), correlating with findings in Figure A. C1. EUS-guided puncture of the fluid-distended afferent limb (yellow outline), previously infused with saline via PTBD, to create a gastroenterostomy. A 15 × 10 mm electrocautery-enhanced lumen-apposing metal stent (ECE-LAMS) was deployed for access. C2 Fluoroscopic confirmation of successful EUS-guided gastroenterostomy (EUS-GE) C3 White-light endoscopic image of the newly created gastroenterostomy showing effective drainage of indigo carmine–stained saline, confirming proper flow from the afferent limb D. Fluoroscopic view of a duodenoscope being advanced through the GE tract (indicated by purple dashed line) toward the papilla. A PTBD-EDGE randevouz was performed, allowing successful placement of an uncovered self-expandable metal stent (UC-SEMS, 10 × 60 mm) in the CBD with immediate biliary decompression E. Follow-up fluoroscopic image eleven months later showing a contrast defect within the previously placed UC-SEMS, consistent with tumor ingrowth and biliary obstruction recurrence F. White-light endoscopic view of the UC-SEMS obstruction, with visible yellowish fibrotic tumor ingrowth. The stent was successfully recanalized using intraductal radiofrequency ablation (id-RFA, two cycles of 90 seconds, 10W, bipolar mode).
Disclosures:
Esma Zeynep Kizilaslan indicated no relevant financial relationships.
Sven Heiko Loosen indicated no relevant financial relationships.
Christoph Roderburg indicated no relevant financial relationships.
Tom Luedde indicated no relevant financial relationships.
Jennis Kandler indicated no relevant financial relationships.
Esma Zeynep Kizilaslan, MD, Sven Heiko Loosen, MD, Christoph Roderburg, MD, Tom Luedde, PhD, Jennis Kandler, MD. P1470 - PTBD-EDGE Rendezvous for Malignant Biliary Obstruction and Afferent Loop Syndrome in Surgically Altered Anatomy After Failure of Conventional Approaches, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

