Sunday Poster Session
Category: Interventional Endoscopy
P1453 - Small Bowel Enteroscopy in Evaluation of Obscure Gastrointestinal Bleeding: Metastatic Melanoma of the Small Bowel
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- AV
Amberly Vaughan, MD (she/her/hers)
Keesler Medical Center
Biloxi, MS
Presenting Author(s)
Amberly Vaughan, MD, Rachel Pray, DO, Wassem Juakiem, MD
Keesler Medical Center, Biloxi, MS
Introduction: Small bowel malignant melanoma is an exceedingly uncommon disease, accounting for only 1%–3% of all GI malignancies. The majority of cases occur with metastatic disease, with the majority originating from an initial cutaneous lesion. Symptoms are nonspecific, and because the anatomy of the small bowel makes endoscopic visualization difficult, the diagnosis is frequently delayed and many cases are not made until autopsy. We report here a case of small bowel melanoma in a 55-year-old male with a history of complete resection of an earlier cutaneous melanoma, highlighting the diagnostic challenge in this unusual presentation.
Case Description/
Methods: A 55-year-old male with a history of cutaneous melanoma status post wide local excision and negative sentinel lymph node biopsy presented with shortness of breath, dizziness, and melena. Esophagogastroduodenoscopy and colonoscopy were not able to identify an etiology of bleeding. Capsule endoscopy indicated bleeding beyond the duodenum with multiple mass-like lesions. Small bowel enteroscopy and biopsy were positive for two dysplastic-appearing, ulcerated, bleeding lesions of the duodenum and jejunum. Pathology established metastatic melanoma. The patient underwent palliative resection and was initiated on combination immunotherapy using nivolumab and ipilimumab.
Discussion: This case illustrates the necessity of maintaining a high index of suspicion for gastrointestinal metastasis in patients with past history of cutaneous melanoma, regardless of past negative staging or length of time since initial therapy. Melanoma is notorious for its unpredictable metastatic course and late recurrence, and thus late presentation is particularly vexing. The patient's initial endoscopies emphasize the diagnostic value of capsule endoscopy and deep enteroscopy in the evaluation of obscure GI bleeding. Micrometastases may be latent for years, making ongoing clinical surveillance imperative. While outcomes have been transformed in advanced melanoma with the introduction of immunotherapy, surgery remains indicated for palliation in bleeding or obstruction. Multidisciplinary management is necessary in order to obtain timely diagnosis and optimal management in such complex presentations.
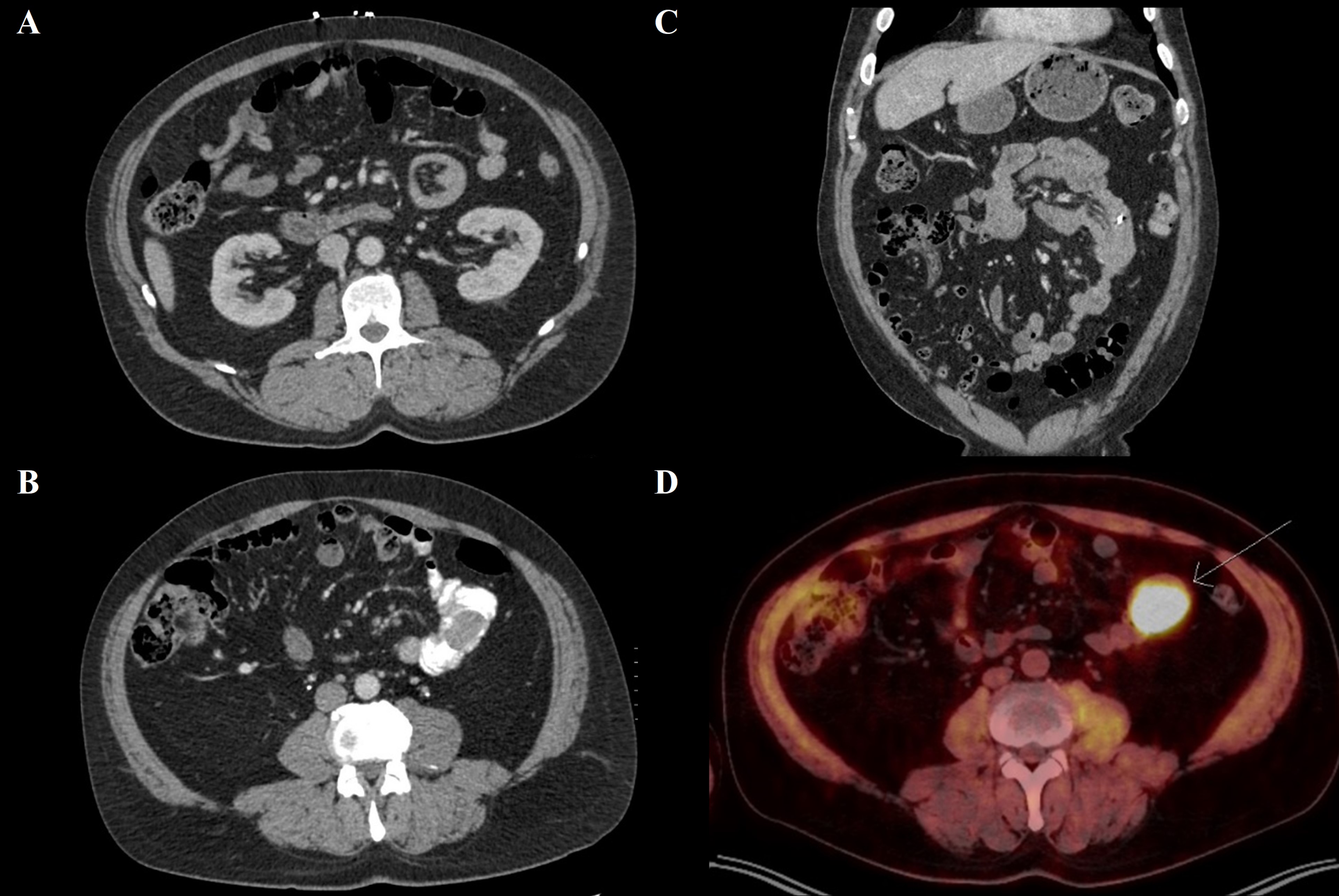
Figure: (A) Small bowel intussusception on CT, transverse (B) Mass on CT with oral contrast (C) Small bowel intussusception on CT, coronal (D) FDG avid small bowel lesion on PET
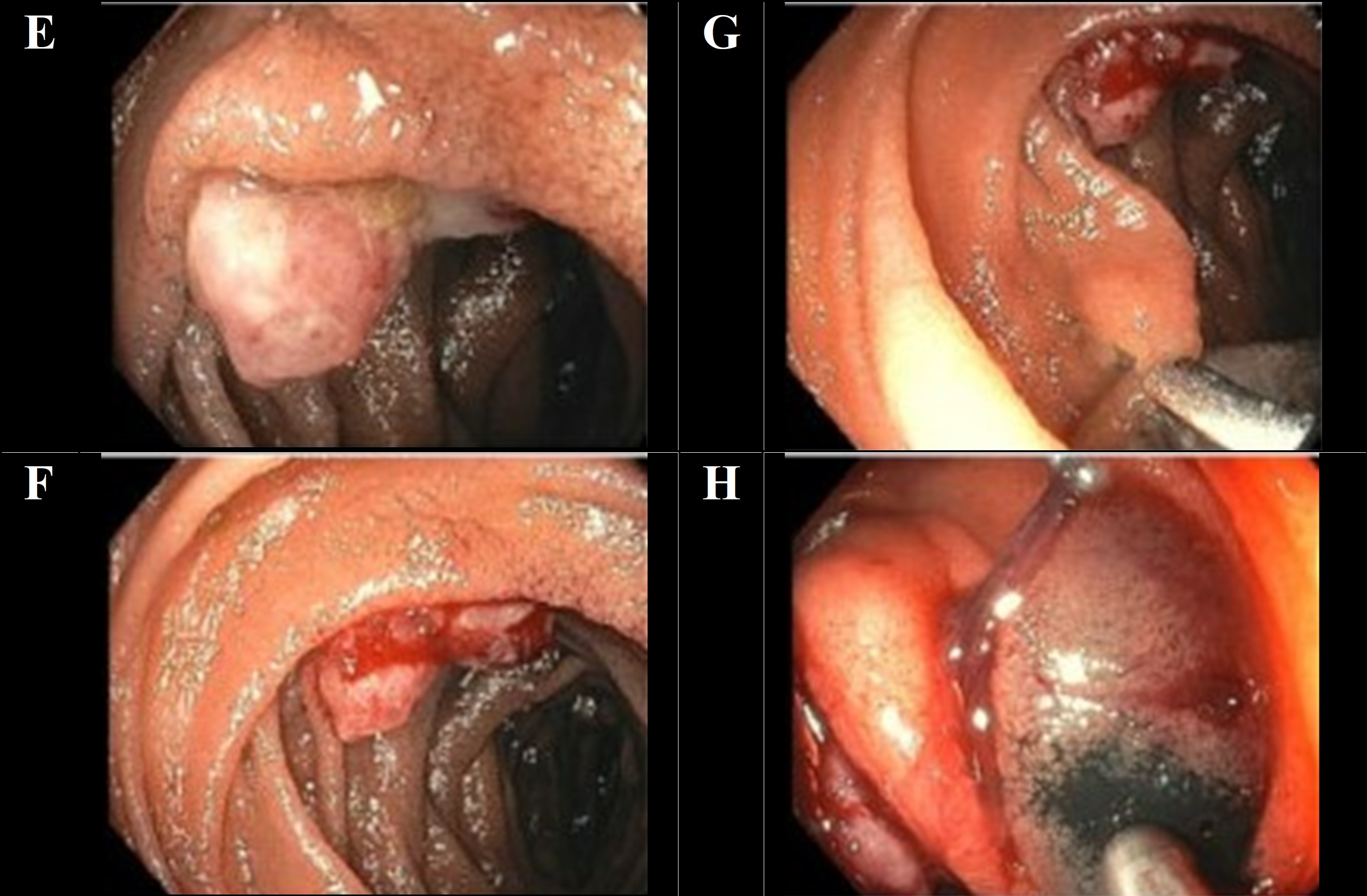
Figure: (E-H) Small bowel enteroscopy and biopsy revealed two dysplastic-appearing, ulcerated, bleeding lesions in the duodenum and jejunum.
Disclosures:
Amberly Vaughan indicated no relevant financial relationships.
Rachel Pray indicated no relevant financial relationships.
Wassem Juakiem indicated no relevant financial relationships.
Amberly Vaughan, MD, Rachel Pray, DO, Wassem Juakiem, MD. P1453 - Small Bowel Enteroscopy in Evaluation of Obscure Gastrointestinal Bleeding: Metastatic Melanoma of the Small Bowel, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Keesler Medical Center, Biloxi, MS
Introduction: Small bowel malignant melanoma is an exceedingly uncommon disease, accounting for only 1%–3% of all GI malignancies. The majority of cases occur with metastatic disease, with the majority originating from an initial cutaneous lesion. Symptoms are nonspecific, and because the anatomy of the small bowel makes endoscopic visualization difficult, the diagnosis is frequently delayed and many cases are not made until autopsy. We report here a case of small bowel melanoma in a 55-year-old male with a history of complete resection of an earlier cutaneous melanoma, highlighting the diagnostic challenge in this unusual presentation.
Case Description/
Methods: A 55-year-old male with a history of cutaneous melanoma status post wide local excision and negative sentinel lymph node biopsy presented with shortness of breath, dizziness, and melena. Esophagogastroduodenoscopy and colonoscopy were not able to identify an etiology of bleeding. Capsule endoscopy indicated bleeding beyond the duodenum with multiple mass-like lesions. Small bowel enteroscopy and biopsy were positive for two dysplastic-appearing, ulcerated, bleeding lesions of the duodenum and jejunum. Pathology established metastatic melanoma. The patient underwent palliative resection and was initiated on combination immunotherapy using nivolumab and ipilimumab.
Discussion: This case illustrates the necessity of maintaining a high index of suspicion for gastrointestinal metastasis in patients with past history of cutaneous melanoma, regardless of past negative staging or length of time since initial therapy. Melanoma is notorious for its unpredictable metastatic course and late recurrence, and thus late presentation is particularly vexing. The patient's initial endoscopies emphasize the diagnostic value of capsule endoscopy and deep enteroscopy in the evaluation of obscure GI bleeding. Micrometastases may be latent for years, making ongoing clinical surveillance imperative. While outcomes have been transformed in advanced melanoma with the introduction of immunotherapy, surgery remains indicated for palliation in bleeding or obstruction. Multidisciplinary management is necessary in order to obtain timely diagnosis and optimal management in such complex presentations.
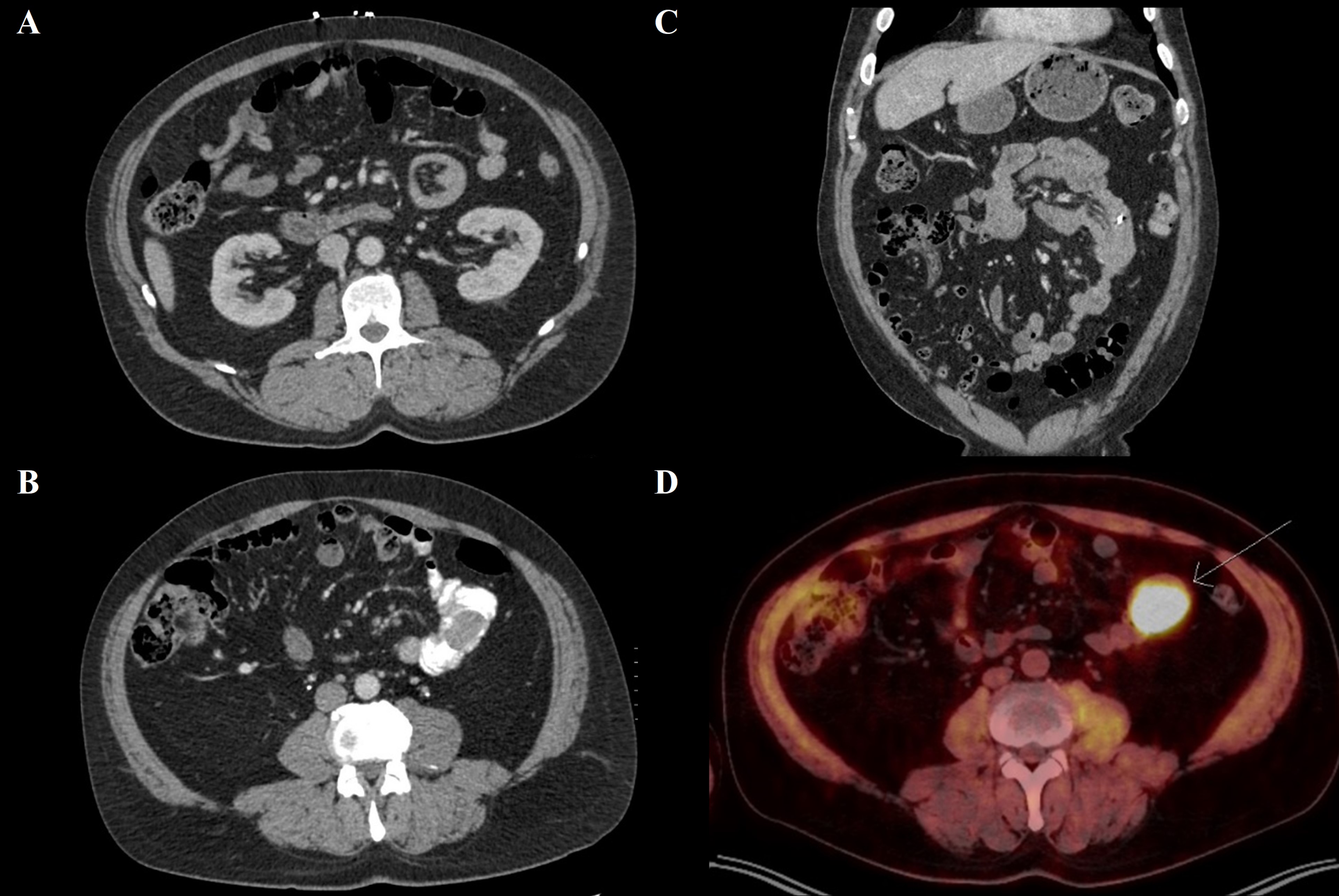
Figure: (A) Small bowel intussusception on CT, transverse (B) Mass on CT with oral contrast (C) Small bowel intussusception on CT, coronal (D) FDG avid small bowel lesion on PET
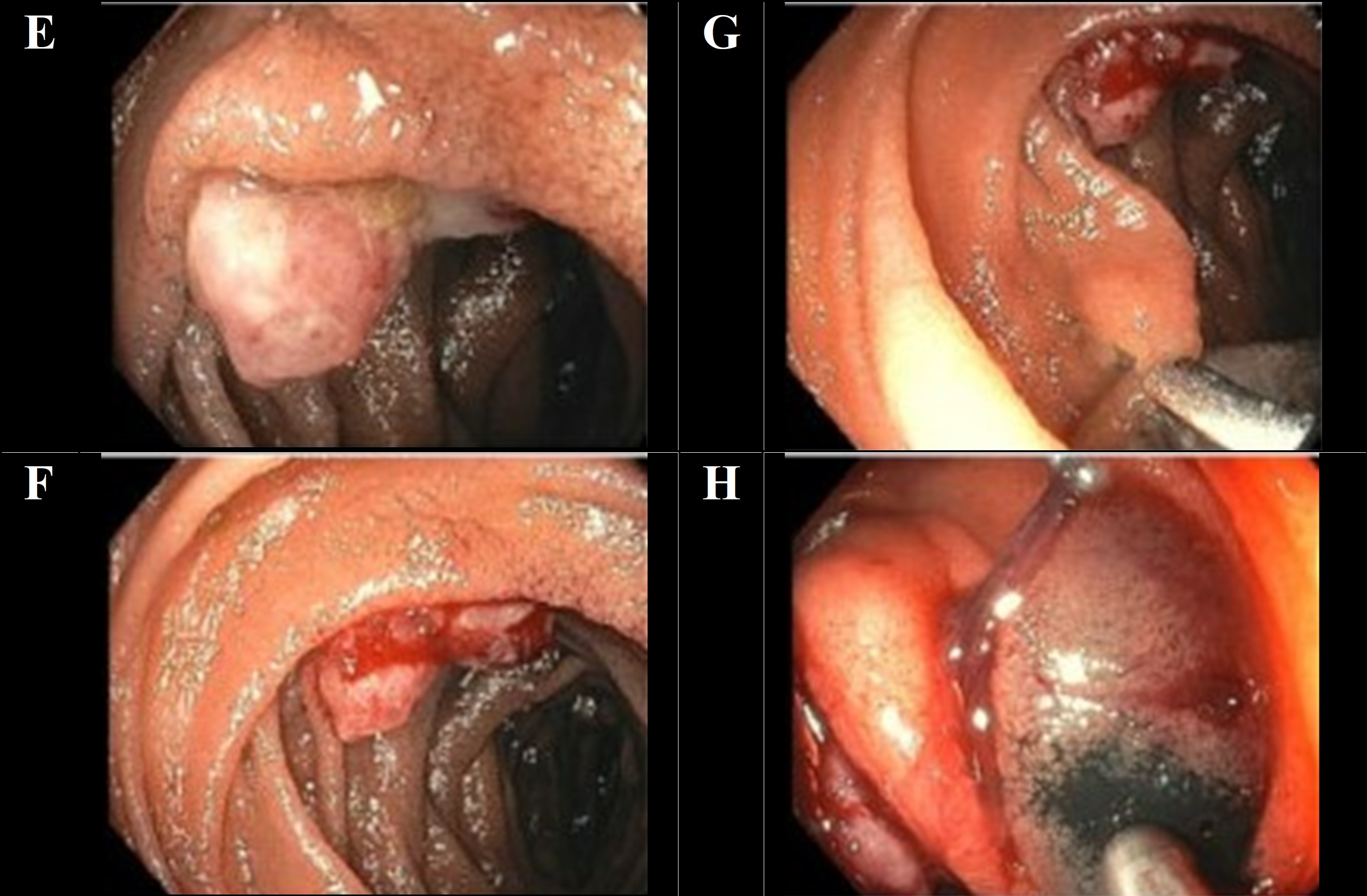
Figure: (E-H) Small bowel enteroscopy and biopsy revealed two dysplastic-appearing, ulcerated, bleeding lesions in the duodenum and jejunum.
Disclosures:
Amberly Vaughan indicated no relevant financial relationships.
Rachel Pray indicated no relevant financial relationships.
Wassem Juakiem indicated no relevant financial relationships.
Amberly Vaughan, MD, Rachel Pray, DO, Wassem Juakiem, MD. P1453 - Small Bowel Enteroscopy in Evaluation of Obscure Gastrointestinal Bleeding: Metastatic Melanoma of the Small Bowel, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
