Sunday Poster Session
Category: Liver
P1561 - Disparities in Utilization of Palliative Care in Acute-on-Chronic Liver Failure (ACLF) in the United States
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Aalam Sohal, MD
Creighton University School of Medicine
Phoenix, AZ
Presenting Author(s)
Aalam Sohal, MD1, Carol Singh, MBBS2, Rahul Chikatmalla, MBBS3, Joanne Lin, DO4, Isha Kohli, MBBS, MPH5, Sunny Sandhu, MD6, Nilofar Najafian, MD1
1Creighton University School of Medicine, Phoenix, AZ; 2Dayanand Medical College and Hospital, New Jersey, NJ; 3University of Miami, Miami, FL; 4University of California San Francisco, San Francisco, CA; 5Icahn School of Medicine at Mount Sinai, New York, NY; 6Stanford University, Palo Alto, CA
Introduction: Acute-on-chronic liver failure (ACLF) is a rapidly progressive syndrome characterized by hepatic decompensation, systemic inflammation, and multi-organ failure, and is associated with a high mortality. Although current guidelines recommend incorporation of palliative care (PC) in these critically ill patients, the resource remains underutilized. Identifying factors associated with PC use, especially in those with in-hospital mortality, is essential to address any disparities and improve the quality of care for patients with ACLF.
Methods: The National Inpatient Sample Database (2016-2022) was used to identify all adult in-hospital mortalities with ACLF. Patients were divided into two groups - stratified by PC utilization. Data was obtained on patient demographics, etiology of liver disease, liver-related decompensations, comorbidities, interventions, and clinical outcomes. Multivariate logistic and linear regression analyses were used to identify predictors of PC utilization in patients with ACLF and to assess the impact of PC on resource utilization.
Results: Of the total 227,900 in-hospital mortalities with ACLF, only 112,555 (49.3%) received PC. Among those who received PC, the majority were male (60.4%), White (68.7%), and had Medicare insurance (46.3%). Compared to Whites, African Americans and Hispanics each had 32% and 30% lower odds of receiving PC. There was an incremental increase in PC use based on income quartiles, with patients in the higher income quartiles having 35.5% higher odds of receiving PC compared to those in the lowest income quartiles. Teaching hospitals had 43.8% higher odds of providing PC than non-teaching hospitals. Compared to patients in the Northeast, those in the Midwest and West had 36.7% and 15.8% higher odds of PC, respectively. MASLD was associated with 9% higher odds of receiving PC. Conversely, patients who had a history of liver transplantation were less likely to receive PC (aOR 0.44; p-0.001) (Fig 1). There were no significant differences in the length of stay, however use of PC was associated with significant reductions in total hospitalization charges (adj. coefficient: -$13,924.1; p< 0.001) (Fig 2).
Discussion: Our study highlights significant racial, regional, socioeconomic, and clinical disparities in PC utilization in in-hospital mortalities with ACLF. These findings suggest that PC resources are not being equitably provided, underscoring the need for targeted interventions to address these gaps.
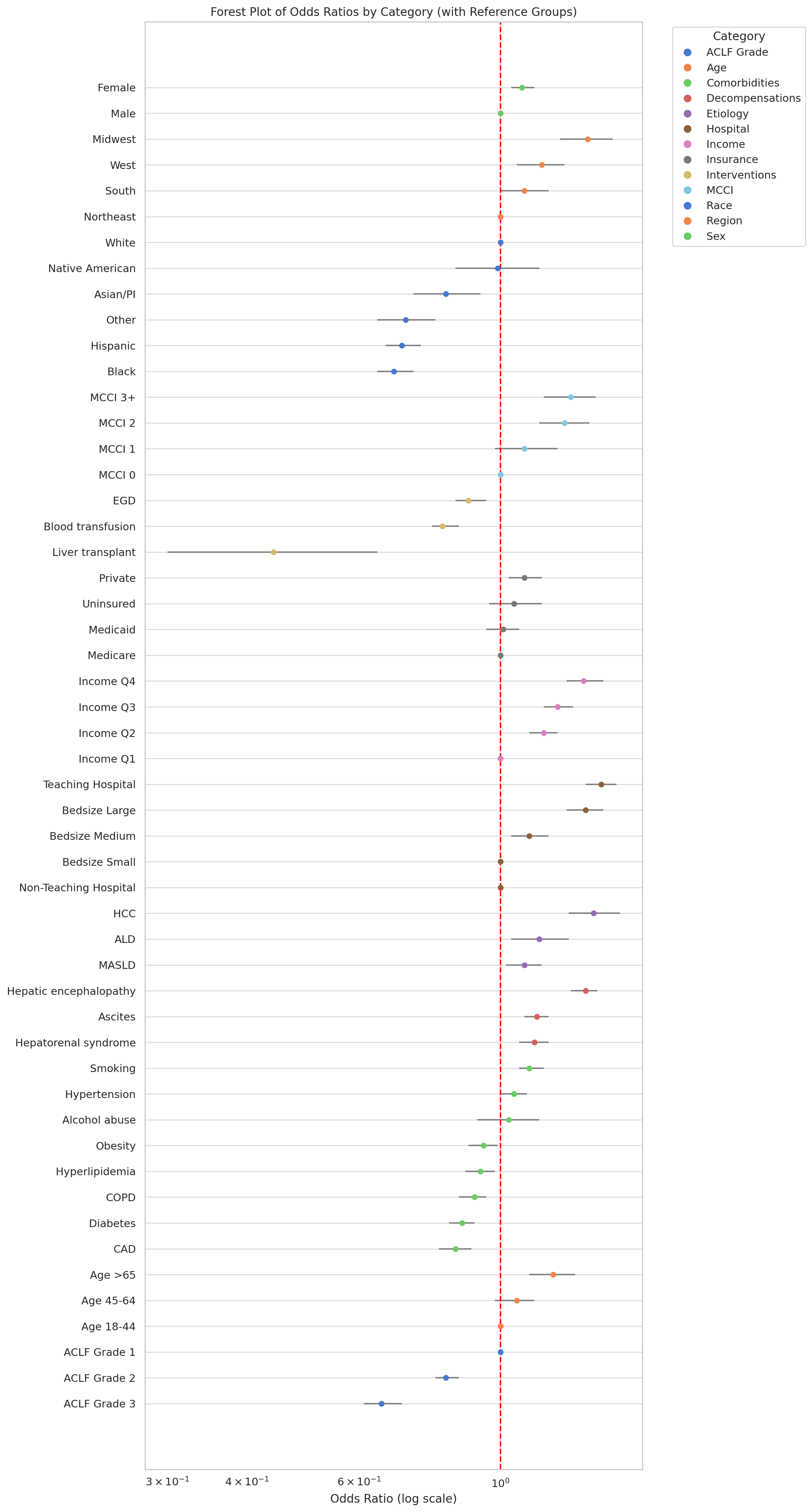
Figure: Figure 1- Forrest plot showing results of multivariate logistic regression assessing the odds of receiving PC for ACLF.

Figure: Figure 2- Resource utilization, stratified by the use of PC
Disclosures:
Aalam Sohal indicated no relevant financial relationships.
Carol Singh indicated no relevant financial relationships.
Rahul Chikatmalla indicated no relevant financial relationships.
Joanne Lin indicated no relevant financial relationships.
Isha Kohli indicated no relevant financial relationships.
Sunny Sandhu indicated no relevant financial relationships.
Nilofar Najafian indicated no relevant financial relationships.
Aalam Sohal, MD1, Carol Singh, MBBS2, Rahul Chikatmalla, MBBS3, Joanne Lin, DO4, Isha Kohli, MBBS, MPH5, Sunny Sandhu, MD6, Nilofar Najafian, MD1. P1561 - Disparities in Utilization of Palliative Care in Acute-on-Chronic Liver Failure (ACLF) in the United States, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Creighton University School of Medicine, Phoenix, AZ; 2Dayanand Medical College and Hospital, New Jersey, NJ; 3University of Miami, Miami, FL; 4University of California San Francisco, San Francisco, CA; 5Icahn School of Medicine at Mount Sinai, New York, NY; 6Stanford University, Palo Alto, CA
Introduction: Acute-on-chronic liver failure (ACLF) is a rapidly progressive syndrome characterized by hepatic decompensation, systemic inflammation, and multi-organ failure, and is associated with a high mortality. Although current guidelines recommend incorporation of palliative care (PC) in these critically ill patients, the resource remains underutilized. Identifying factors associated with PC use, especially in those with in-hospital mortality, is essential to address any disparities and improve the quality of care for patients with ACLF.
Methods: The National Inpatient Sample Database (2016-2022) was used to identify all adult in-hospital mortalities with ACLF. Patients were divided into two groups - stratified by PC utilization. Data was obtained on patient demographics, etiology of liver disease, liver-related decompensations, comorbidities, interventions, and clinical outcomes. Multivariate logistic and linear regression analyses were used to identify predictors of PC utilization in patients with ACLF and to assess the impact of PC on resource utilization.
Results: Of the total 227,900 in-hospital mortalities with ACLF, only 112,555 (49.3%) received PC. Among those who received PC, the majority were male (60.4%), White (68.7%), and had Medicare insurance (46.3%). Compared to Whites, African Americans and Hispanics each had 32% and 30% lower odds of receiving PC. There was an incremental increase in PC use based on income quartiles, with patients in the higher income quartiles having 35.5% higher odds of receiving PC compared to those in the lowest income quartiles. Teaching hospitals had 43.8% higher odds of providing PC than non-teaching hospitals. Compared to patients in the Northeast, those in the Midwest and West had 36.7% and 15.8% higher odds of PC, respectively. MASLD was associated with 9% higher odds of receiving PC. Conversely, patients who had a history of liver transplantation were less likely to receive PC (aOR 0.44; p-0.001) (Fig 1). There were no significant differences in the length of stay, however use of PC was associated with significant reductions in total hospitalization charges (adj. coefficient: -$13,924.1; p< 0.001) (Fig 2).
Discussion: Our study highlights significant racial, regional, socioeconomic, and clinical disparities in PC utilization in in-hospital mortalities with ACLF. These findings suggest that PC resources are not being equitably provided, underscoring the need for targeted interventions to address these gaps.
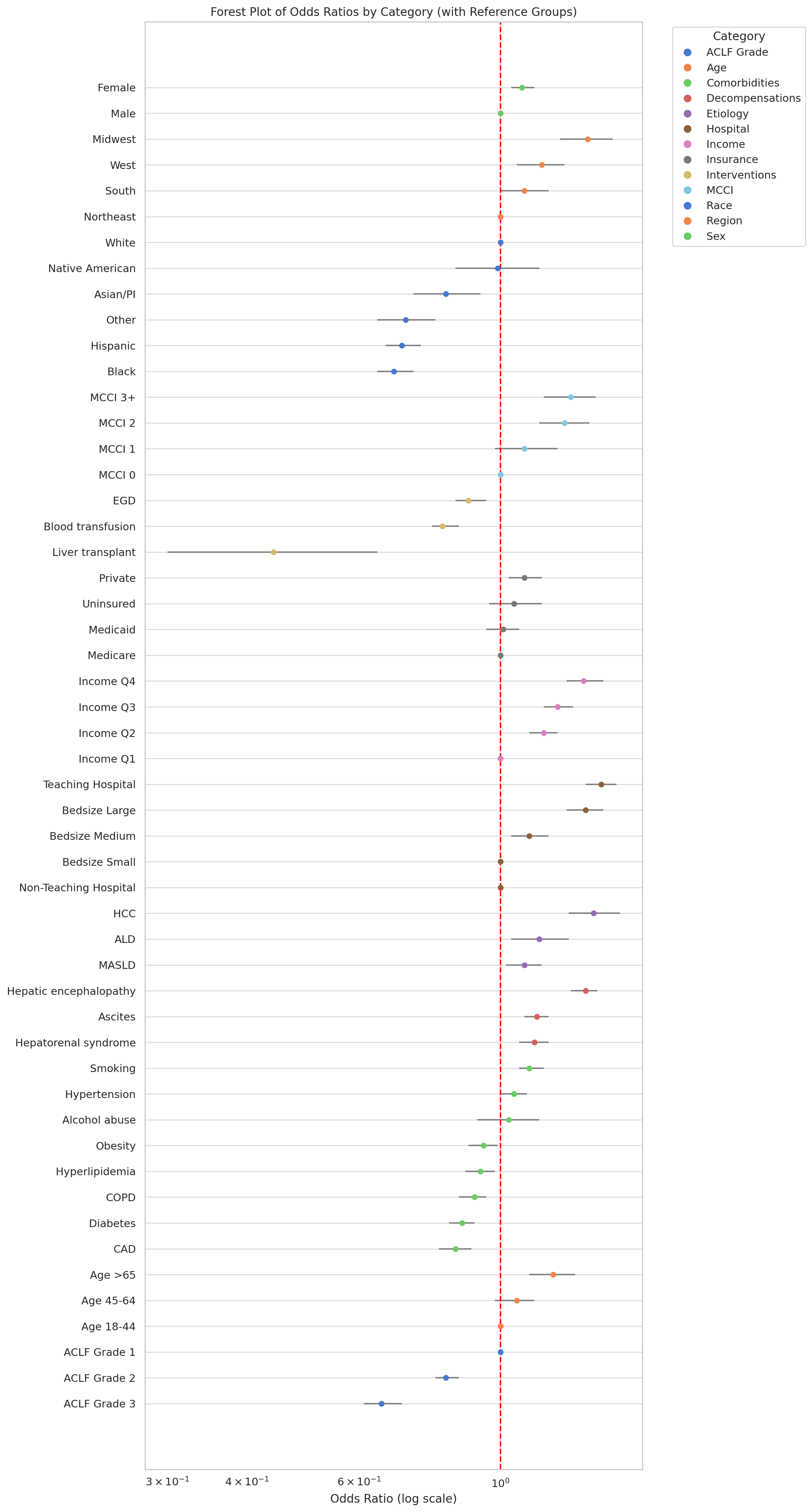
Figure: Figure 1- Forrest plot showing results of multivariate logistic regression assessing the odds of receiving PC for ACLF.

Figure: Figure 2- Resource utilization, stratified by the use of PC
Disclosures:
Aalam Sohal indicated no relevant financial relationships.
Carol Singh indicated no relevant financial relationships.
Rahul Chikatmalla indicated no relevant financial relationships.
Joanne Lin indicated no relevant financial relationships.
Isha Kohli indicated no relevant financial relationships.
Sunny Sandhu indicated no relevant financial relationships.
Nilofar Najafian indicated no relevant financial relationships.
Aalam Sohal, MD1, Carol Singh, MBBS2, Rahul Chikatmalla, MBBS3, Joanne Lin, DO4, Isha Kohli, MBBS, MPH5, Sunny Sandhu, MD6, Nilofar Najafian, MD1. P1561 - Disparities in Utilization of Palliative Care in Acute-on-Chronic Liver Failure (ACLF) in the United States, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
