Sunday Poster Session
Category: Liver
P1560 - Targeting Health Equity in Hepatitis C Elimination: A Quality Improvement Initiative to Re-engage Marginalized Veterans
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Janan D. Leppo, MD
UC San Diego Department of Internal Medicine
San Diego, CA
Presenting Author(s)
Janan D. Leppo, MD1, Ann Deioma, BSN, RN2, Heather Patton, MD2
1UC San Diego Department of Internal Medicine, San Diego, CA; 2VA San Diego Healthcare System, San Diego, CA
Introduction: Although the Veterans Health Administration (VHA) has successfully cured the majority of chronic hepatitis C virus (HCV) infections following availability of direct-acting antiviral (DAA) therapy, a subset of veterans remains untreated. These individuals often face complex barriers, such as homelessness, substance use, psychiatric illness, and care fragmentation, that limit engagement in care. At the VA San Diego Healthcare System, we initiated a quality improvement (QI) project to systematically identify and re-engage veterans with untreated HCV.
Methods: Using the VA Liver Dashboard, we identified 88 veterans with documented HCV viremia and no record of antiviral treatment. Patients were contacted via mailed letters and follow-up phone calls. Electronic notifications were sent to primary care providers (PCPs), and Hepatology referrals were placed on behalf of 14 veterans lacking an assigned PCP. Appointments for liver disease staging with vibration controlled transient elastography (VCTE) were offered prior to hepatology consultation. Patients with hepatocellular carcinoma (n=4), HIV/HCV coinfection (n=2), or deceased after outreach (n=5) were excluded, leaving 77 eligible untreated veterans. 5 patients lacked valid contact information.
Results: 37/77 (48%) Veterans either answered phone calls or called in to schedule appointments after receiving a letter. 25/77 (32%) veterans scheduled VCTE appointments, 13 of whom completed VCTE examination. The median liver stiffness measured from VCTE was 6.7 kPa (range: 4.5–8.9), and the median FIB-4 score was 1.05 (range: 0.61-1.55). 8/13 (61.5%) have initiated DAA therapy, while the remaining 5 veterans have not followed up for treatment initiation. Among the 77 veterans who were included, 24 have a history of substance use disorder, 18 are experiencing homelessness, 5 have no valid mailing address or phone number, 2 are under conservatorship for psychiatric illnesses, and 30 have documented depression or anxiety.
Discussion: Despite national advances in HCV elimination, this QI initiative highlights the challenges of linking viremic veterans with significant psychosocial and structural barriers to care. Contributing factors include unstable housing, phone access, or care avoidance. Next steps will include 2-3 additional re-engagement efforts using mailed letters, PCP alerts, and follow-up phone calls. These targeted interventions will help inform broader strategies to close treatment gaps toward a goal of HCV elimination within the VA.
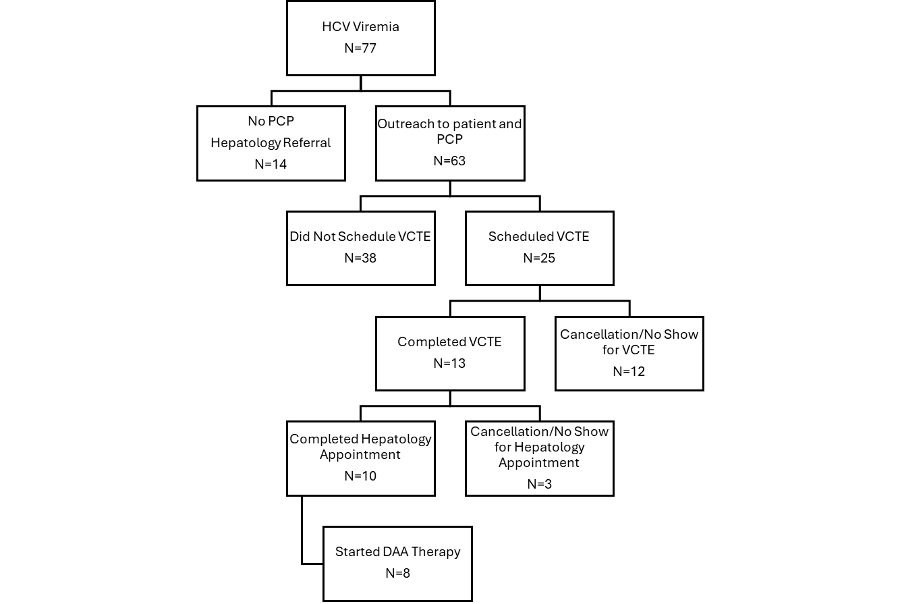
Figure: Figure 1. Flow diagram of intervention to link viremic Veterans to care. None of the Veterans lacking a primary care provider (PCP) were successfully scheduled for treatment evaluation.
Disclosures:
Janan Leppo indicated no relevant financial relationships.
Ann Deioma indicated no relevant financial relationships.
Heather Patton indicated no relevant financial relationships.
Janan D. Leppo, MD1, Ann Deioma, BSN, RN2, Heather Patton, MD2. P1560 - Targeting Health Equity in Hepatitis C Elimination: A Quality Improvement Initiative to Re-engage Marginalized Veterans, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1UC San Diego Department of Internal Medicine, San Diego, CA; 2VA San Diego Healthcare System, San Diego, CA
Introduction: Although the Veterans Health Administration (VHA) has successfully cured the majority of chronic hepatitis C virus (HCV) infections following availability of direct-acting antiviral (DAA) therapy, a subset of veterans remains untreated. These individuals often face complex barriers, such as homelessness, substance use, psychiatric illness, and care fragmentation, that limit engagement in care. At the VA San Diego Healthcare System, we initiated a quality improvement (QI) project to systematically identify and re-engage veterans with untreated HCV.
Methods: Using the VA Liver Dashboard, we identified 88 veterans with documented HCV viremia and no record of antiviral treatment. Patients were contacted via mailed letters and follow-up phone calls. Electronic notifications were sent to primary care providers (PCPs), and Hepatology referrals were placed on behalf of 14 veterans lacking an assigned PCP. Appointments for liver disease staging with vibration controlled transient elastography (VCTE) were offered prior to hepatology consultation. Patients with hepatocellular carcinoma (n=4), HIV/HCV coinfection (n=2), or deceased after outreach (n=5) were excluded, leaving 77 eligible untreated veterans. 5 patients lacked valid contact information.
Results: 37/77 (48%) Veterans either answered phone calls or called in to schedule appointments after receiving a letter. 25/77 (32%) veterans scheduled VCTE appointments, 13 of whom completed VCTE examination. The median liver stiffness measured from VCTE was 6.7 kPa (range: 4.5–8.9), and the median FIB-4 score was 1.05 (range: 0.61-1.55). 8/13 (61.5%) have initiated DAA therapy, while the remaining 5 veterans have not followed up for treatment initiation. Among the 77 veterans who were included, 24 have a history of substance use disorder, 18 are experiencing homelessness, 5 have no valid mailing address or phone number, 2 are under conservatorship for psychiatric illnesses, and 30 have documented depression or anxiety.
Discussion: Despite national advances in HCV elimination, this QI initiative highlights the challenges of linking viremic veterans with significant psychosocial and structural barriers to care. Contributing factors include unstable housing, phone access, or care avoidance. Next steps will include 2-3 additional re-engagement efforts using mailed letters, PCP alerts, and follow-up phone calls. These targeted interventions will help inform broader strategies to close treatment gaps toward a goal of HCV elimination within the VA.
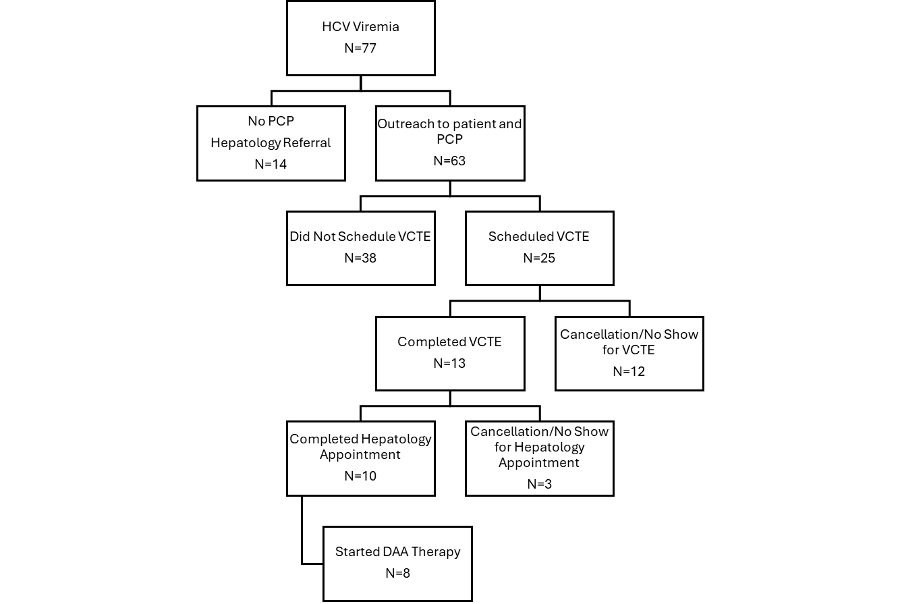
Figure: Figure 1. Flow diagram of intervention to link viremic Veterans to care. None of the Veterans lacking a primary care provider (PCP) were successfully scheduled for treatment evaluation.
Disclosures:
Janan Leppo indicated no relevant financial relationships.
Ann Deioma indicated no relevant financial relationships.
Heather Patton indicated no relevant financial relationships.
Janan D. Leppo, MD1, Ann Deioma, BSN, RN2, Heather Patton, MD2. P1560 - Targeting Health Equity in Hepatitis C Elimination: A Quality Improvement Initiative to Re-engage Marginalized Veterans, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
