Sunday Poster Session
Category: Liver
P1557 - Alcohol Use Disorder (AUD): A Quality Improvement Initiative to Improve Naltrexone Prescription Patterns and Readmissions Rates in Patients With AUD
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Abhishek Alur, MD, MBA (he/him/his)
Loyola University Medical Center
Chicago, IL
Presenting Author(s)
Abhishek Alur, MD, MBA1, Dinkar Ahuja, MD1, Mohammad Abourahma, MD2, Bruce Guay, MD3
1Loyola University Medical Center, Chicago, IL; 2Loyola University Medical Center, Maywood, IL; 3Edward Hines Jr. Veterans Affairs Hospital, Hines, IL
Introduction: Alcohol use disorder (AUD) remains one of the most prevalent mental health conditions in the United States. AUD is the third leading cause of preventable death in the U.S, costing over $5 billion from AUD-related hospitalizations. Studies have shown that alcohol cessation medications (ACMs), such as naltrexone and acamprosate, can significantly reduce readmissions over short and long-term follow-up. At the Hines Veterans Affairs (HVA), a large portion of patients with AUD are not prescribed ACMs. To address this treatment gap, we implemented a quality improvement initiative on inpatient general medicine (GM) teams focused on prescribing naltrexone to patients with AUD and assessing the impact on 90-day readmission rates.
Methods: A pre-intervention group included inpatients with AUD related admissions (e.g., withdrawal, alcohol-related pancreatitis, or injury related to intoxication) over the month of July 2024 on two GM teams at the HVA and 90-day readmissions were recorded. The intervention group included similar AUD patients and occurred on the same two GM teams between September 15, 2024, and January 15, 2025. Internal medicine residents were trained on naltrexone efficacy and safety during bi-monthly GM orientation and GM team pharmacists helped prompt teams on evaluation of AUD patient eligibility for initiation of naltrexone at discharge. Patient data and 90-day readmissions were recorded.
Results: The pre-intervention group had 10 patients with 17 total readmissions over 90-days. The intervention group (n=24 patients, 22 total readmissions) had a 46% lower 90-day readmission rate compared to the pre-intervention group (0.92 vs 1.7 readmissions per patient over 90-days; rate ratio = 0.54, p = 0.052). One patient in the intervention group accounted for eight of 22 total readmissions. 15 patients (63%) in the intervention group had zero readmissions. Only 10 patients (42%) agreed to and received naltrexone at discharge. Psychiatry was consulted during 22 patients' (92%) initial admissions.
Discussion: The intervention group had fewer 90-day readmissions despite less than half of the patients receiving naltrexone, suggesting the QI intervention may have motivated behavior change. Psychiatry involvement and coordination of follow-up including month long rehabilitation stays, which may have enhanced our interventions' effectiveness. Limitations include small sample size, limited readmission tracking to the HVA system only, and sustained alcohol cessation was not assessed.
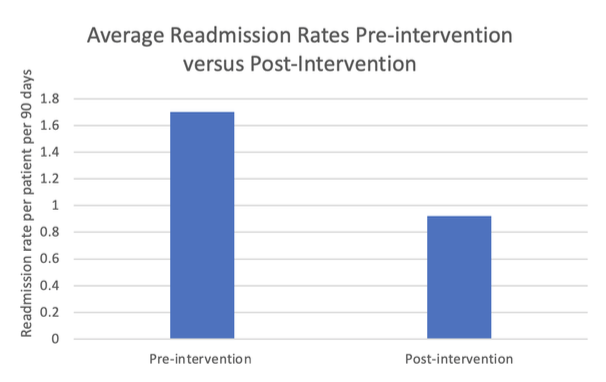
Figure: Chart 1. Demonstrates average readmission rate per patient over 90- day windows in pre-intervention group (1.7 readmissions per 90-days) was greater than post-intervention group (0.92 readmissions per 90- days).
Disclosures:
Abhishek Alur indicated no relevant financial relationships.
Dinkar Ahuja indicated no relevant financial relationships.
Mohammad Abourahma indicated no relevant financial relationships.
Bruce Guay indicated no relevant financial relationships.
Abhishek Alur, MD, MBA1, Dinkar Ahuja, MD1, Mohammad Abourahma, MD2, Bruce Guay, MD3. P1557 - Alcohol Use Disorder (AUD): A Quality Improvement Initiative to Improve Naltrexone Prescription Patterns and Readmissions Rates in Patients With AUD, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Loyola University Medical Center, Chicago, IL; 2Loyola University Medical Center, Maywood, IL; 3Edward Hines Jr. Veterans Affairs Hospital, Hines, IL
Introduction: Alcohol use disorder (AUD) remains one of the most prevalent mental health conditions in the United States. AUD is the third leading cause of preventable death in the U.S, costing over $5 billion from AUD-related hospitalizations. Studies have shown that alcohol cessation medications (ACMs), such as naltrexone and acamprosate, can significantly reduce readmissions over short and long-term follow-up. At the Hines Veterans Affairs (HVA), a large portion of patients with AUD are not prescribed ACMs. To address this treatment gap, we implemented a quality improvement initiative on inpatient general medicine (GM) teams focused on prescribing naltrexone to patients with AUD and assessing the impact on 90-day readmission rates.
Methods: A pre-intervention group included inpatients with AUD related admissions (e.g., withdrawal, alcohol-related pancreatitis, or injury related to intoxication) over the month of July 2024 on two GM teams at the HVA and 90-day readmissions were recorded. The intervention group included similar AUD patients and occurred on the same two GM teams between September 15, 2024, and January 15, 2025. Internal medicine residents were trained on naltrexone efficacy and safety during bi-monthly GM orientation and GM team pharmacists helped prompt teams on evaluation of AUD patient eligibility for initiation of naltrexone at discharge. Patient data and 90-day readmissions were recorded.
Results: The pre-intervention group had 10 patients with 17 total readmissions over 90-days. The intervention group (n=24 patients, 22 total readmissions) had a 46% lower 90-day readmission rate compared to the pre-intervention group (0.92 vs 1.7 readmissions per patient over 90-days; rate ratio = 0.54, p = 0.052). One patient in the intervention group accounted for eight of 22 total readmissions. 15 patients (63%) in the intervention group had zero readmissions. Only 10 patients (42%) agreed to and received naltrexone at discharge. Psychiatry was consulted during 22 patients' (92%) initial admissions.
Discussion: The intervention group had fewer 90-day readmissions despite less than half of the patients receiving naltrexone, suggesting the QI intervention may have motivated behavior change. Psychiatry involvement and coordination of follow-up including month long rehabilitation stays, which may have enhanced our interventions' effectiveness. Limitations include small sample size, limited readmission tracking to the HVA system only, and sustained alcohol cessation was not assessed.
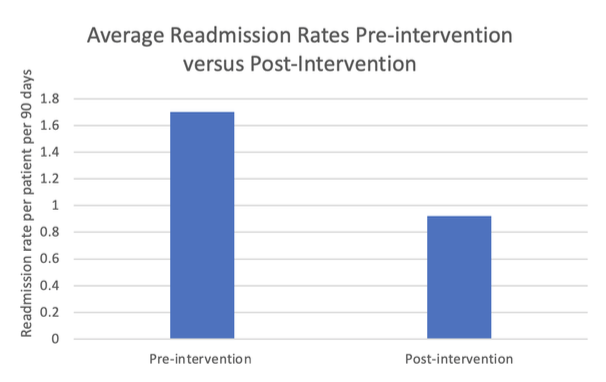
Figure: Chart 1. Demonstrates average readmission rate per patient over 90- day windows in pre-intervention group (1.7 readmissions per 90-days) was greater than post-intervention group (0.92 readmissions per 90- days).
Disclosures:
Abhishek Alur indicated no relevant financial relationships.
Dinkar Ahuja indicated no relevant financial relationships.
Mohammad Abourahma indicated no relevant financial relationships.
Bruce Guay indicated no relevant financial relationships.
Abhishek Alur, MD, MBA1, Dinkar Ahuja, MD1, Mohammad Abourahma, MD2, Bruce Guay, MD3. P1557 - Alcohol Use Disorder (AUD): A Quality Improvement Initiative to Improve Naltrexone Prescription Patterns and Readmissions Rates in Patients With AUD, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
