Sunday Poster Session
Category: Liver
P1555 - Risk of Gastrointestinal Malignancies in Patients With Metabolic Dysfunction-Associated Steatotic Liver Disease: A US-based Propensity Matched Cohort Study
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Rishi Chowdhary, MD (he/him/his)
Case Western Reserve University / MetroHealth
Cleveland, OH
Presenting Author(s)
Rishi Chowdhary, MD1, Harsh Vadnagara, MBBS2, Dhruv Gandhi, MD3, Thai Hau Koo, MD4, Rohit Goyal, MD5, Arshia Sethi, 6, Kirti Arora, 7, Rakshand Shetty, MBBS8, Venkata Sunkesula, MD1
1Case Western Reserve University / MetroHealth, Cleveland, OH; 2BJ Medical College, Cleveland, OH; 3St Francis Medical Center, Monroe, LA, Mumbai, Maharashtra, India; 4University of Sciences Malaysia Specialist Hospital, Kelantan, Kelantan, Malaysia; 5Louisiana State University, Shreveport, LA; 6Icahn School of Medicine at Mount Sinai, New York, NY; 7Cleveland Clinic Akron General, Akron, OH; 8Kasturba Medical College of Manipal, Brahmavara, Karnataka, India
Introduction: Metabolic dysfunction-associated steatotic liver disease (MASLD) is the most prevalent chronic liver disease globally and is increasingly linked to extrahepatic malignancies. While its association with hepatocellular carcinoma is well established, its role in gastrointestinal (GI) cancers remains underexplored. This study assessed the risk of site-specific gastrointestinal (GI) malignancies in patients with MASLD, including an age-stratified analysis across all cancer sites.
Methods: We conducted a retrospective cohort study using TriNetX, a federated electronic health record network spanning 69 U.S. healthcare organizations. Adults (≥18 years) diagnosed with MASLD (ICD-10: K75.81, K76.0) between 2010–2020, confirmed by abdominal imaging, were included. Patients with viral hepatitis, alcohol-related liver disease, autoimmune hepatitis, HIV, solid organ transplant, or prior malignancy were excluded. Propensity score matching (1:1) was performed using demographic, metabolic, and clinical comorbidities to create well-balanced MASLD and non-MASLD cohorts (n=360,650 each). Primary outcomes included incident esophageal, gastric, small intestinal, colorectal, gallbladder, and pancreatic cancers. Age-stratified analyses were performed within the MASLD cohort.
Results: MASLD was independently associated with increased risk of colorectal (OR 1.20; 95% CI: 1.12–1.29), gastric (OR 1.34; 95% CI: 1.15–1.55), pancreatic (OR 1.36; 95% CI: 1.24–1.49), small intestinal (OR 1.26; 95% CI: 1.02–1.55), and gallbladder (OR 1.46; 95% CI: 1.22–1.75) cancers (all p< 0.05), with no significant association for esophageal cancer (OR 0.98; 95% CI: 0.82–1.18; p=0.86). MASLD also conferred a 30% increased time-dependent risk of malignancy (HR 1.30; 95% CI: 1.29–1.31; p< 0.001).
In age-stratified analysis, MASLD patients >50 years had significantly higher odds of gastric (OR 4.77; 95% CI: 3.28–6.94), colorectal (OR 4.69; 95% CI: 3.95–5.56), small intestinal (OR 3.43; 95% CI: 2.11–5.58), gallbladder (OR 4.05; 95% CI: 3.78–10.52), and pancreatic cancers (OR 8.61; 95% CI: 6.35–11.69) compared to those ≤50 (all p< 0.001).
Discussion: MASLD is independently associated with elevated risk of multiple GI malignancies, especially colorectal, pancreatic, and gallbladder cancers. The pronounced age-related risk gradient underscores the need for risk-adapted surveillance, repositioning MASLD as a systemic condition with meaningful oncologic implications.
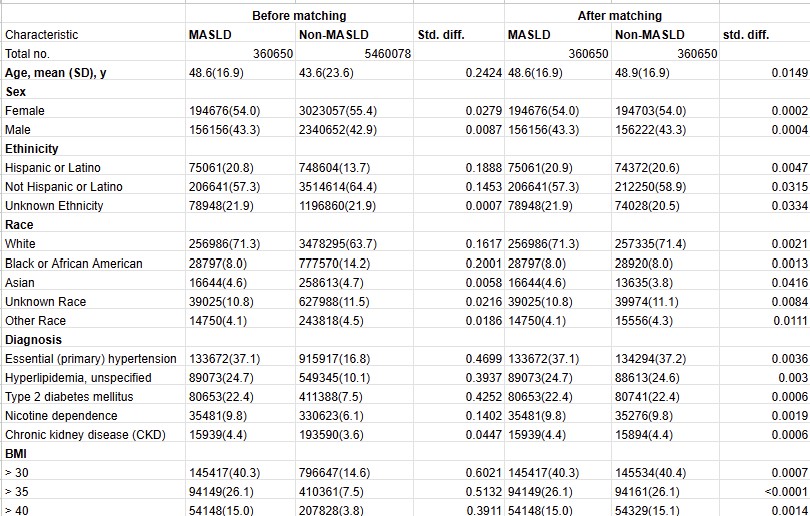
Figure: Forest Plots Showing Overall and Age-Stratified Risk of Gastrointestinal Malignancies in MASLD Patients compared to the Non-MASLD population
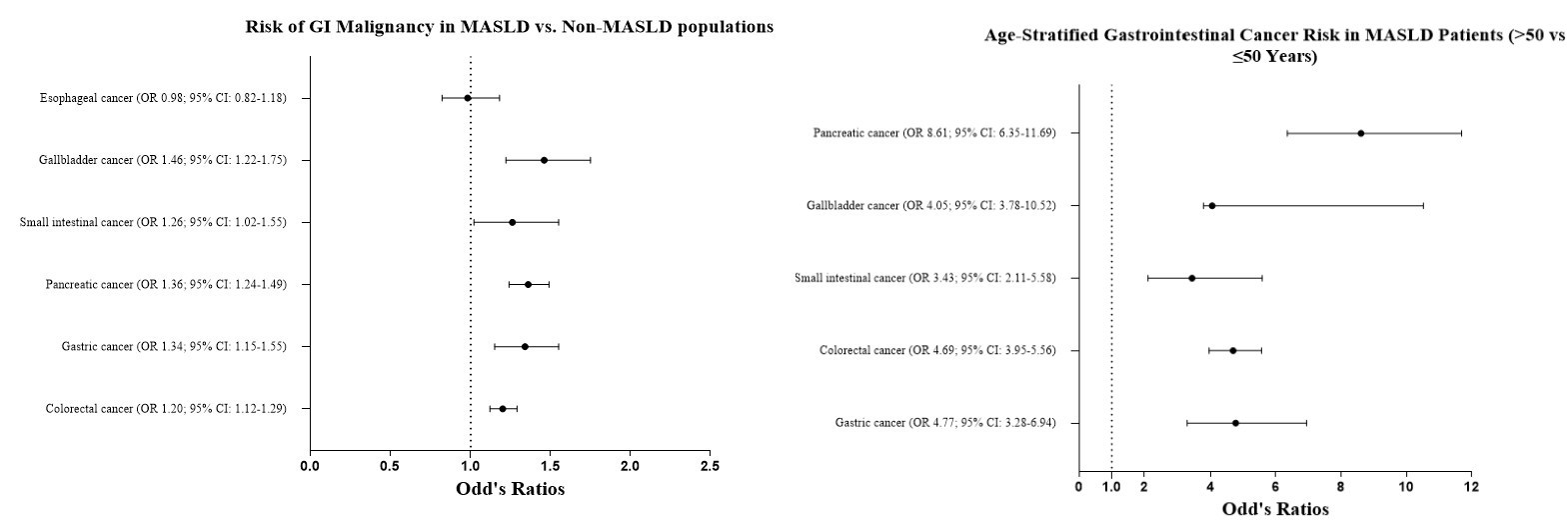
Figure: Baseline Demographics, Comorbidities, and BMI in Patients With and Without MASLD Before and After Propensity Score Matching
Disclosures:
Rishi Chowdhary indicated no relevant financial relationships.
Harsh Vadnagara indicated no relevant financial relationships.
Dhruv Gandhi indicated no relevant financial relationships.
Thai Hau Koo indicated no relevant financial relationships.
Rohit Goyal indicated no relevant financial relationships.
Arshia Sethi indicated no relevant financial relationships.
Kirti Arora indicated no relevant financial relationships.
Rakshand Shetty indicated no relevant financial relationships.
Venkata Sunkesula indicated no relevant financial relationships.
Rishi Chowdhary, MD1, Harsh Vadnagara, MBBS2, Dhruv Gandhi, MD3, Thai Hau Koo, MD4, Rohit Goyal, MD5, Arshia Sethi, 6, Kirti Arora, 7, Rakshand Shetty, MBBS8, Venkata Sunkesula, MD1. P1555 - Risk of Gastrointestinal Malignancies in Patients With Metabolic Dysfunction-Associated Steatotic Liver Disease: A US-based Propensity Matched Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Case Western Reserve University / MetroHealth, Cleveland, OH; 2BJ Medical College, Cleveland, OH; 3St Francis Medical Center, Monroe, LA, Mumbai, Maharashtra, India; 4University of Sciences Malaysia Specialist Hospital, Kelantan, Kelantan, Malaysia; 5Louisiana State University, Shreveport, LA; 6Icahn School of Medicine at Mount Sinai, New York, NY; 7Cleveland Clinic Akron General, Akron, OH; 8Kasturba Medical College of Manipal, Brahmavara, Karnataka, India
Introduction: Metabolic dysfunction-associated steatotic liver disease (MASLD) is the most prevalent chronic liver disease globally and is increasingly linked to extrahepatic malignancies. While its association with hepatocellular carcinoma is well established, its role in gastrointestinal (GI) cancers remains underexplored. This study assessed the risk of site-specific gastrointestinal (GI) malignancies in patients with MASLD, including an age-stratified analysis across all cancer sites.
Methods: We conducted a retrospective cohort study using TriNetX, a federated electronic health record network spanning 69 U.S. healthcare organizations. Adults (≥18 years) diagnosed with MASLD (ICD-10: K75.81, K76.0) between 2010–2020, confirmed by abdominal imaging, were included. Patients with viral hepatitis, alcohol-related liver disease, autoimmune hepatitis, HIV, solid organ transplant, or prior malignancy were excluded. Propensity score matching (1:1) was performed using demographic, metabolic, and clinical comorbidities to create well-balanced MASLD and non-MASLD cohorts (n=360,650 each). Primary outcomes included incident esophageal, gastric, small intestinal, colorectal, gallbladder, and pancreatic cancers. Age-stratified analyses were performed within the MASLD cohort.
Results: MASLD was independently associated with increased risk of colorectal (OR 1.20; 95% CI: 1.12–1.29), gastric (OR 1.34; 95% CI: 1.15–1.55), pancreatic (OR 1.36; 95% CI: 1.24–1.49), small intestinal (OR 1.26; 95% CI: 1.02–1.55), and gallbladder (OR 1.46; 95% CI: 1.22–1.75) cancers (all p< 0.05), with no significant association for esophageal cancer (OR 0.98; 95% CI: 0.82–1.18; p=0.86). MASLD also conferred a 30% increased time-dependent risk of malignancy (HR 1.30; 95% CI: 1.29–1.31; p< 0.001).
In age-stratified analysis, MASLD patients >50 years had significantly higher odds of gastric (OR 4.77; 95% CI: 3.28–6.94), colorectal (OR 4.69; 95% CI: 3.95–5.56), small intestinal (OR 3.43; 95% CI: 2.11–5.58), gallbladder (OR 4.05; 95% CI: 3.78–10.52), and pancreatic cancers (OR 8.61; 95% CI: 6.35–11.69) compared to those ≤50 (all p< 0.001).
Discussion: MASLD is independently associated with elevated risk of multiple GI malignancies, especially colorectal, pancreatic, and gallbladder cancers. The pronounced age-related risk gradient underscores the need for risk-adapted surveillance, repositioning MASLD as a systemic condition with meaningful oncologic implications.
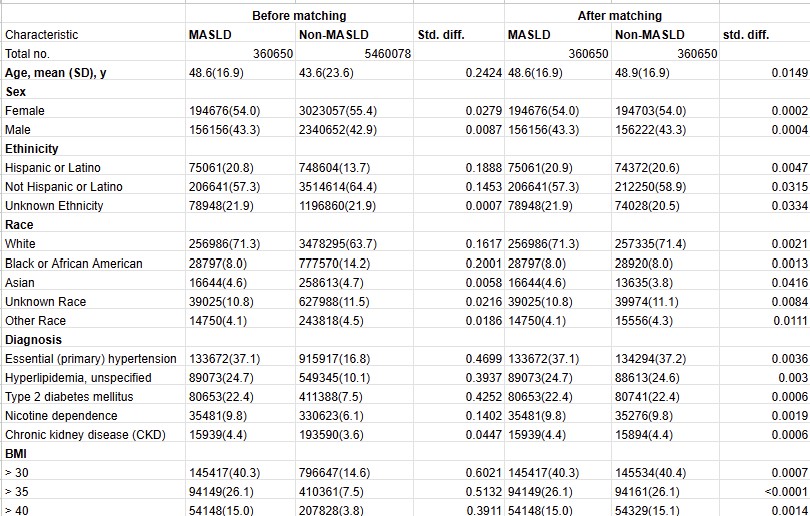
Figure: Forest Plots Showing Overall and Age-Stratified Risk of Gastrointestinal Malignancies in MASLD Patients compared to the Non-MASLD population
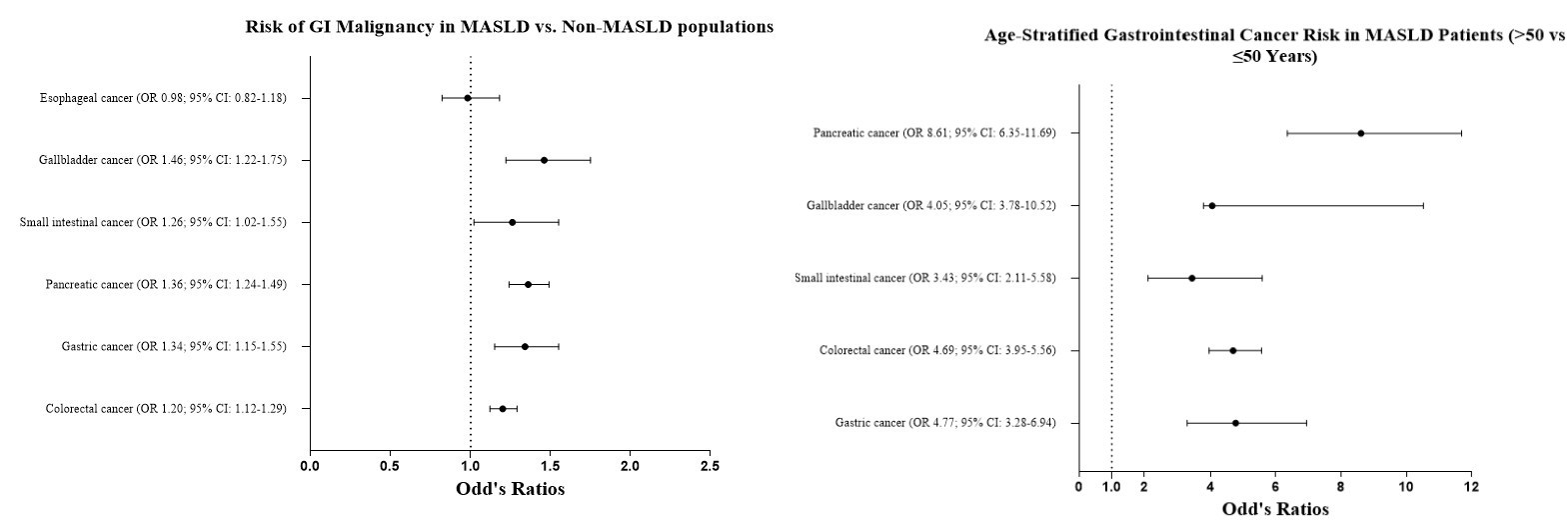
Figure: Baseline Demographics, Comorbidities, and BMI in Patients With and Without MASLD Before and After Propensity Score Matching
Disclosures:
Rishi Chowdhary indicated no relevant financial relationships.
Harsh Vadnagara indicated no relevant financial relationships.
Dhruv Gandhi indicated no relevant financial relationships.
Thai Hau Koo indicated no relevant financial relationships.
Rohit Goyal indicated no relevant financial relationships.
Arshia Sethi indicated no relevant financial relationships.
Kirti Arora indicated no relevant financial relationships.
Rakshand Shetty indicated no relevant financial relationships.
Venkata Sunkesula indicated no relevant financial relationships.
Rishi Chowdhary, MD1, Harsh Vadnagara, MBBS2, Dhruv Gandhi, MD3, Thai Hau Koo, MD4, Rohit Goyal, MD5, Arshia Sethi, 6, Kirti Arora, 7, Rakshand Shetty, MBBS8, Venkata Sunkesula, MD1. P1555 - Risk of Gastrointestinal Malignancies in Patients With Metabolic Dysfunction-Associated Steatotic Liver Disease: A US-based Propensity Matched Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
