Sunday Poster Session
Category: Liver
P1545 - Optimizing Non-Selective Beta-Blocker Use Among Patients with Compensated Advanced Chronic Liver Disease
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Jameel Alp, MD (he/him/his)
University of Minnesota
Minneapolis, MN
Presenting Author(s)
Jameel Alp, MD1, Nirjhar Dutta, DO, MS2, Susan Lou, MD3, Brian Hanson, MD3, Prowpanga Udompap, MD3
1University of Minnesota, Minneapolis, MN; 2University of Minnesota Medical School, Minneapolis, MN; 3University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN
Introduction: Non-selective beta-blockers (NSBB), especially carvedilol, have been shown to reduce the risk of hepatic decompensation in patients with compensated advanced chronic liver disease (cACLD) and clinically significant portal hypertension (CSPH). Liver stiffness (LS) measured by vibration-controlled transient elastography (VCTE), along with platelet count (plt), can be used to identify patients with cACLD and CSPH; in other words, those eligible for NSBB in whom screening esophagogastroduodenoscopy (EGD) for esophageal varices (EV) may be safely forgone. However, it is unclear whether this recent change in recommendations has been adopted in clinical practice. We aimed to determine the proportion of EGDs for EV screening among patients with cACLD that could potentially be avoided, as well as the current rate of NSBB use.
Methods: We identified patients with cACLD who underwent EGD for EV screening at the Minneapolis VA Medical Center between October 1, 2023, and September 30, 2024. CSPH was defined based on imaging evidence of portal hypertension or by LS on VCTE and plt as follows: LS ≥25 kPa; or LS 15-20 kPa with plt < 110 x10^3/uL; or LS 20-25 kPa with plt < 150 x10^3/uL. We assessed NSBB eligibility, presence of EV, and contraindications to NSBB. Trends in NSBB use were compared before and after May 2024, when the updated recommendations from the American Association for the Study of Liver Diseases were published.
Results: Among 71 patients with cACLD who underwent EGD for EV screening, 78.7% had CSPH, but only 12.6% of these were identified using VCTE and plt. Overall, 64.7% of patients were eligible for NSBB, while 14% had contraindications, making EGD appropriate in those cases. No patients had EV requiring intervention. Comparison of NSBB utilization before and after May 2024 showed no significant change.
Discussion: The results of this study highlight a gap between updated clinical recommendations and their adoption in real-world practice. None of the patients who underwent EGD had EV requiring intervention, and more than two-thirds of these procedures could have been avoided with appropriate NSBB initiation. Our findings highlight the opportunity to increase the use of VCTE and NSBB in the appropriate clinical context.
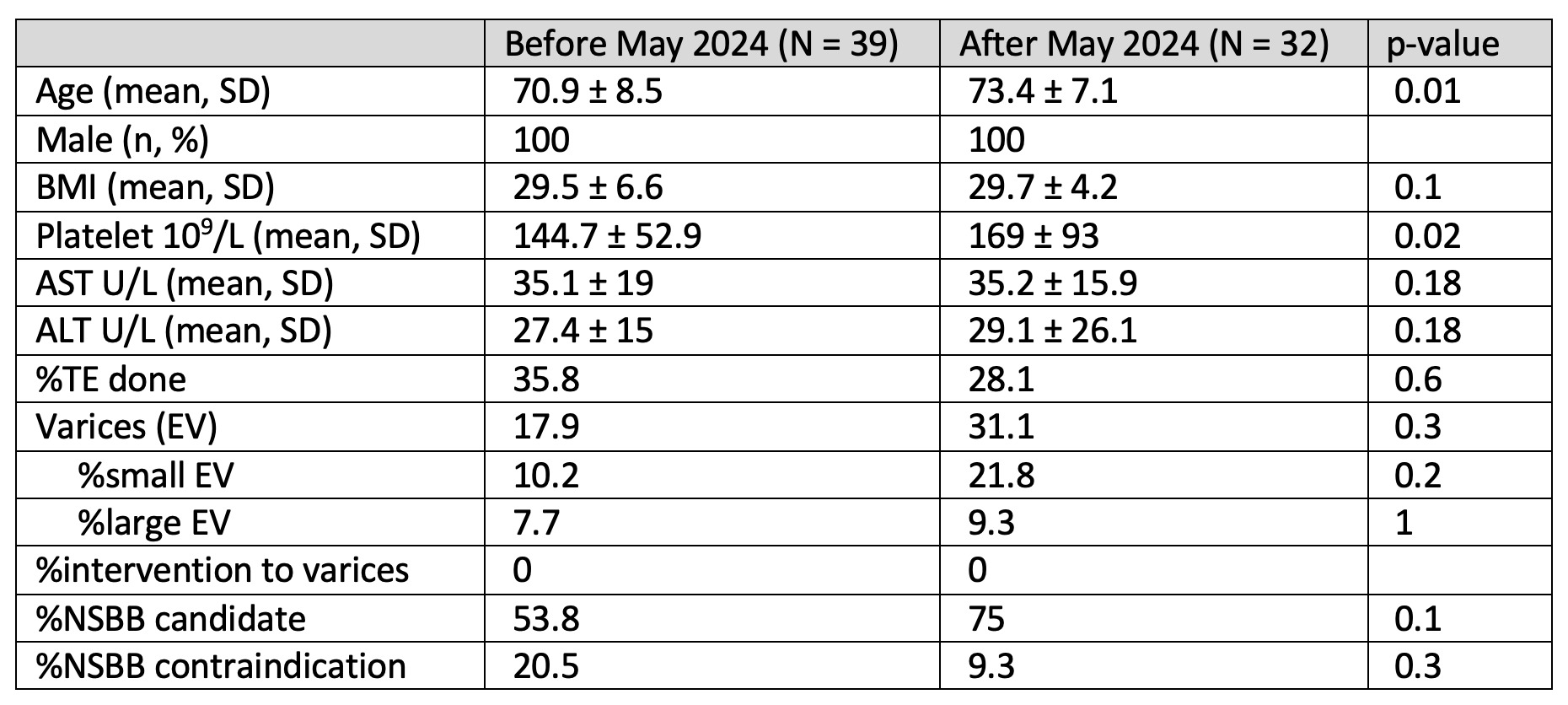
Figure: Table 1. Comparison of patient characteristics, diagnostic practices, and management outcomes for individuals who underwent EGD for EV screening before and after the publication of the AASLD guidance on risk stratification and management of portal hypertension and varices in cirrhosis in May 2024.
Disclosures:
Jameel Alp indicated no relevant financial relationships.
Nirjhar Dutta indicated no relevant financial relationships.
Susan Lou indicated no relevant financial relationships.
Brian Hanson indicated no relevant financial relationships.
Prowpanga Udompap indicated no relevant financial relationships.
Jameel Alp, MD1, Nirjhar Dutta, DO, MS2, Susan Lou, MD3, Brian Hanson, MD3, Prowpanga Udompap, MD3. P1545 - Optimizing Non-Selective Beta-Blocker Use Among Patients with Compensated Advanced Chronic Liver Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Minnesota, Minneapolis, MN; 2University of Minnesota Medical School, Minneapolis, MN; 3University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN
Introduction: Non-selective beta-blockers (NSBB), especially carvedilol, have been shown to reduce the risk of hepatic decompensation in patients with compensated advanced chronic liver disease (cACLD) and clinically significant portal hypertension (CSPH). Liver stiffness (LS) measured by vibration-controlled transient elastography (VCTE), along with platelet count (plt), can be used to identify patients with cACLD and CSPH; in other words, those eligible for NSBB in whom screening esophagogastroduodenoscopy (EGD) for esophageal varices (EV) may be safely forgone. However, it is unclear whether this recent change in recommendations has been adopted in clinical practice. We aimed to determine the proportion of EGDs for EV screening among patients with cACLD that could potentially be avoided, as well as the current rate of NSBB use.
Methods: We identified patients with cACLD who underwent EGD for EV screening at the Minneapolis VA Medical Center between October 1, 2023, and September 30, 2024. CSPH was defined based on imaging evidence of portal hypertension or by LS on VCTE and plt as follows: LS ≥25 kPa; or LS 15-20 kPa with plt < 110 x10^3/uL; or LS 20-25 kPa with plt < 150 x10^3/uL. We assessed NSBB eligibility, presence of EV, and contraindications to NSBB. Trends in NSBB use were compared before and after May 2024, when the updated recommendations from the American Association for the Study of Liver Diseases were published.
Results: Among 71 patients with cACLD who underwent EGD for EV screening, 78.7% had CSPH, but only 12.6% of these were identified using VCTE and plt. Overall, 64.7% of patients were eligible for NSBB, while 14% had contraindications, making EGD appropriate in those cases. No patients had EV requiring intervention. Comparison of NSBB utilization before and after May 2024 showed no significant change.
Discussion: The results of this study highlight a gap between updated clinical recommendations and their adoption in real-world practice. None of the patients who underwent EGD had EV requiring intervention, and more than two-thirds of these procedures could have been avoided with appropriate NSBB initiation. Our findings highlight the opportunity to increase the use of VCTE and NSBB in the appropriate clinical context.
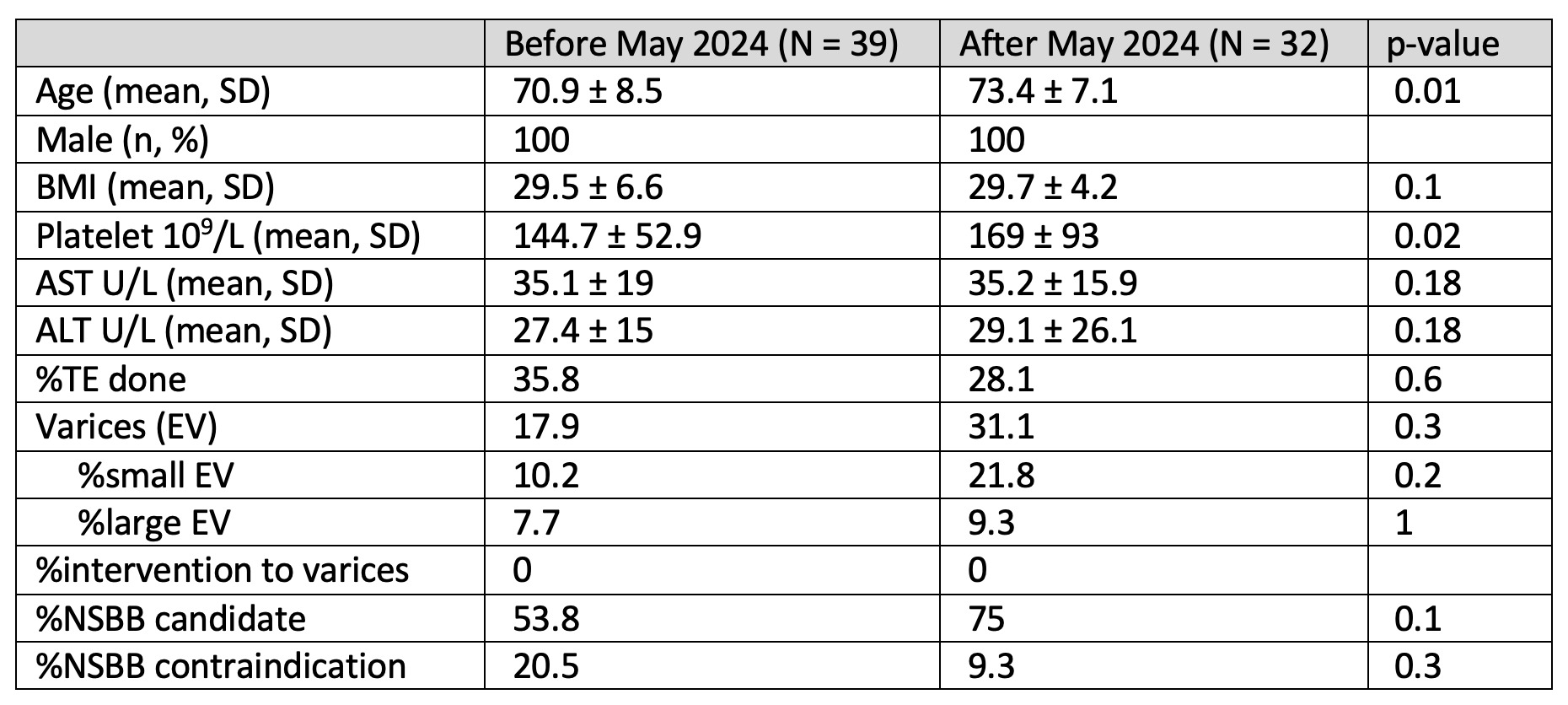
Figure: Table 1. Comparison of patient characteristics, diagnostic practices, and management outcomes for individuals who underwent EGD for EV screening before and after the publication of the AASLD guidance on risk stratification and management of portal hypertension and varices in cirrhosis in May 2024.
Disclosures:
Jameel Alp indicated no relevant financial relationships.
Nirjhar Dutta indicated no relevant financial relationships.
Susan Lou indicated no relevant financial relationships.
Brian Hanson indicated no relevant financial relationships.
Prowpanga Udompap indicated no relevant financial relationships.
Jameel Alp, MD1, Nirjhar Dutta, DO, MS2, Susan Lou, MD3, Brian Hanson, MD3, Prowpanga Udompap, MD3. P1545 - Optimizing Non-Selective Beta-Blocker Use Among Patients with Compensated Advanced Chronic Liver Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
