Sunday Poster Session
Category: Liver
P1654 - Effect of Thromboembolic Events on Long-Term Treatment Outcomes in Liver Cirrhosis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- MB
Martin Banks, MD
Bayhealth Medical Center - - Dover, DE
Dover, DE
Presenting Author(s)
Martin Banks, MD1, Adaobi Ahanotu, MD2, Rand Alkalbani, MD3, Farhan Azad, DO3, Kelly M. Vo, DO4, Amolika Gupta, MD5, Marwan S. Abougergi, MD6
1Bayhealth Medical Center - - Dover, DE, Dover, DE; 2University of Maryland Medical Center, Hyattsville, MD; 3INOVA Fairfax Hospital, Fairfax, VA; 4Walter Reed National Military Medical Center, Bethesda, MD; 5Inova Fairfax Medical Campus, Vienna, VA; 6INOVA Fairfax Hospital, Falls Church, VA
Introduction: Liver cirrhosis can be associated with a hypercoagulable state, which in turn can result in deep venous thrombosis (DVT), pulmonary embolism (PE) or portal vein thrombosis (PVT). These conditions alter circulatory hemodynamics and thus the disease course. They also present a treatment dilemma due to the cirrhosis-related risk of variceal hemorrhage. No national study to date has examined the long-term outcome of this patient population.
Methods: All patients admitted with liver cirrhosis in the United States in January were identified from 2016 to 2022 through the National Readmission Database. Patients with a principal diagnosis of either DVT/PE or PVT were identified. The follow-up period was 12 months. The primary outcome was liver decompensation. The secondary outcomes were 1-year mortality, incidence of esophageal or gastric varices, variceal hemorrhage, ascites, hepatic encephalopathy, acute liver failure and liver transplantation. Diagnoses were identified using ICD-10 CM codes. Logistic regression models were used to adjust for confounders, which were age, sex, income in the patient’s zipcode, insurance type, Charlson score and hospital bedsize, teaching status and urban location.
Results: 365,848 patients were included in the study. Of those, 1,767 patients had a DVT/PE and 695 had PVT. Table 1 presents the patient’s characteristics. The mean age was 61 years. The majority of patients were males, of lower income, insured by Medicare or Medicaid, and treated at large urban non-teaching hospitals. The adjusted odds ratios are presented in Table 2. Compared with patients without thromboembolism, patients with DVT/PE had lower adjusted odds of all-cause mortality, new ascites development and incident liver decompensation. On the other hand, PVT was associated with almost 3-fold increase in the adjusted odds of both new gastric or esophageal varices and variceal hemorrhage as well as 50% increase in the adjusted odds of acute liver failure. The three patient groups had similar adjusted odds of liver transplantation and incident hepatic encephalopathy.
Discussion: The development of DVT/PE is not associated with worsening outcomes among patients with liver cirrhosis and seems to be protective against liver decompensation and 1-year mortality. On the other hand, portal vein thrombosis is associated with a substantial increase in the risk of varices, variceal hemorrhage and acute liver failure. These finding can help guide follow-up frequency and prognosis discussion in this setting.
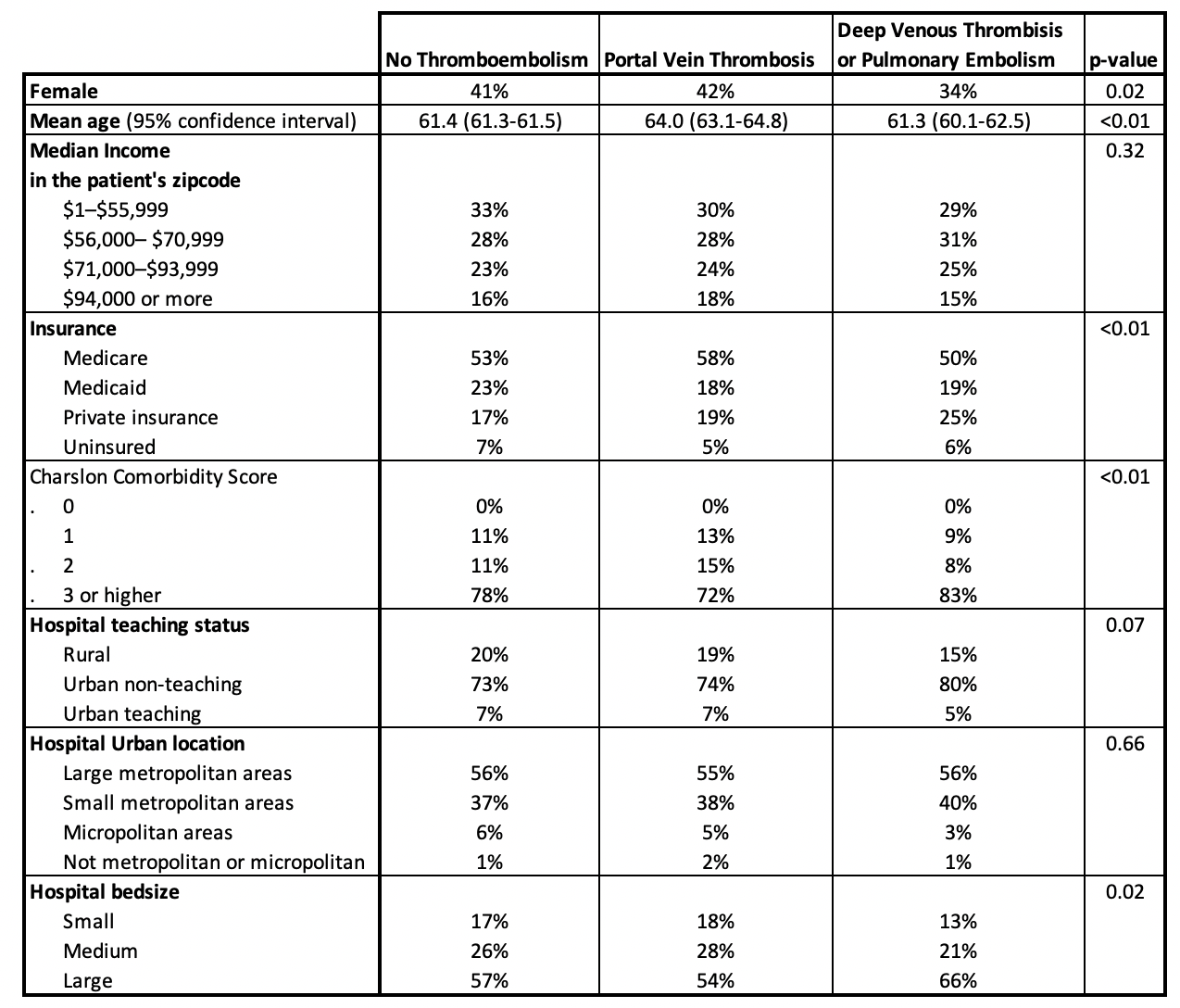
Figure: Table 1: Patient's Characteristics
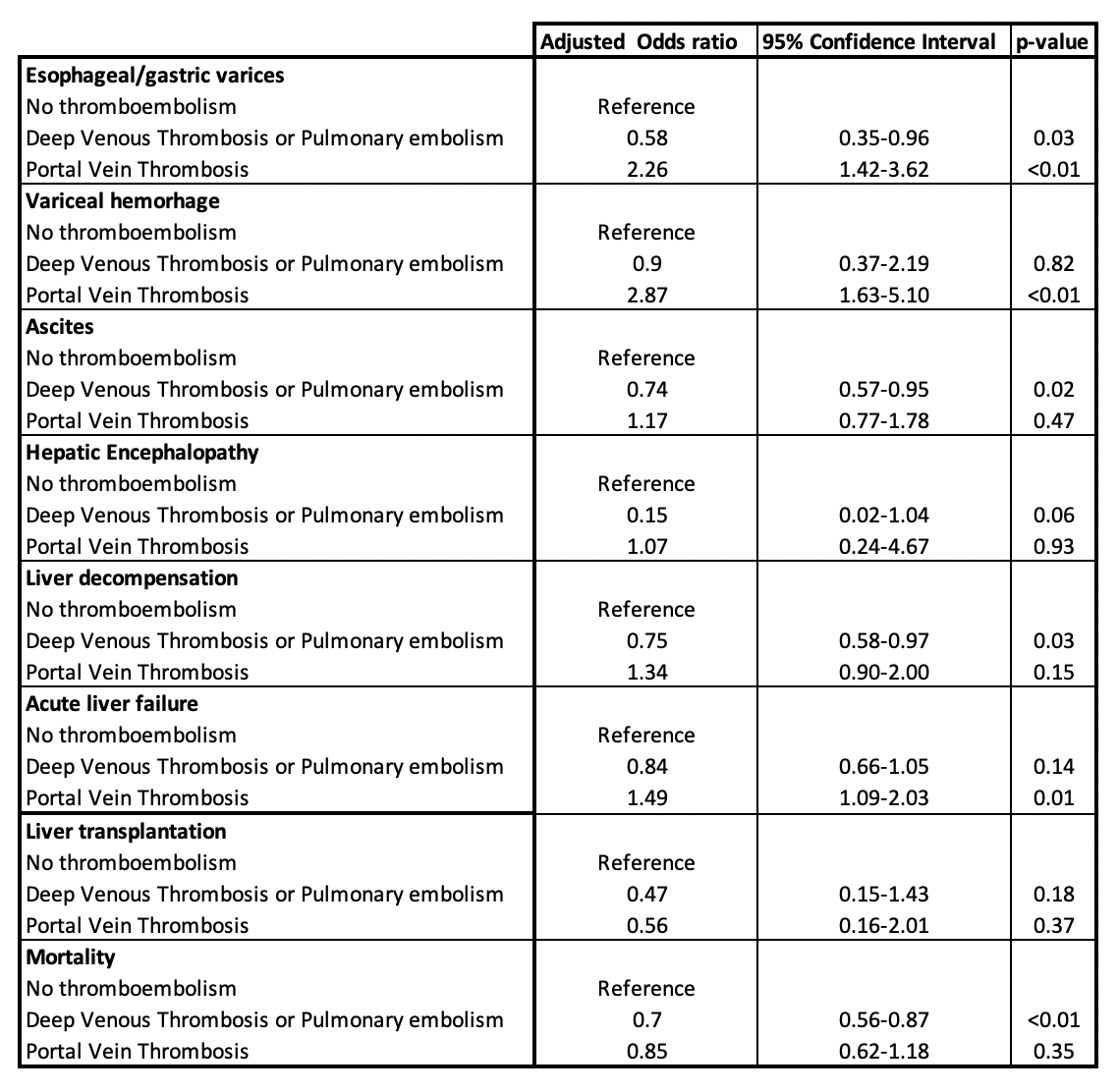
Figure: Table 2: Study Outcomes
Disclosures:
Martin Banks indicated no relevant financial relationships.
Adaobi Ahanotu indicated no relevant financial relationships.
Rand Alkalbani indicated no relevant financial relationships.
Farhan Azad indicated no relevant financial relationships.
Kelly Vo indicated no relevant financial relationships.
Amolika Gupta indicated no relevant financial relationships.
Marwan Abougergi indicated no relevant financial relationships.
Martin Banks, MD1, Adaobi Ahanotu, MD2, Rand Alkalbani, MD3, Farhan Azad, DO3, Kelly M. Vo, DO4, Amolika Gupta, MD5, Marwan S. Abougergi, MD6. P1654 - Effect of Thromboembolic Events on Long-Term Treatment Outcomes in Liver Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Bayhealth Medical Center - - Dover, DE, Dover, DE; 2University of Maryland Medical Center, Hyattsville, MD; 3INOVA Fairfax Hospital, Fairfax, VA; 4Walter Reed National Military Medical Center, Bethesda, MD; 5Inova Fairfax Medical Campus, Vienna, VA; 6INOVA Fairfax Hospital, Falls Church, VA
Introduction: Liver cirrhosis can be associated with a hypercoagulable state, which in turn can result in deep venous thrombosis (DVT), pulmonary embolism (PE) or portal vein thrombosis (PVT). These conditions alter circulatory hemodynamics and thus the disease course. They also present a treatment dilemma due to the cirrhosis-related risk of variceal hemorrhage. No national study to date has examined the long-term outcome of this patient population.
Methods: All patients admitted with liver cirrhosis in the United States in January were identified from 2016 to 2022 through the National Readmission Database. Patients with a principal diagnosis of either DVT/PE or PVT were identified. The follow-up period was 12 months. The primary outcome was liver decompensation. The secondary outcomes were 1-year mortality, incidence of esophageal or gastric varices, variceal hemorrhage, ascites, hepatic encephalopathy, acute liver failure and liver transplantation. Diagnoses were identified using ICD-10 CM codes. Logistic regression models were used to adjust for confounders, which were age, sex, income in the patient’s zipcode, insurance type, Charlson score and hospital bedsize, teaching status and urban location.
Results: 365,848 patients were included in the study. Of those, 1,767 patients had a DVT/PE and 695 had PVT. Table 1 presents the patient’s characteristics. The mean age was 61 years. The majority of patients were males, of lower income, insured by Medicare or Medicaid, and treated at large urban non-teaching hospitals. The adjusted odds ratios are presented in Table 2. Compared with patients without thromboembolism, patients with DVT/PE had lower adjusted odds of all-cause mortality, new ascites development and incident liver decompensation. On the other hand, PVT was associated with almost 3-fold increase in the adjusted odds of both new gastric or esophageal varices and variceal hemorrhage as well as 50% increase in the adjusted odds of acute liver failure. The three patient groups had similar adjusted odds of liver transplantation and incident hepatic encephalopathy.
Discussion: The development of DVT/PE is not associated with worsening outcomes among patients with liver cirrhosis and seems to be protective against liver decompensation and 1-year mortality. On the other hand, portal vein thrombosis is associated with a substantial increase in the risk of varices, variceal hemorrhage and acute liver failure. These finding can help guide follow-up frequency and prognosis discussion in this setting.
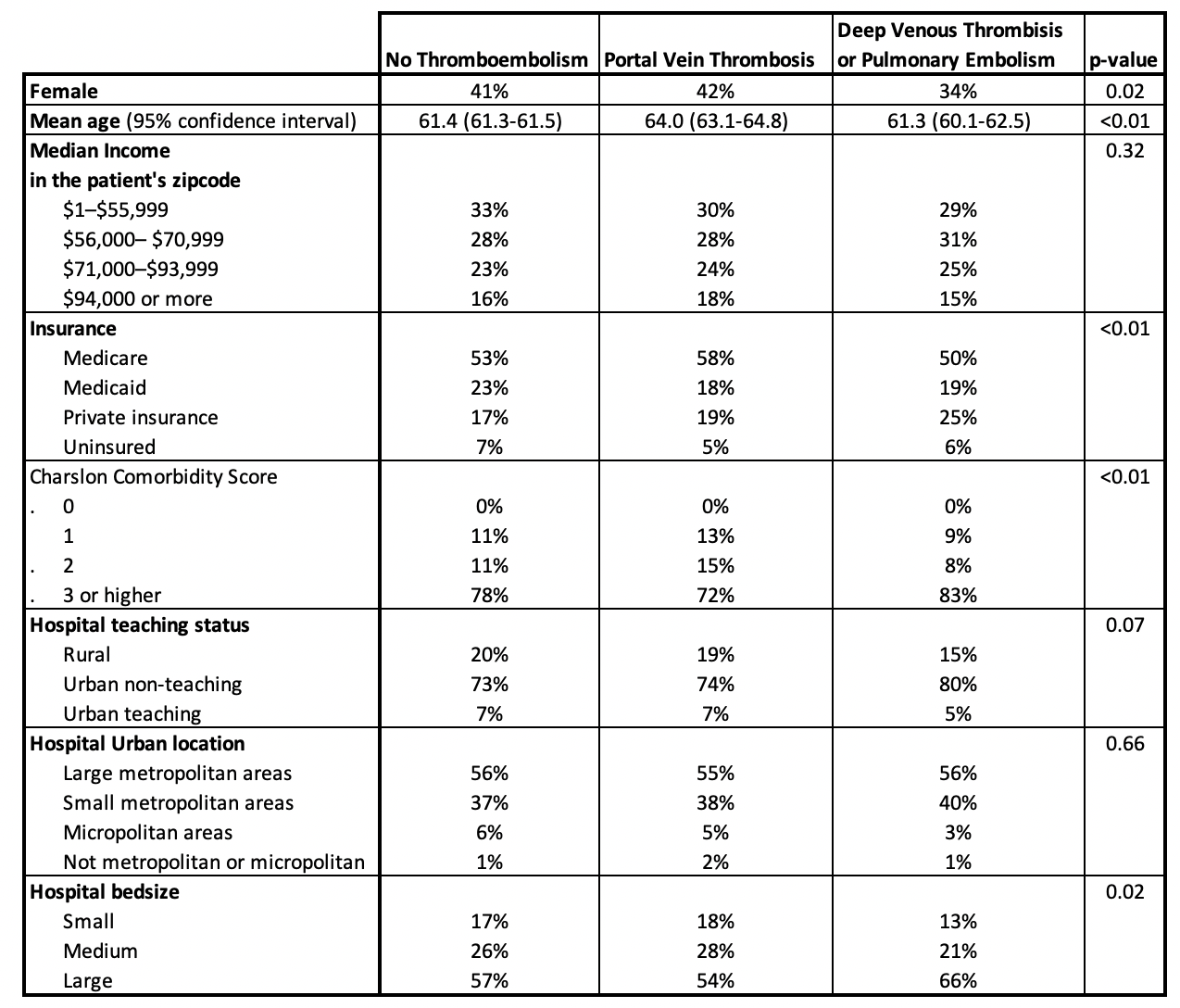
Figure: Table 1: Patient's Characteristics
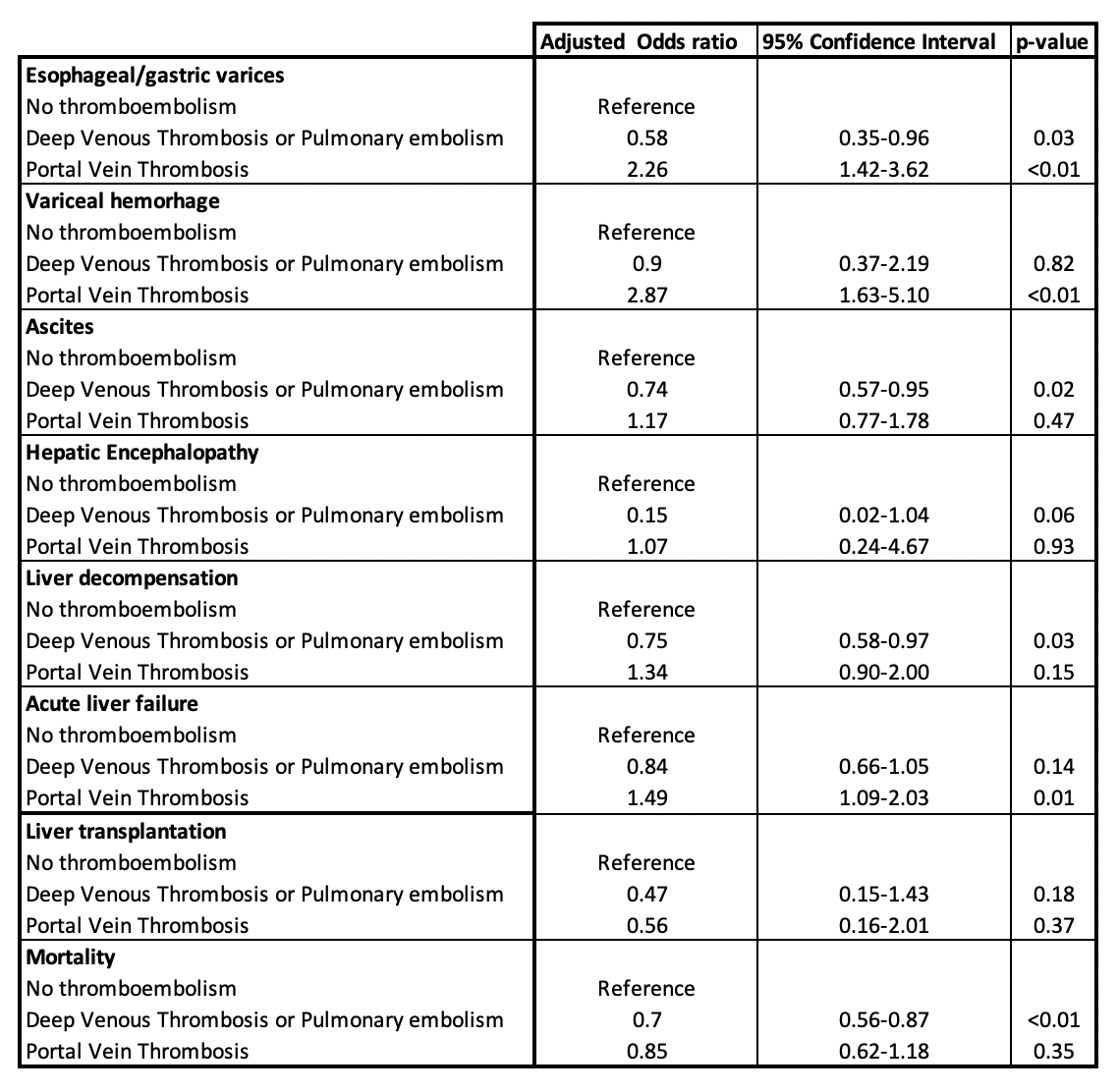
Figure: Table 2: Study Outcomes
Disclosures:
Martin Banks indicated no relevant financial relationships.
Adaobi Ahanotu indicated no relevant financial relationships.
Rand Alkalbani indicated no relevant financial relationships.
Farhan Azad indicated no relevant financial relationships.
Kelly Vo indicated no relevant financial relationships.
Amolika Gupta indicated no relevant financial relationships.
Marwan Abougergi indicated no relevant financial relationships.
Martin Banks, MD1, Adaobi Ahanotu, MD2, Rand Alkalbani, MD3, Farhan Azad, DO3, Kelly M. Vo, DO4, Amolika Gupta, MD5, Marwan S. Abougergi, MD6. P1654 - Effect of Thromboembolic Events on Long-Term Treatment Outcomes in Liver Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
