Sunday Poster Session
Category: Liver
P1652 - Comparative Analysis of Renal Histopathological Findings in Liver Transplantation Alone vs Simultaneous Liver-Kidney Transplantation
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Mohammed Abourahma, MD
Loyola University Medical Center
Willowbrook, IL
Presenting Author(s)
Mohammed Abourahma, MD1, Dinkar Ahuja, MD2, Alexander O'Hara, MD3, Puja Brahmbhatt, MD3, Michelle Lee, MD3, Atta Ullah, MD2, Scott Cotler, MD3, Kavitha Vellanki, MD3
1Loyola University Medical Center, Willowbrook, IL; 2Loyola University Medical Center, Chicago, IL; 3Loyola University Medical Center, Maywood, IL
Introduction: Chronic kidney disease (CKD) is common in solid organ transplant recipients (SOT). Due to immune tolerance, liver transplant recipients often require less immunosuppression than other SOT. Renal histopathology may differ between LTA and simultaneous liver-kidney transplant (SLKT) recipients due to distinct clinical profiles, but no direct comparison has been reported.
Methods: We performed a single-center retrospective review of adults who underwent liver transplantation (2000–2023) and received a post-transplant kidney biopsy. Clinical history and biopsy data were reviewed. Groups were compared using Fisher's exact test.
Results:
A total of 42 kidney biopsies were reviewed from 36 patients (15 in 14 LTA recipients, 27 in 22 SLKT recipients). SLKT patients were younger, with hepatorenal syndrome (HRS) as the most common cause of renal failure, and biopsies were done earlier post-transplant (median 9 vs. 23 months). Seven LTA recipients developed ESRD (4 on dialysis, 3 received a kidney transplant).
In LTA, primary glomerular disease was predominant: FSGS (26.6%), diabetic nephropathy (20%), AKI (13.3%), glomerulosclerosis (13.3%), TMA (6.6%), TMA/MPGN (6.6%), and IgA nephropathy (6.6%). One case had rare hepatic glomerulopathy with lipid deposits and mild IgA nephropathy.
In SLKT, AKI (29.6%) was most common, followed by rejection (22.2%), non-specific inflammation (22.2%), BK nephropathy (18.5%), FSGS, IgA nephropathy, and glomerulosclerosis (each 4.5%). One had overlapping BK nephropathy and rejection; three had concurrent liver and kidney rejection within 4 months.
Overall, primary glomerular pathology was higher in LTA recipients than SLKT recipients (73.3% vs. 3.7%, p < 0.01). Chronic changes were more frequent in LTA (≥30% sclerosis in 66.6% vs. 9% in SLKT, p < 0.01).
Discussion: Primary glomerular diseases are common in LTA recipients. Kidney biopsy should be considered when clinically appropriate to support listing for SLKT. SLKT recipients more often showed acute pathologies such as AKI, rejection, and BK nephropathy.
Since primary glomerular pathologies were more common in LTA, this suggests that kidney dysfunction in this group is often more related to intrinsic renal disease that may have been present before transplantation. Also, chronic changes were more common in LTA. This suggests the need for more stringent work-up and may necessitate a need for biopsy protocols to better assess selection of patients for SLKT and ultimately improve outcomes.
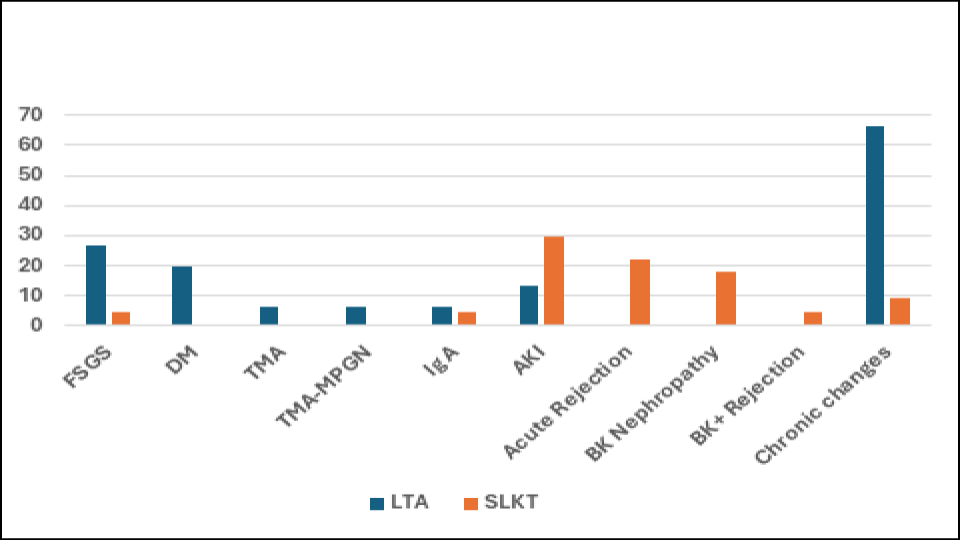
Figure: Table 1 - Clinical Characteristics of Patients Undergoing Renal Biopsy after LTA and SLKT
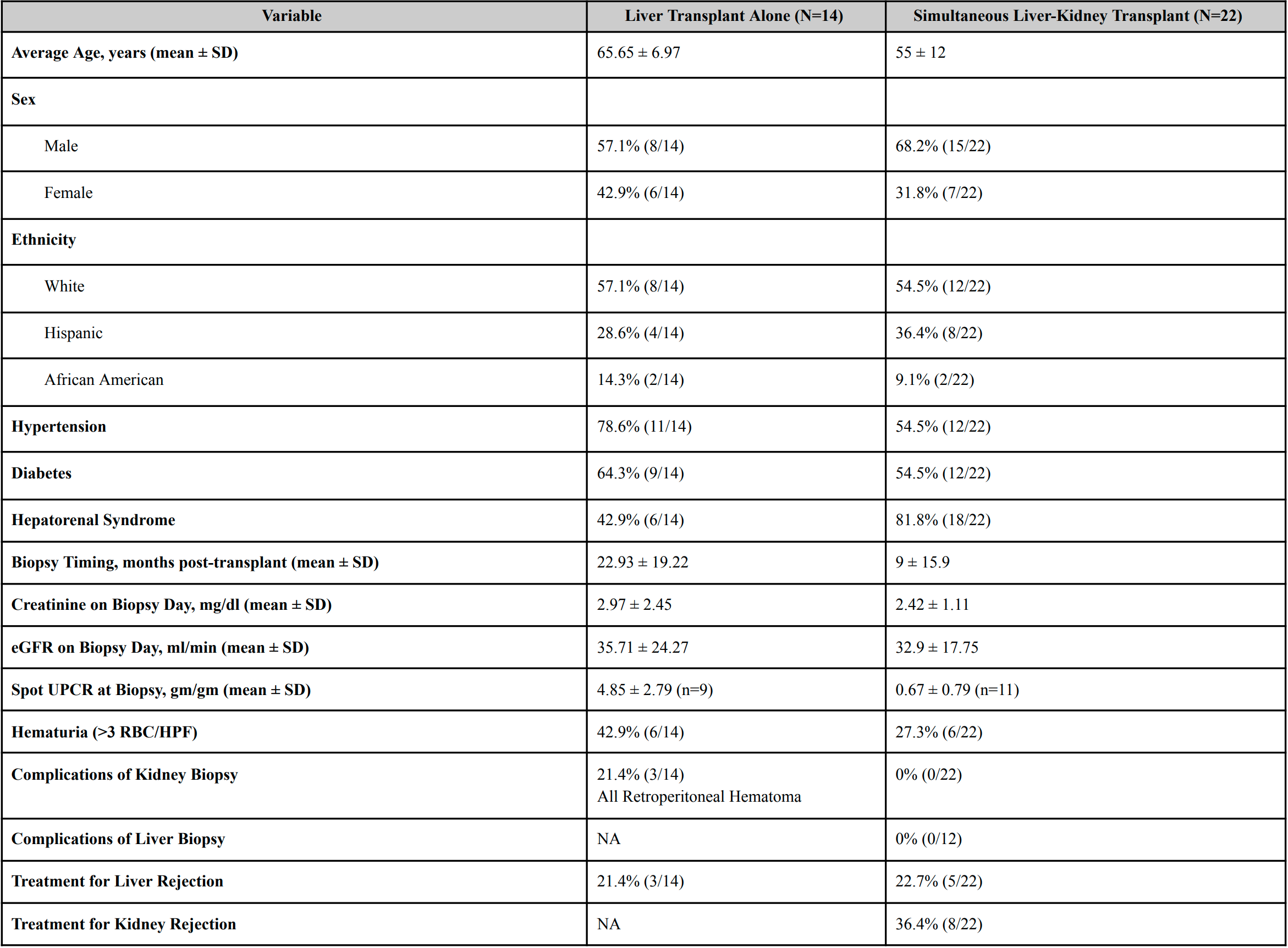
Figure: Kidney Histopathology in Liver Transplantation
Disclosures:
Mohammed Abourahma indicated no relevant financial relationships.
Dinkar Ahuja indicated no relevant financial relationships.
Alexander O'Hara indicated no relevant financial relationships.
Puja Brahmbhatt indicated no relevant financial relationships.
Michelle Lee indicated no relevant financial relationships.
Atta Ullah indicated no relevant financial relationships.
Scott Cotler indicated no relevant financial relationships.
Kavitha Vellanki indicated no relevant financial relationships.
Mohammed Abourahma, MD1, Dinkar Ahuja, MD2, Alexander O'Hara, MD3, Puja Brahmbhatt, MD3, Michelle Lee, MD3, Atta Ullah, MD2, Scott Cotler, MD3, Kavitha Vellanki, MD3. P1652 - Comparative Analysis of Renal Histopathological Findings in Liver Transplantation Alone vs Simultaneous Liver-Kidney Transplantation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Loyola University Medical Center, Willowbrook, IL; 2Loyola University Medical Center, Chicago, IL; 3Loyola University Medical Center, Maywood, IL
Introduction: Chronic kidney disease (CKD) is common in solid organ transplant recipients (SOT). Due to immune tolerance, liver transplant recipients often require less immunosuppression than other SOT. Renal histopathology may differ between LTA and simultaneous liver-kidney transplant (SLKT) recipients due to distinct clinical profiles, but no direct comparison has been reported.
Methods: We performed a single-center retrospective review of adults who underwent liver transplantation (2000–2023) and received a post-transplant kidney biopsy. Clinical history and biopsy data were reviewed. Groups were compared using Fisher's exact test.
Results:
A total of 42 kidney biopsies were reviewed from 36 patients (15 in 14 LTA recipients, 27 in 22 SLKT recipients). SLKT patients were younger, with hepatorenal syndrome (HRS) as the most common cause of renal failure, and biopsies were done earlier post-transplant (median 9 vs. 23 months). Seven LTA recipients developed ESRD (4 on dialysis, 3 received a kidney transplant).
In LTA, primary glomerular disease was predominant: FSGS (26.6%), diabetic nephropathy (20%), AKI (13.3%), glomerulosclerosis (13.3%), TMA (6.6%), TMA/MPGN (6.6%), and IgA nephropathy (6.6%). One case had rare hepatic glomerulopathy with lipid deposits and mild IgA nephropathy.
In SLKT, AKI (29.6%) was most common, followed by rejection (22.2%), non-specific inflammation (22.2%), BK nephropathy (18.5%), FSGS, IgA nephropathy, and glomerulosclerosis (each 4.5%). One had overlapping BK nephropathy and rejection; three had concurrent liver and kidney rejection within 4 months.
Overall, primary glomerular pathology was higher in LTA recipients than SLKT recipients (73.3% vs. 3.7%, p < 0.01). Chronic changes were more frequent in LTA (≥30% sclerosis in 66.6% vs. 9% in SLKT, p < 0.01).
Discussion: Primary glomerular diseases are common in LTA recipients. Kidney biopsy should be considered when clinically appropriate to support listing for SLKT. SLKT recipients more often showed acute pathologies such as AKI, rejection, and BK nephropathy.
Since primary glomerular pathologies were more common in LTA, this suggests that kidney dysfunction in this group is often more related to intrinsic renal disease that may have been present before transplantation. Also, chronic changes were more common in LTA. This suggests the need for more stringent work-up and may necessitate a need for biopsy protocols to better assess selection of patients for SLKT and ultimately improve outcomes.
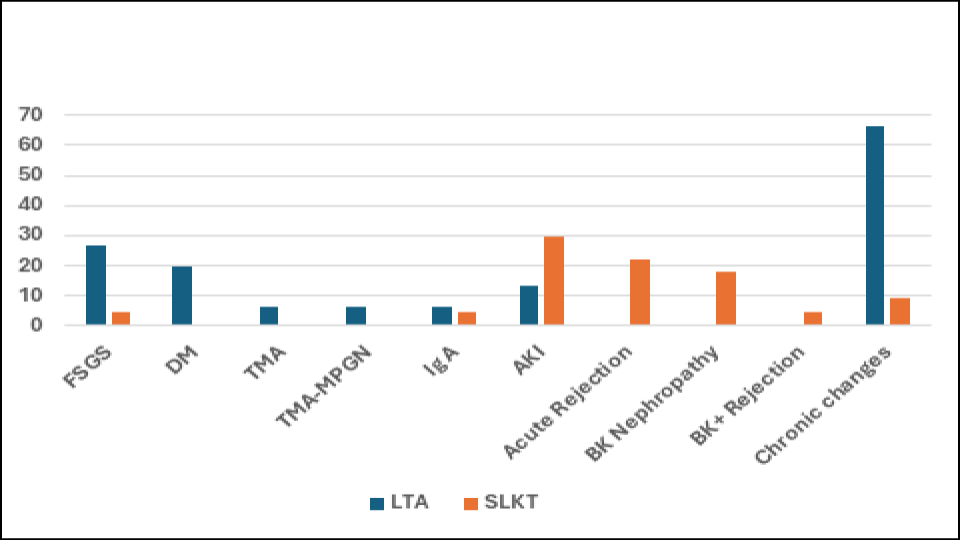
Figure: Table 1 - Clinical Characteristics of Patients Undergoing Renal Biopsy after LTA and SLKT
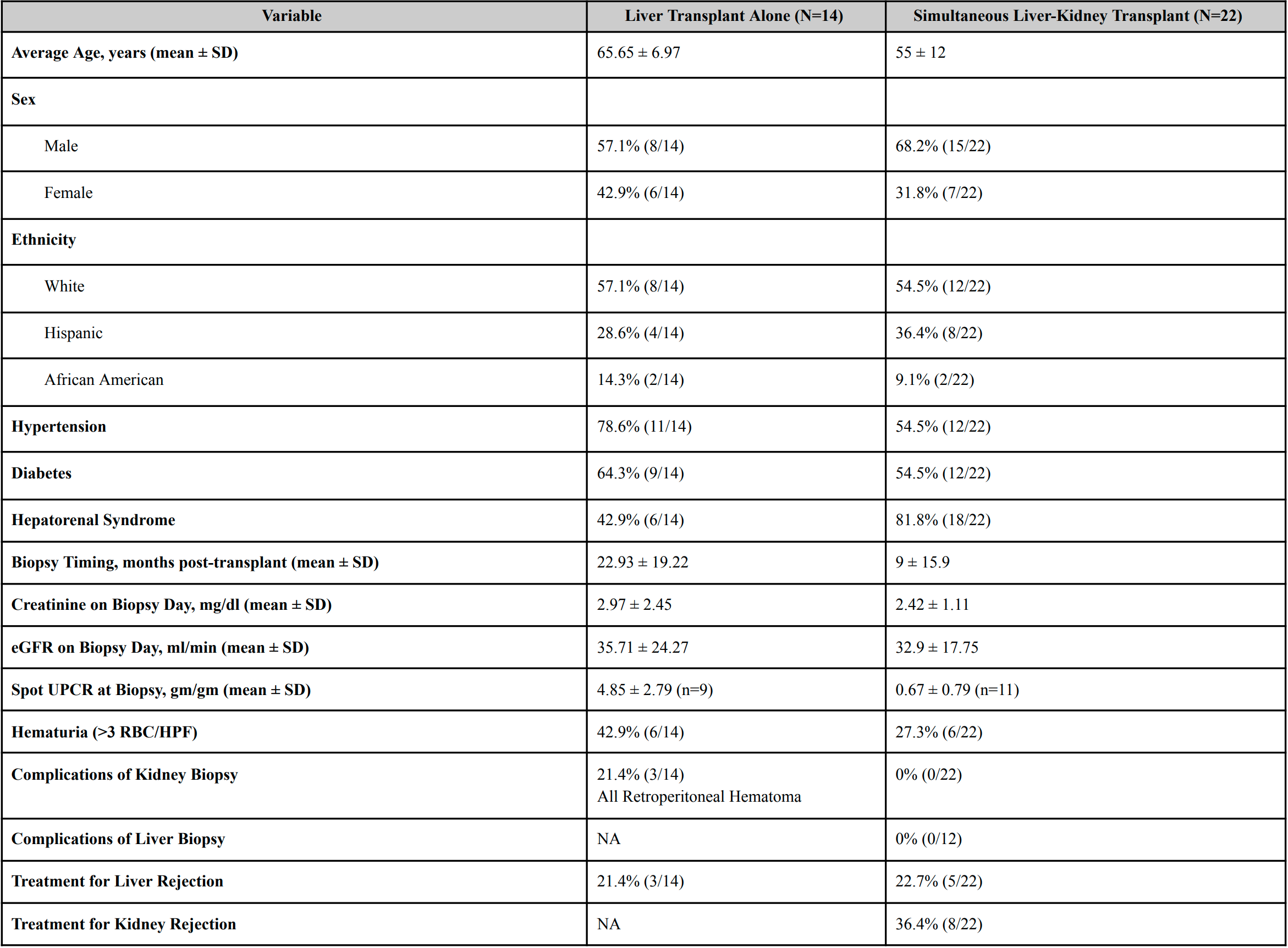
Figure: Kidney Histopathology in Liver Transplantation
Disclosures:
Mohammed Abourahma indicated no relevant financial relationships.
Dinkar Ahuja indicated no relevant financial relationships.
Alexander O'Hara indicated no relevant financial relationships.
Puja Brahmbhatt indicated no relevant financial relationships.
Michelle Lee indicated no relevant financial relationships.
Atta Ullah indicated no relevant financial relationships.
Scott Cotler indicated no relevant financial relationships.
Kavitha Vellanki indicated no relevant financial relationships.
Mohammed Abourahma, MD1, Dinkar Ahuja, MD2, Alexander O'Hara, MD3, Puja Brahmbhatt, MD3, Michelle Lee, MD3, Atta Ullah, MD2, Scott Cotler, MD3, Kavitha Vellanki, MD3. P1652 - Comparative Analysis of Renal Histopathological Findings in Liver Transplantation Alone vs Simultaneous Liver-Kidney Transplantation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
