Sunday Poster Session
Category: Liver
P1647 - Prevalence of Metabolic Dysfunction Associated Steatotic Liver Disease in Patients With Type 2 Diabetes Mellitus in the United Arab Emirates
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- SK
Shiva Kumar, MD, FACG
Cleveland Clinic Abu Dhabi
Abu Dhabi, Abu Dhabi, United Arab Emirates
Presenting Author(s)
Oumaima AlKabbani, MD1, Fatma Mahmoud, MD2, Doa’a Alkhader, MD2, Wael Osman, PhD1, Shaikha Alharmoodi, MD1, Abdulrahman Alakberi, MD1, Rabih Hijazi, MD2, Maguy Chiha, MD2, Ola Jarad, MD2, Shiva Kumar, MD, FACG2
1Khalifa University, Abu Dhabi, Abu Dhabi, United Arab Emirates; 2Cleveland Clinic Abu Dhabi, Abu Dhabi, Abu Dhabi, United Arab Emirates
Introduction: Metabolic dysfunction associated steatotic liver disease (MASLD) has emerged as the primary indication for liver transplantation and primary risk factor for the development of Hepatocellular carcinoma (HCC). The prevalence of Type 2 Diabetes Mellitus (T2DM) and MASLD in the Middle East are among the highest in the world. T2DM is an important determinant of the presence of MASLD and its presence has also been shown to be a predictor of advanced fibrosis, mortality and risk of HCC in MASLD. However, majority of patients with T2DM are not screened for MASLD and there is limited data on the prevalence of MASLD and its phenotype among patients with T2DM in the UAE, underscoring the need for regional data to help guide clinical decision making. Our aim was to determine the prevalence of MASLD and advanced fibrosis using Laboratory-based non-invasive tests and Transient Elastography in a cohort of Emirati patients with Type 2 Diabetes Mellitus
Methods: We evaluated a retrospective cohort of 735 consecutive Emirati patients ≥ 18 years of age with T2DM and no prior diagnosis of MASLD from Jan 2022 - April 2024. 492 met study inclusion criteria (figure 1). FIB-4 score > 1.3 and ≥ 2.67 and MASLD fibrosis score (MFS score) > −1.455 and ≥ 0.675 were used to identify subjects at risk of any fibrosis and advanced fibrosis, respectively. Study groups were compared using Chi square test and one-way ANOVA, and multivariable regression was performed to identify factors associated with MASLD and advanced fibrosis.
Results: Details of the study subjects including distribution of body mass index, FIB-4 and MFS scores is shown in Figure 1. Among the subset of subjects who underwent Transient Elastography (FibroScan), 18.9 % were noted to have some degree of underlying fibrosis, with 9% having moderate-advanced fibrosis. Based on the controlled attenuation parameter (CAP) score, 88% were found to have steatosis with severe steatosis in 55%. Variables associated with FIB-4 score and correlation between FIB-4 and Liver Stiffness Measurement (LSM) using scatter plot are shown in Figure 2.
Discussion: In a cohort of Emirati patients with T2DM, 43% were noted to have MASLD with fibrosis using non-invasive tests and 19% had fibrosis on TE with moderate to advanced fibrosis in 9%. Age, BMI and hypertension were among the variables associated with presence of underlying fibrosis. These results underscore the need to screen patients with T2DM in the Middle East for MASLD and fibrosis to enable timely intervention.
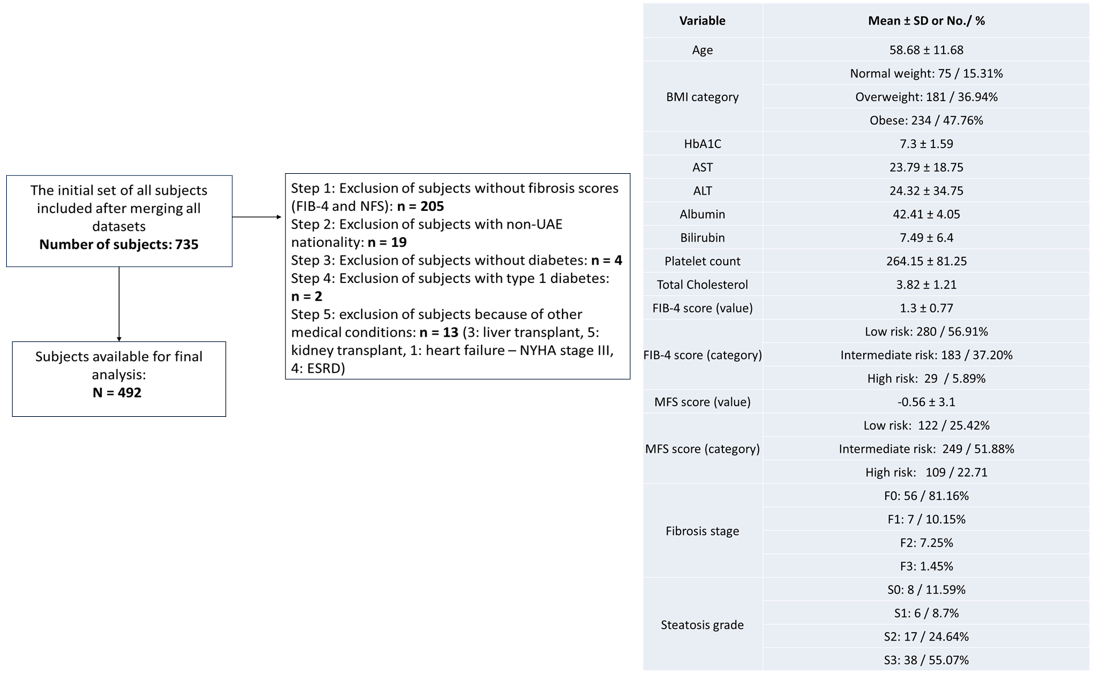
Figure: Figure 1. Study subjects and their characteristics
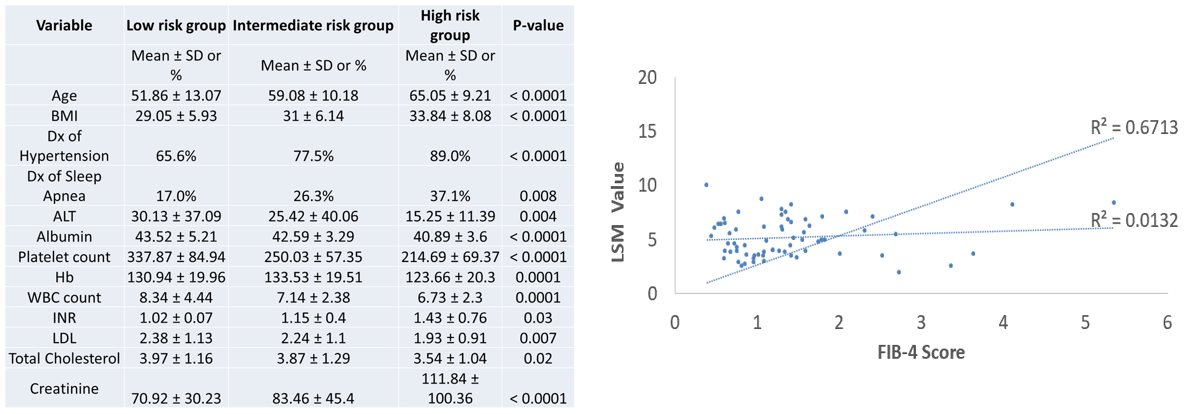
Figure: Figure 2. Variables associated with FIB-4 score and correlation between FIB-4 and LSM using scatter plot
Disclosures:
Oumaima AlKabbani indicated no relevant financial relationships.
Fatma Mahmoud indicated no relevant financial relationships.
Doa’a Alkhader indicated no relevant financial relationships.
Wael Osman indicated no relevant financial relationships.
Shaikha Alharmoodi indicated no relevant financial relationships.
Abdulrahman Alakberi indicated no relevant financial relationships.
Rabih Hijazi indicated no relevant financial relationships.
Maguy Chiha indicated no relevant financial relationships.
Ola Jarad indicated no relevant financial relationships.
Shiva Kumar indicated no relevant financial relationships.
Oumaima AlKabbani, MD1, Fatma Mahmoud, MD2, Doa’a Alkhader, MD2, Wael Osman, PhD1, Shaikha Alharmoodi, MD1, Abdulrahman Alakberi, MD1, Rabih Hijazi, MD2, Maguy Chiha, MD2, Ola Jarad, MD2, Shiva Kumar, MD, FACG2. P1647 - Prevalence of Metabolic Dysfunction Associated Steatotic Liver Disease in Patients With Type 2 Diabetes Mellitus in the United Arab Emirates, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Khalifa University, Abu Dhabi, Abu Dhabi, United Arab Emirates; 2Cleveland Clinic Abu Dhabi, Abu Dhabi, Abu Dhabi, United Arab Emirates
Introduction: Metabolic dysfunction associated steatotic liver disease (MASLD) has emerged as the primary indication for liver transplantation and primary risk factor for the development of Hepatocellular carcinoma (HCC). The prevalence of Type 2 Diabetes Mellitus (T2DM) and MASLD in the Middle East are among the highest in the world. T2DM is an important determinant of the presence of MASLD and its presence has also been shown to be a predictor of advanced fibrosis, mortality and risk of HCC in MASLD. However, majority of patients with T2DM are not screened for MASLD and there is limited data on the prevalence of MASLD and its phenotype among patients with T2DM in the UAE, underscoring the need for regional data to help guide clinical decision making. Our aim was to determine the prevalence of MASLD and advanced fibrosis using Laboratory-based non-invasive tests and Transient Elastography in a cohort of Emirati patients with Type 2 Diabetes Mellitus
Methods: We evaluated a retrospective cohort of 735 consecutive Emirati patients ≥ 18 years of age with T2DM and no prior diagnosis of MASLD from Jan 2022 - April 2024. 492 met study inclusion criteria (figure 1). FIB-4 score > 1.3 and ≥ 2.67 and MASLD fibrosis score (MFS score) > −1.455 and ≥ 0.675 were used to identify subjects at risk of any fibrosis and advanced fibrosis, respectively. Study groups were compared using Chi square test and one-way ANOVA, and multivariable regression was performed to identify factors associated with MASLD and advanced fibrosis.
Results: Details of the study subjects including distribution of body mass index, FIB-4 and MFS scores is shown in Figure 1. Among the subset of subjects who underwent Transient Elastography (FibroScan), 18.9 % were noted to have some degree of underlying fibrosis, with 9% having moderate-advanced fibrosis. Based on the controlled attenuation parameter (CAP) score, 88% were found to have steatosis with severe steatosis in 55%. Variables associated with FIB-4 score and correlation between FIB-4 and Liver Stiffness Measurement (LSM) using scatter plot are shown in Figure 2.
Discussion: In a cohort of Emirati patients with T2DM, 43% were noted to have MASLD with fibrosis using non-invasive tests and 19% had fibrosis on TE with moderate to advanced fibrosis in 9%. Age, BMI and hypertension were among the variables associated with presence of underlying fibrosis. These results underscore the need to screen patients with T2DM in the Middle East for MASLD and fibrosis to enable timely intervention.
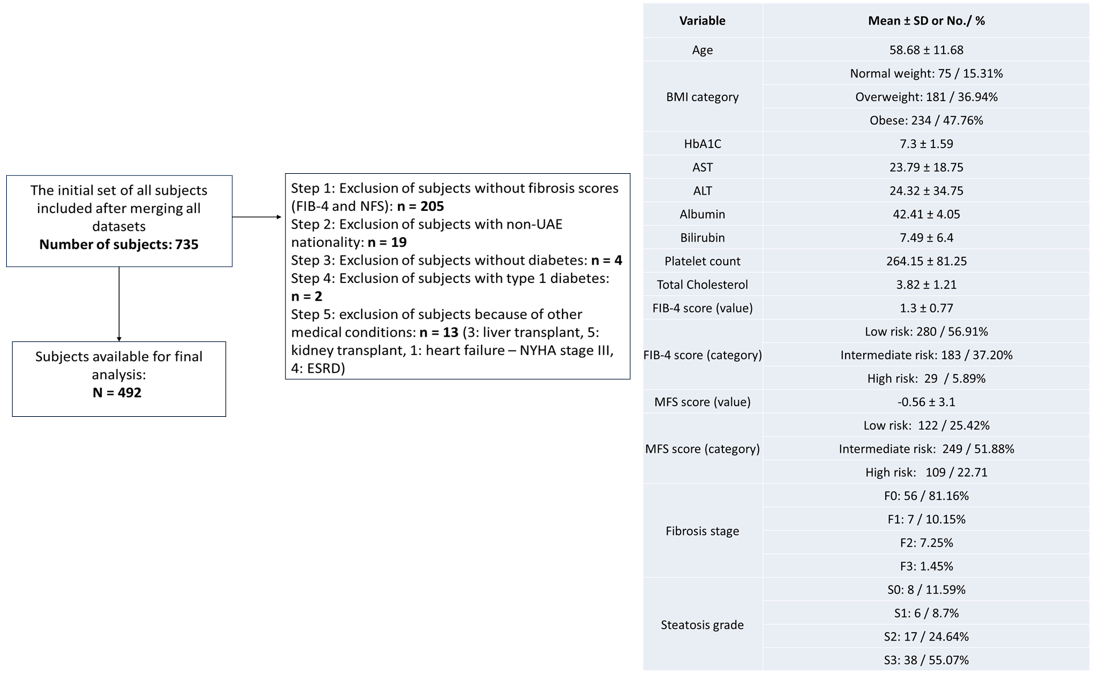
Figure: Figure 1. Study subjects and their characteristics
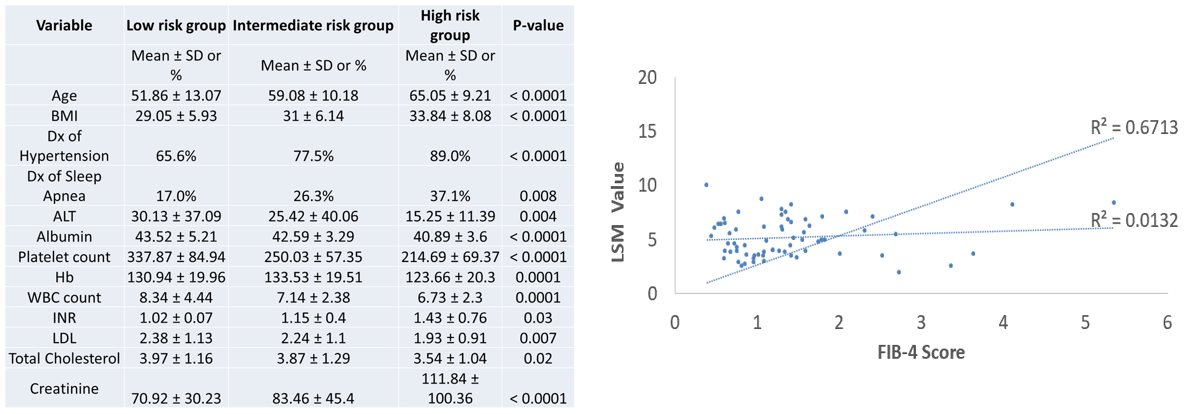
Figure: Figure 2. Variables associated with FIB-4 score and correlation between FIB-4 and LSM using scatter plot
Disclosures:
Oumaima AlKabbani indicated no relevant financial relationships.
Fatma Mahmoud indicated no relevant financial relationships.
Doa’a Alkhader indicated no relevant financial relationships.
Wael Osman indicated no relevant financial relationships.
Shaikha Alharmoodi indicated no relevant financial relationships.
Abdulrahman Alakberi indicated no relevant financial relationships.
Rabih Hijazi indicated no relevant financial relationships.
Maguy Chiha indicated no relevant financial relationships.
Ola Jarad indicated no relevant financial relationships.
Shiva Kumar indicated no relevant financial relationships.
Oumaima AlKabbani, MD1, Fatma Mahmoud, MD2, Doa’a Alkhader, MD2, Wael Osman, PhD1, Shaikha Alharmoodi, MD1, Abdulrahman Alakberi, MD1, Rabih Hijazi, MD2, Maguy Chiha, MD2, Ola Jarad, MD2, Shiva Kumar, MD, FACG2. P1647 - Prevalence of Metabolic Dysfunction Associated Steatotic Liver Disease in Patients With Type 2 Diabetes Mellitus in the United Arab Emirates, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
