Sunday Poster Session
Category: Liver
P1641 - Aspirin Use Is Associated With Reduced Mortality and Critical Complications in Cirrhosis: A Nationwide Inpatient Analysis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Muhamad Oum, MD (he/him/his)
Saint Agnes Medical Center, Fresno CA
Fresno, CA
Presenting Author(s)
Muhamad Oum, MD1, Khalid Aloum, MD2, Bisher Sawaf, MD3, Sammy Saab, MD, MPH4
1Saint Agnes Medical Center, Fresno CA, Fresno, CA; 2SBH Health System, Bronx, NY; 3The University of Toledo, Toledo, OH; 4David Geffen School of Medicine at UCLA, Los Angeles, CA
Introduction: Cirrhosis is a progressive, high-mortality condition marked by inflammation, portal hypertension, and systemic complications. Although advances in supportive care have improved survival, pharmacologic interventions to alter outcomes remain limited. Aspirin, through its anti-inflammatory and antiplatelet effects, may mitigate liver-related complications. This study evaluated the association between long-term aspirin use and clinical outcomes in hospitalized patients with cirrhosis using a nationally representative database.
Methods: We conducted a retrospective cohort study using the Nationwide Inpatient Sample (NIS) from 2016 to 2021. Patients with cirrhosis were identified using ICD-10 codes and stratified by long-term aspirin use. Collected variables included demographics, comorbidities (Charlson index), insurance type, and hospital characteristics. Primary outcomes included in-hospital mortality, ICU admission, shock, sepsis, peritonitis, acute kidney injury (AKI), and length of stay (LOS). Multivariable logistic regression models adjusted for age, sex, race, insurance, income, and comorbidity burden were used to estimate adjusted odds ratios (aORs) and 95% confidence intervals (CIs).
Results: Among 2,720,259 cirrhosis hospitalizations, 308,945 (11.4%) involved long-term aspirin use. Aspirin users were older (67.2 vs. 63.3 years), more often male (57.9% vs. 52.7%), and had greater comorbidity burden. Aspirin use was independently associated with lower odds of:
· In-hospital mortality (aOR 0.50; 95% CI: 0.47–0.53; p < 0.001),
· ICU admission (aOR 0.66; 95% CI: 0.62–0.70; p < 0.001),
· Shock (aOR 0.58; 95% CI: 0.55–0.61; p < 0.001),
· Sepsis (aOR 0.65; 95% CI: 0.63–0.68; p < 0.001),
· Peritonitis (aOR 0.54; 95% CI: 0.50–0.58; p < 0.001),
· AKI (aOR 0.82; 95% CI: 0.80–0.84; p < 0.001).
Aspirin users had a significantly shorter mean hospital stay (5.37 vs. 6.20 days; p < 0.001), with a mean reduction of 0.83 days (95% CI: −0.90 to −0.77; p < 0.001).
Discussion: In this large national cohort, long-term aspirin use was associated with reduced mortality and critical complications in patients with cirrhosis. Despite a higher baseline comorbidity burden, aspirin users experienced improved outcomes and shorter hospital stays. These findings highlight a potential protective role of aspirin in cirrhosis and support the need for prospective studies to evaluate its therapeutic safety and efficacy.
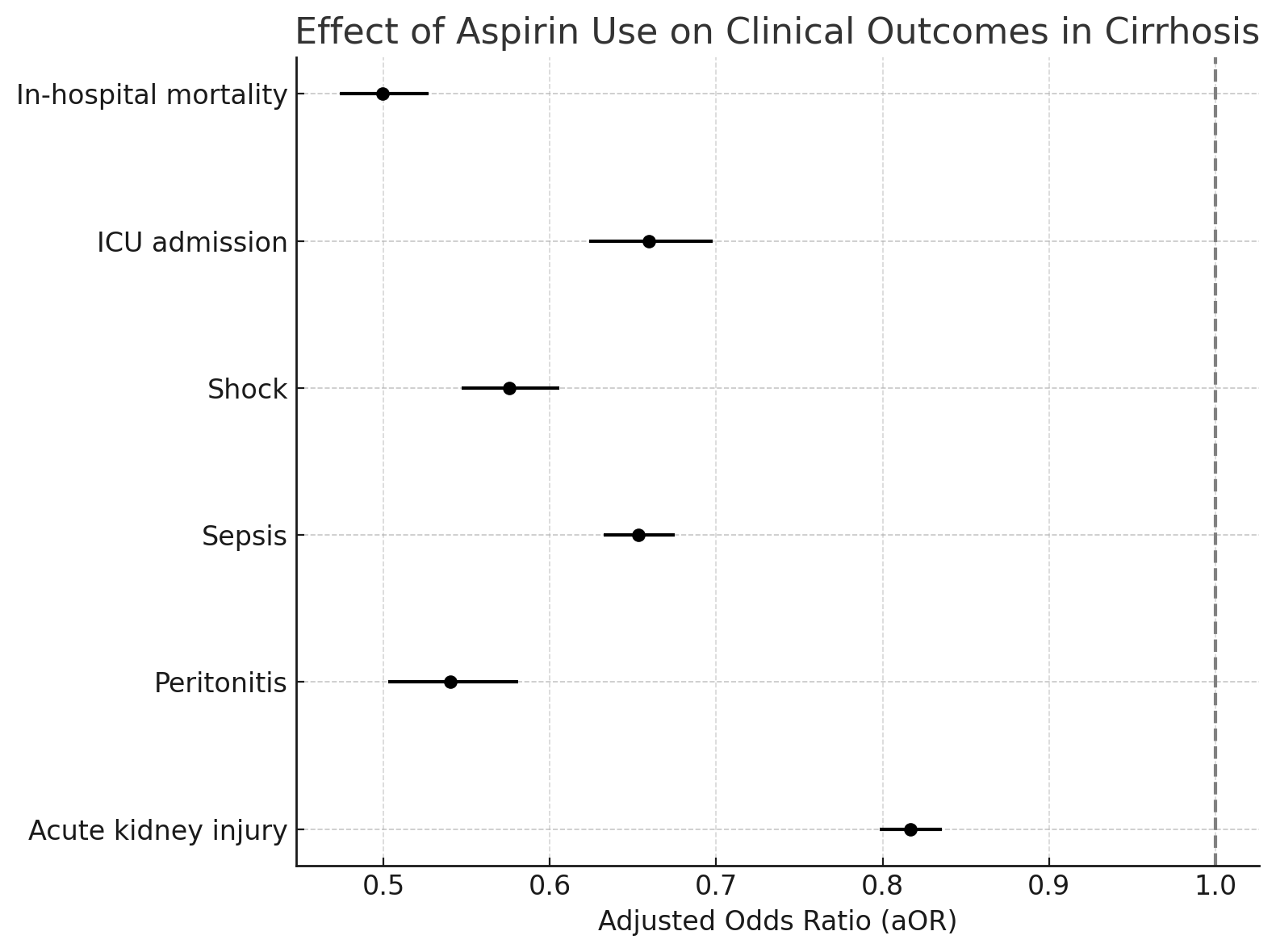
Figure: Effect of Aspirin use on Clinical Outcomes in Cirrhosis
Disclosures:
Muhamad Oum indicated no relevant financial relationships.
Khalid Aloum indicated no relevant financial relationships.
Bisher Sawaf indicated no relevant financial relationships.
Sammy Saab: abbvie – Speakers Bureau. eton – Advisor or Review Panel Member. gilead – Advisor or Review Panel Member, Advisory Committee/Board Member, Consultant, Speakers Bureau. ipsen – Advisor or Review Panel Member, Advisory Committee/Board Member, Speakers Bureau. kezar – Advisory Committee/Board Member. madrigal – Advisor or Review Panel Member, Advisory Committee/Board Member, Speakers Bureau. orphalan – Advisory Committee/Board Member. salix – Advisory Committee/Board Member, Speakers Bureau.
Muhamad Oum, MD1, Khalid Aloum, MD2, Bisher Sawaf, MD3, Sammy Saab, MD, MPH4. P1641 - Aspirin Use Is Associated With Reduced Mortality and Critical Complications in Cirrhosis: A Nationwide Inpatient Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Saint Agnes Medical Center, Fresno CA, Fresno, CA; 2SBH Health System, Bronx, NY; 3The University of Toledo, Toledo, OH; 4David Geffen School of Medicine at UCLA, Los Angeles, CA
Introduction: Cirrhosis is a progressive, high-mortality condition marked by inflammation, portal hypertension, and systemic complications. Although advances in supportive care have improved survival, pharmacologic interventions to alter outcomes remain limited. Aspirin, through its anti-inflammatory and antiplatelet effects, may mitigate liver-related complications. This study evaluated the association between long-term aspirin use and clinical outcomes in hospitalized patients with cirrhosis using a nationally representative database.
Methods: We conducted a retrospective cohort study using the Nationwide Inpatient Sample (NIS) from 2016 to 2021. Patients with cirrhosis were identified using ICD-10 codes and stratified by long-term aspirin use. Collected variables included demographics, comorbidities (Charlson index), insurance type, and hospital characteristics. Primary outcomes included in-hospital mortality, ICU admission, shock, sepsis, peritonitis, acute kidney injury (AKI), and length of stay (LOS). Multivariable logistic regression models adjusted for age, sex, race, insurance, income, and comorbidity burden were used to estimate adjusted odds ratios (aORs) and 95% confidence intervals (CIs).
Results: Among 2,720,259 cirrhosis hospitalizations, 308,945 (11.4%) involved long-term aspirin use. Aspirin users were older (67.2 vs. 63.3 years), more often male (57.9% vs. 52.7%), and had greater comorbidity burden. Aspirin use was independently associated with lower odds of:
· In-hospital mortality (aOR 0.50; 95% CI: 0.47–0.53; p < 0.001),
· ICU admission (aOR 0.66; 95% CI: 0.62–0.70; p < 0.001),
· Shock (aOR 0.58; 95% CI: 0.55–0.61; p < 0.001),
· Sepsis (aOR 0.65; 95% CI: 0.63–0.68; p < 0.001),
· Peritonitis (aOR 0.54; 95% CI: 0.50–0.58; p < 0.001),
· AKI (aOR 0.82; 95% CI: 0.80–0.84; p < 0.001).
Aspirin users had a significantly shorter mean hospital stay (5.37 vs. 6.20 days; p < 0.001), with a mean reduction of 0.83 days (95% CI: −0.90 to −0.77; p < 0.001).
Discussion: In this large national cohort, long-term aspirin use was associated with reduced mortality and critical complications in patients with cirrhosis. Despite a higher baseline comorbidity burden, aspirin users experienced improved outcomes and shorter hospital stays. These findings highlight a potential protective role of aspirin in cirrhosis and support the need for prospective studies to evaluate its therapeutic safety and efficacy.
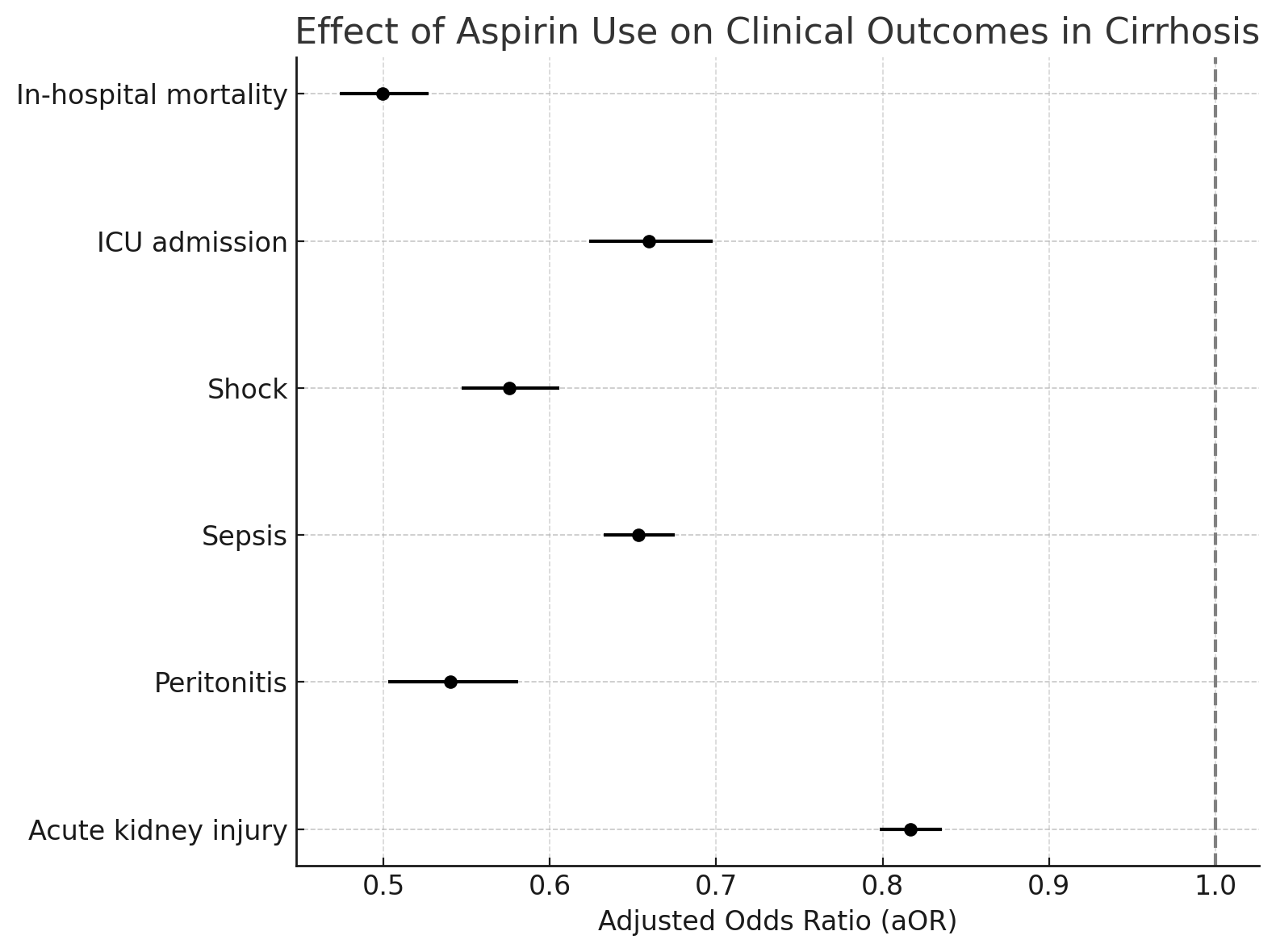
Figure: Effect of Aspirin use on Clinical Outcomes in Cirrhosis
Disclosures:
Muhamad Oum indicated no relevant financial relationships.
Khalid Aloum indicated no relevant financial relationships.
Bisher Sawaf indicated no relevant financial relationships.
Sammy Saab: abbvie – Speakers Bureau. eton – Advisor or Review Panel Member. gilead – Advisor or Review Panel Member, Advisory Committee/Board Member, Consultant, Speakers Bureau. ipsen – Advisor or Review Panel Member, Advisory Committee/Board Member, Speakers Bureau. kezar – Advisory Committee/Board Member. madrigal – Advisor or Review Panel Member, Advisory Committee/Board Member, Speakers Bureau. orphalan – Advisory Committee/Board Member. salix – Advisory Committee/Board Member, Speakers Bureau.
Muhamad Oum, MD1, Khalid Aloum, MD2, Bisher Sawaf, MD3, Sammy Saab, MD, MPH4. P1641 - Aspirin Use Is Associated With Reduced Mortality and Critical Complications in Cirrhosis: A Nationwide Inpatient Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
