Sunday Poster Session
Category: Liver
P1716 - Beware the “Benign” Hepatic Cyst: Mass Effect Causing Portal Vein Thrombosis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Claire F. Maher, BA
University of Virginia School of Medicine
Charlottesville, VA
Presenting Author(s)
Claire F. Maher, BA1, Ana S. Lopez Alvarez, BS, MS1, Emily Minor, MD, PhD2, Samantha Epstein, MD3, Brian J. Wentworth, MD, MS2
1University of Virginia School of Medicine, Charlottesville, VA; 2University of Virginia, Charlottesville, VA; 3University of Virginia Medical Center, Charlottesville, VA
Introduction: Simple hepatic cysts are common incidental findings on abdominal imaging and are typically managed expectantly if asymptomatic. However, symptoms can develop due to mass effect, infection, rupture, or hemorrhage of the cyst in which case intervention is warranted. We describe a unique case of a large hepatic cyst causing mass effect with associated intrahepatic portal vein thrombosis (PVT) in an otherwise healthy male.
Case Description/
Methods: A 77-year-old man with previously asymptomatic simple hepatic cysts (Figure 1) presented to his primary care physician with several months of worsening post-prandial right upper quadrant (RUQ) abdominal pain. Ultrasound (US) demonstrated interval enlargement of his cysts without hepatic steatosis, advanced fibrosis, thrombosis, or features of portal hypertension. US-guided aspiration of the largest right lobe cyst successfully removed 1.6 liters of brown fluid; cytology was negative. His pain improved post-procedure; however, the following day he developed worsening RUQ pain prompting emergency department presentation. Contrasted CT demonstrated rapid re-accumulation of the cyst with compression of the right portal vein and acute non-occlusive PVT (Figure 2); he was subsequently admitted. Further drainage was planned with interventional radiology but aborted when intraprocedural US revealed septations. Subsequent contrasted magnetic resonance imaging (MRI) for further definition favored the septations to be sequelae of recent aspiration rather than a biliary cystadenoma. The patient was initiated on apixaban to promote recanalization and prevent further PVT progression. Prior to discharge, surgery was consulted for cyst fenestration of the largest cysts in segment 6 and 7. He underwent an uncomplicated, successful robotic procedure several weeks later in the outpatient setting with full resolution of his RUQ pain. At outpatient hepatology follow-up he was doing well, although on repeat contrasted MRI there was a lack of recanalization of the right intrahepatic portal vein, suggestive of developing chronic thrombosis. His apixaban was continued with planned six-month total course.
Discussion: Portal vein thrombosis is a rare but serious hepatic cyst complication due to mass effect. Multimodal management is necessary when hepatic cysts become symptomatic or recurrent. An acute change in symptoms in patients with a history of hepatic cysts should prompt early contrasted cross-sectional imaging to assess for complications.

Figure: Contrast enhanced computed tomography of the abdomen and pelvis showing the hepatic cyst measuring 13 x 9 cm with patent adjacent right portal vein branches.
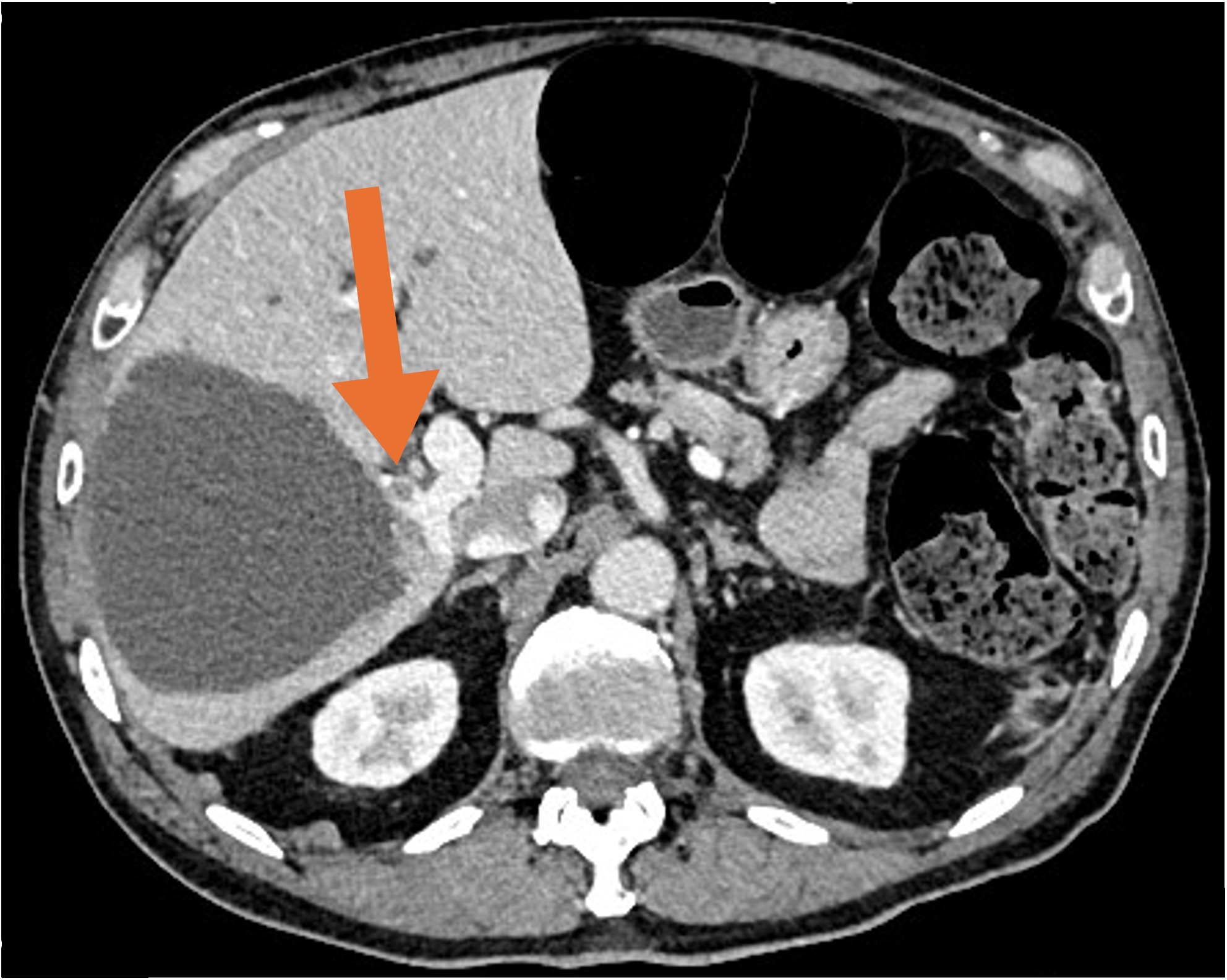
Figure: Contrast enhanced computed tomography of the abdomen and pelvis showing interval decrease in size of the cyst after aspiration with persistent mass effect on the right portal vein and new non-occlusive thrombus in the anterior branch of the right portal vein.
Disclosures:
Claire Maher indicated no relevant financial relationships.
Ana Lopez Alvarez indicated no relevant financial relationships.
Emily Minor indicated no relevant financial relationships.
Samantha Epstein indicated no relevant financial relationships.
Brian Wentworth: GSK – Consultant. Ipsen – Consultant, Speakers Bureau. Luna Labs USA, LLC – Consultant.
Claire F. Maher, BA1, Ana S. Lopez Alvarez, BS, MS1, Emily Minor, MD, PhD2, Samantha Epstein, MD3, Brian J. Wentworth, MD, MS2. P1716 - Beware the “Benign” Hepatic Cyst: Mass Effect Causing Portal Vein Thrombosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Virginia School of Medicine, Charlottesville, VA; 2University of Virginia, Charlottesville, VA; 3University of Virginia Medical Center, Charlottesville, VA
Introduction: Simple hepatic cysts are common incidental findings on abdominal imaging and are typically managed expectantly if asymptomatic. However, symptoms can develop due to mass effect, infection, rupture, or hemorrhage of the cyst in which case intervention is warranted. We describe a unique case of a large hepatic cyst causing mass effect with associated intrahepatic portal vein thrombosis (PVT) in an otherwise healthy male.
Case Description/
Methods: A 77-year-old man with previously asymptomatic simple hepatic cysts (Figure 1) presented to his primary care physician with several months of worsening post-prandial right upper quadrant (RUQ) abdominal pain. Ultrasound (US) demonstrated interval enlargement of his cysts without hepatic steatosis, advanced fibrosis, thrombosis, or features of portal hypertension. US-guided aspiration of the largest right lobe cyst successfully removed 1.6 liters of brown fluid; cytology was negative. His pain improved post-procedure; however, the following day he developed worsening RUQ pain prompting emergency department presentation. Contrasted CT demonstrated rapid re-accumulation of the cyst with compression of the right portal vein and acute non-occlusive PVT (Figure 2); he was subsequently admitted. Further drainage was planned with interventional radiology but aborted when intraprocedural US revealed septations. Subsequent contrasted magnetic resonance imaging (MRI) for further definition favored the septations to be sequelae of recent aspiration rather than a biliary cystadenoma. The patient was initiated on apixaban to promote recanalization and prevent further PVT progression. Prior to discharge, surgery was consulted for cyst fenestration of the largest cysts in segment 6 and 7. He underwent an uncomplicated, successful robotic procedure several weeks later in the outpatient setting with full resolution of his RUQ pain. At outpatient hepatology follow-up he was doing well, although on repeat contrasted MRI there was a lack of recanalization of the right intrahepatic portal vein, suggestive of developing chronic thrombosis. His apixaban was continued with planned six-month total course.
Discussion: Portal vein thrombosis is a rare but serious hepatic cyst complication due to mass effect. Multimodal management is necessary when hepatic cysts become symptomatic or recurrent. An acute change in symptoms in patients with a history of hepatic cysts should prompt early contrasted cross-sectional imaging to assess for complications.

Figure: Contrast enhanced computed tomography of the abdomen and pelvis showing the hepatic cyst measuring 13 x 9 cm with patent adjacent right portal vein branches.
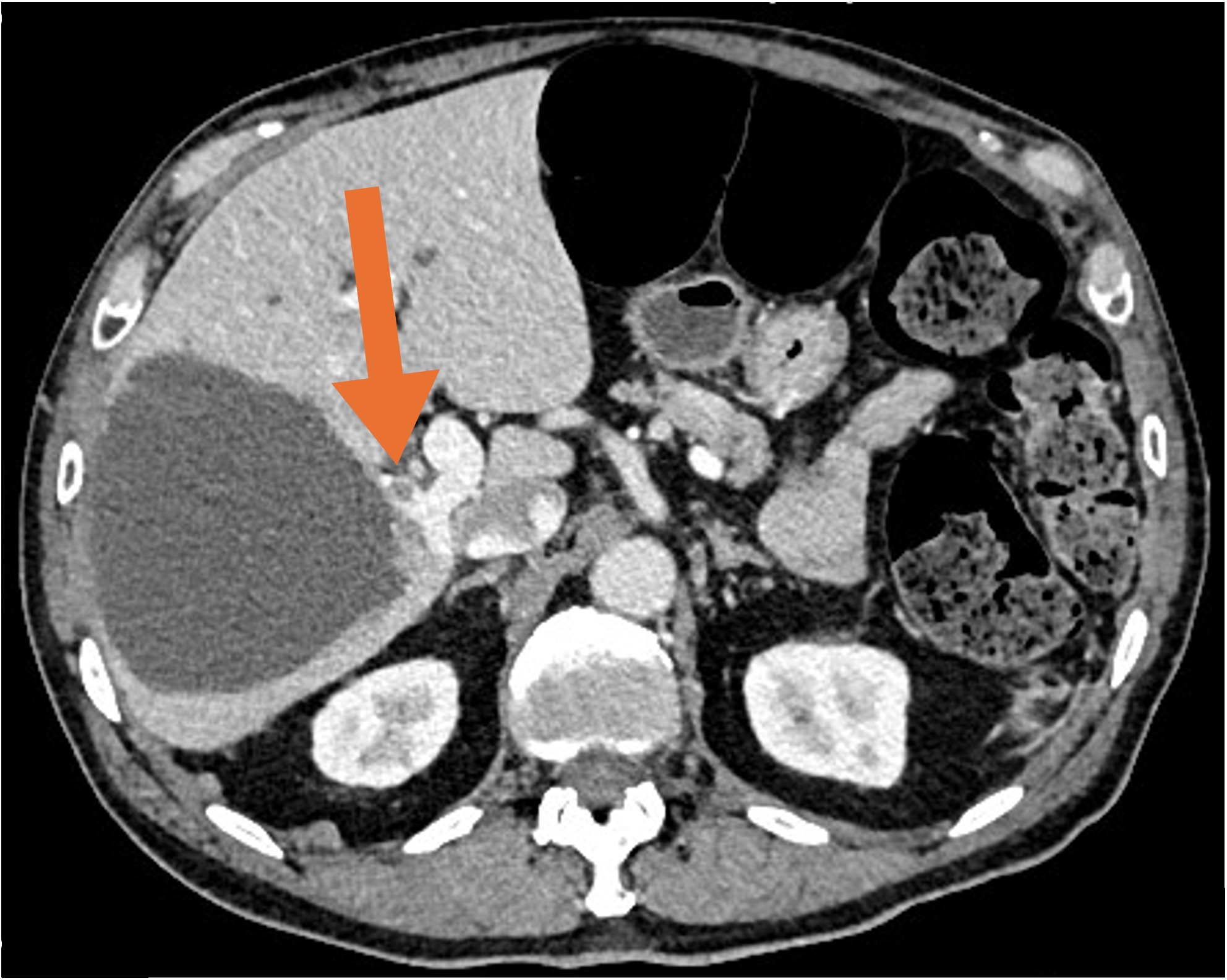
Figure: Contrast enhanced computed tomography of the abdomen and pelvis showing interval decrease in size of the cyst after aspiration with persistent mass effect on the right portal vein and new non-occlusive thrombus in the anterior branch of the right portal vein.
Disclosures:
Claire Maher indicated no relevant financial relationships.
Ana Lopez Alvarez indicated no relevant financial relationships.
Emily Minor indicated no relevant financial relationships.
Samantha Epstein indicated no relevant financial relationships.
Brian Wentworth: GSK – Consultant. Ipsen – Consultant, Speakers Bureau. Luna Labs USA, LLC – Consultant.
Claire F. Maher, BA1, Ana S. Lopez Alvarez, BS, MS1, Emily Minor, MD, PhD2, Samantha Epstein, MD3, Brian J. Wentworth, MD, MS2. P1716 - Beware the “Benign” Hepatic Cyst: Mass Effect Causing Portal Vein Thrombosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
