Sunday Poster Session
Category: Liver
P1713 - Acute Liver Injury During Pregnancy: A Challenging Diagnosis of Autoimmune Hepatitis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- ZK
Zach Kovach, MD
West Virginia University School of Medicine
Morgantown, WV
Presenting Author(s)
Katherine Shepherd, MD1, Zach Kovach, MD2, Rehmat Awan, MD2, Anastasia Digman, PharmD2, Kanwarpreet Tandon, MBBS2, Jennifer Hadam-Veverka, MD2
1West Virginia University, Morgantown, WV; 2West Virginia University School of Medicine, Morgantown, WV
Introduction: The etiology of autoimmune hepatitis (AIH) is multifactorial including genetic susceptibility often in conjunction with environmental triggers. This culmination of factors results in a T-cell mediated immune response leading to persistent inflammation of the liver. AIH is more common in women and classically presents in child-bearing aged women. During pregnancy, AIH can have increased maternal and fetal complications.
Case Description/
Methods: We present a 27-year-old female with a diagnosis of Crohn’s disease with recent infliximab induction. She improved clinically and became pregnant. At 23 weeks gestation, she presented with severe pruritis and scleral icterus. Laboratory testing revealed elevated bile acids, bilirubin, and liver enzymes (Table 1). Intrahepatic cholestasis of pregnancy (ICP) was thought to be contributing, but unlikely to explain the severity of liver enzyme elevation. Imaging with RUQ ultrasound and MRCP were unremarkable. Infectious workup including serologies for CMV, HSV, EBV, HAV, HBV, HCV, and HIV were negative. Autoimmune work up was significant for positive anti-nuclear antibody (1:320), but anti-mitochondrial antibody and anti-smooth muscle antibody were negative. Infliximab was held for concern of DILI. A liver biopsy was performed which showed acute and subacute panlobular hepatitis with hepatocanalicular cholestasis. Multidisciplinary review including transplant hepatology and pathology believed the presentation was most consistent with underlying autoimmune process triggered by DILI and pregnancy. Prednisone was initiated, and she was continued on 40 mg prednisone with normalization of liver enzymes. She delivered at 32 weeks due to premature rupture of membranes. After delivery, she was started on azathioprine and prednisone was tapered by 5 mg weekly.
Discussion: Diagnosing and managing acute liver injury during pregnancy is challenging, as it requires balancing the need for accurate identification and treatment of the liver condition, while minimizing risk to the fetus. While her elevated bile acid levels and pruritis were indicative of ICP, the severity of her elevated liver enzymes warranted additional workup. Underlying Crohn’s disease with infliximab exposure during pregnancy likely triggered AIH. This case emphasizes the importance of recognizing coexisting liver processes during pregnancy that can have detrimental maternal and fetal outcomes if left untreated.
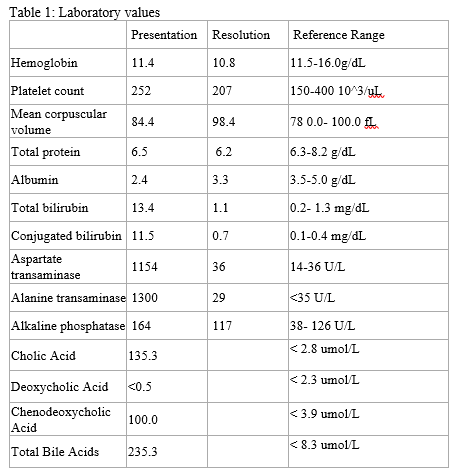
Figure: Table 1: Laboratory Values
Disclosures:
Katherine Shepherd indicated no relevant financial relationships.
Zach Kovach indicated no relevant financial relationships.
Rehmat Awan indicated no relevant financial relationships.
Anastasia Digman indicated no relevant financial relationships.
Kanwarpreet Tandon indicated no relevant financial relationships.
Jennifer Hadam-Veverka: Abbvie – Speakers Bureau. Johnson & Johnson – Speakers Bureau. Takeda – Speakers Bureau.
Katherine Shepherd, MD1, Zach Kovach, MD2, Rehmat Awan, MD2, Anastasia Digman, PharmD2, Kanwarpreet Tandon, MBBS2, Jennifer Hadam-Veverka, MD2. P1713 - Acute Liver Injury During Pregnancy: A Challenging Diagnosis of Autoimmune Hepatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1West Virginia University, Morgantown, WV; 2West Virginia University School of Medicine, Morgantown, WV
Introduction: The etiology of autoimmune hepatitis (AIH) is multifactorial including genetic susceptibility often in conjunction with environmental triggers. This culmination of factors results in a T-cell mediated immune response leading to persistent inflammation of the liver. AIH is more common in women and classically presents in child-bearing aged women. During pregnancy, AIH can have increased maternal and fetal complications.
Case Description/
Methods: We present a 27-year-old female with a diagnosis of Crohn’s disease with recent infliximab induction. She improved clinically and became pregnant. At 23 weeks gestation, she presented with severe pruritis and scleral icterus. Laboratory testing revealed elevated bile acids, bilirubin, and liver enzymes (Table 1). Intrahepatic cholestasis of pregnancy (ICP) was thought to be contributing, but unlikely to explain the severity of liver enzyme elevation. Imaging with RUQ ultrasound and MRCP were unremarkable. Infectious workup including serologies for CMV, HSV, EBV, HAV, HBV, HCV, and HIV were negative. Autoimmune work up was significant for positive anti-nuclear antibody (1:320), but anti-mitochondrial antibody and anti-smooth muscle antibody were negative. Infliximab was held for concern of DILI. A liver biopsy was performed which showed acute and subacute panlobular hepatitis with hepatocanalicular cholestasis. Multidisciplinary review including transplant hepatology and pathology believed the presentation was most consistent with underlying autoimmune process triggered by DILI and pregnancy. Prednisone was initiated, and she was continued on 40 mg prednisone with normalization of liver enzymes. She delivered at 32 weeks due to premature rupture of membranes. After delivery, she was started on azathioprine and prednisone was tapered by 5 mg weekly.
Discussion: Diagnosing and managing acute liver injury during pregnancy is challenging, as it requires balancing the need for accurate identification and treatment of the liver condition, while minimizing risk to the fetus. While her elevated bile acid levels and pruritis were indicative of ICP, the severity of her elevated liver enzymes warranted additional workup. Underlying Crohn’s disease with infliximab exposure during pregnancy likely triggered AIH. This case emphasizes the importance of recognizing coexisting liver processes during pregnancy that can have detrimental maternal and fetal outcomes if left untreated.
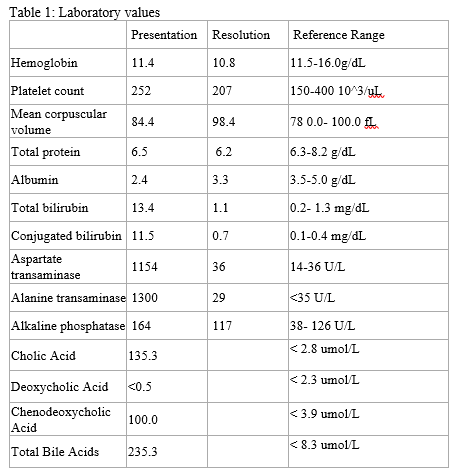
Figure: Table 1: Laboratory Values
Disclosures:
Katherine Shepherd indicated no relevant financial relationships.
Zach Kovach indicated no relevant financial relationships.
Rehmat Awan indicated no relevant financial relationships.
Anastasia Digman indicated no relevant financial relationships.
Kanwarpreet Tandon indicated no relevant financial relationships.
Jennifer Hadam-Veverka: Abbvie – Speakers Bureau. Johnson & Johnson – Speakers Bureau. Takeda – Speakers Bureau.
Katherine Shepherd, MD1, Zach Kovach, MD2, Rehmat Awan, MD2, Anastasia Digman, PharmD2, Kanwarpreet Tandon, MBBS2, Jennifer Hadam-Veverka, MD2. P1713 - Acute Liver Injury During Pregnancy: A Challenging Diagnosis of Autoimmune Hepatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
