Sunday Poster Session
Category: Liver
Unmasking Hepatic Brucelloma: A Rare Mimic of Malignancy in a Case of <i>Brucella melitensis</i> Infection
P1791 - Unmasking Hepatic Brucelloma: A Rare Mimic of Malignancy in a Case of Brucella melitensis Infection
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- GD
Grecia Dominguez Rivera, MD
University of Texas Health San Antonio
San Antonio, TX
Presenting Author(s)
Grecia Dominguez Rivera, MD1, Emilio Fernandez, MD1, Fabian Rodas, MD2, Eugenia Tsai, MD2, Lisa D. Pedicone, PhD2, Andres Gomez-Aldana, MD2, Carmen Landaverde, MD2, Jan Petrasek, MD, PhD2, Eric Lawitz, MD3, Fred Poordad, MD2
1University of Texas Health San Antonio, San Antonio, TX; 2Texas Liver Institute, Austin, TX; 3Texas Liver Institute, San Antonio, TX
Introduction: Hepatic brucelloma is an uncommon sequela of brucellosis, the most prevalent zoonotic disease worldwide, predominantly observed in certain endemic regions with diverse clinical presentations. Considering the pathogen’s predilection for the reticuloendothelial system, liver involvement in brucellosis is almost invariable.
Case Description/
Methods: A 44-year-old Hispanic male with a past medical history of hypertension, hyperlipidemia, and recurrent diverticulitis presented with a five-day history of right upper quadrant pain. Initial labs revealed leukocytosis (12.07 x 10³/μL) and normal serum aminotransferases. CT of the abdomen and pelvis (CT A/P) showed a 7.1 cm heterogeneous mass with internal calcification in the right hepatic lobe, extending along the infrahepatic surface to form a 3.2 cm exophytic soft tissue component with hypoattenuation. Four-phase CT demonstrated lack of arterial enhancement and extension to the adjacent anterior abdominal wall and hepatic flexure of the colon. US-guided liver biopsy showed vaguely granulomatous inflammation with abundant reactive plasma cells. Further systemic granulomatous etiologies revealed a positive Brucella agglutination test with a titer of 1:80. Subsequent Karius testing confirmed Brucella melitensis. He completed a seven-day course of IV gentamicin and started a regimen of doxycycline and rifampin. A repeat CT A/P at six weeks showed interval decrease in brucelloma size. The antibiotic regimen was subsequently adjusted with treatment ongoing at the time of submission.
Discussion: Brucellosis affects the liver in various ways, ranging from benign subclinical increases in serum aminotransferase levels to more severe manifestations such as chronic suppurative disease. However, in this case, the patient presented unusually with a large liver mass associated with normal serum aminotransferases that raised significant concern for malignancy. Noninvasive diagnostic tools, including serological and radiological assessments, were critical in guiding the diagnosis. Different histologic patterns can be observed, the most common being granuloma formation. In our case, the diagnosis was confirmed by Karius testing, which detects microbial cell-free DNA in plasma and offers high sensitivity, especially when traditional cultures yield negative results. This case highlights the importance of considering hepatic brucelloma in the differential diagnosis of hepatic masses, even when they display invasive behavior, such as that seen in our patient.
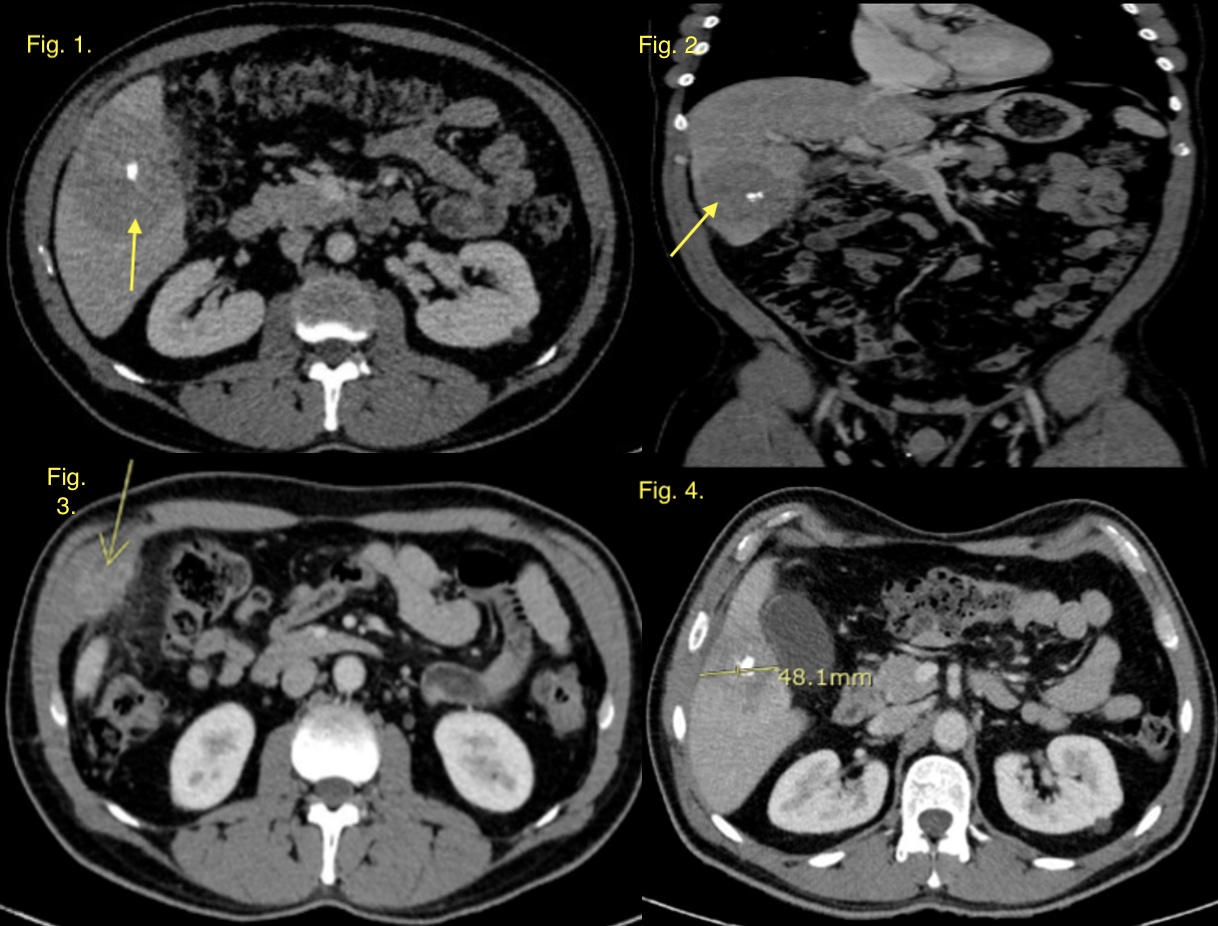
Figure: Fig. 1 and 2 CT A/P on 01/15/2025 showing a 7.1 cm heterogeneous mass with internal calcification in the right hepatic lobe, extending along the infrahepatic surface. Fig. 3 and 4 CT A/P on 04/02/2025 showing decreased centrally calcified hepatic segment 5/6 abscess, now measuring 6.2 cm
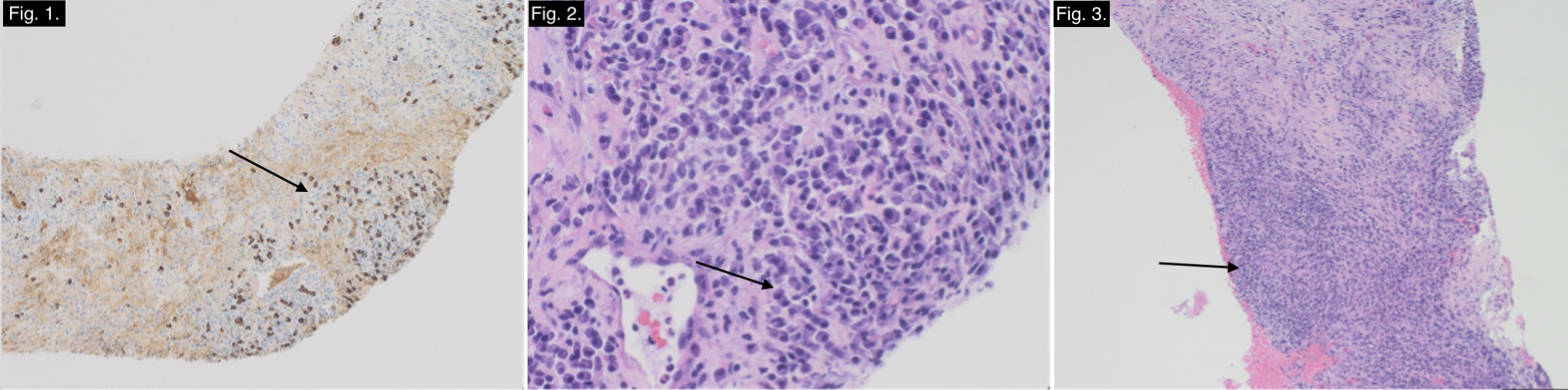
Figure: H&E stained sections of liver show marked inflammation (Fig. 1) consisting of numerous plasma cells (Fig. 2) including a subset of IgG4+ plasma cells (Fig. 3). Additional special stains (GMS and AFB) were negative for fungal organisms and acid fast bacilli.
Disclosures:
Grecia Dominguez Rivera indicated no relevant financial relationships.
Emilio Fernandez indicated no relevant financial relationships.
Fabian Rodas indicated no relevant financial relationships.
Eugenia Tsai indicated no relevant financial relationships.
Lisa D. Pedicone indicated no relevant financial relationships.
Andres Gomez-Aldana indicated no relevant financial relationships.
Carmen Landaverde indicated no relevant financial relationships.
Jan Petrasek indicated no relevant financial relationships.
Eric Lawitz: 89 Bio INC – Consultant, Grant/Research Support, Speakers Bureau. Abbvie – Speakers Bureau. Akero Therapeitics – Grant/Research Support. Alnylam Phamaceuticals INC – Grant/Research Support. Amgen – Grant/Research Support. Aztrazeneca – Consultant, Grant/Research Support. Bioscience – Grant/Research Support. Boehringer Ingelheim – Consultant, Grant/Research Support. Bristol-Myers Squibb – Grant/Research Support. Corcept Therapeutics – Consultant, Grant/Research Support. Cour Pharmaceuticals Inc – Grant/Research Support. Cymabay Therapeutics – Grant/Research Support. Eli Lily and Company – Consultant, Grant/Research Support. Enanta Pharmaceuticals – Grant/Research Support. Enyo Pharma – Grant/Research Support. Exalenz – Grant/Research Support. Galectin Therapeutics – Grant/Research Support. Galmed Pharmaceuticals – Grant/Research Support. Genfit – Grant/Research Support. Gilead Sciences – Grant/Research Support, Speakers Bureau. GlaxoSmithKline – Grant/Research Support. Hanmi Pharmaceuticals – Grant/Research Support. Hightide Biopharma – Grant/Research Support. Intercept Pharmaceuticals – Grant/Research Support, Speakers Bureau. Inventiva – Grant/Research Support. Ipsen – Grant/Research Support. Jansen Pharmaceuticals – Grant/Research Support. Madrigal Pharmaceuticals – Grant/Research Support, Speakers Bureau. Merck & Co – Consultant, Grant/Research Support. NGM Biopharmaceuticals Inc – Grant/Research Support. Northsea Therapeutics – Grant/Research Support. Novartis – Grant/Research Support. Novo Nordisk Inc – Consultant, Grant/Research Support. Organovo – Consultant, Grant/Research Support. Poxel Co – Grant/Research Support. Regeneron – Consultant, Grant/Research Support. Sagimet Biosciences – Consultant, Grant/Research Support. Takeda – Grant/Research Support. Terns pharmaceuticals – Grant/Research Support. Viking Therapeutics – Grant/Research Support. Zydus Pharmaceuticals – Grant/Research Support.
Fred Poordad indicated no relevant financial relationships.
Grecia Dominguez Rivera, MD1, Emilio Fernandez, MD1, Fabian Rodas, MD2, Eugenia Tsai, MD2, Lisa D. Pedicone, PhD2, Andres Gomez-Aldana, MD2, Carmen Landaverde, MD2, Jan Petrasek, MD, PhD2, Eric Lawitz, MD3, Fred Poordad, MD2. P1791 - Unmasking Hepatic Brucelloma: A Rare Mimic of Malignancy in a Case of <i>Brucella melitensis</i> Infection, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Texas Health San Antonio, San Antonio, TX; 2Texas Liver Institute, Austin, TX; 3Texas Liver Institute, San Antonio, TX
Introduction: Hepatic brucelloma is an uncommon sequela of brucellosis, the most prevalent zoonotic disease worldwide, predominantly observed in certain endemic regions with diverse clinical presentations. Considering the pathogen’s predilection for the reticuloendothelial system, liver involvement in brucellosis is almost invariable.
Case Description/
Methods: A 44-year-old Hispanic male with a past medical history of hypertension, hyperlipidemia, and recurrent diverticulitis presented with a five-day history of right upper quadrant pain. Initial labs revealed leukocytosis (12.07 x 10³/μL) and normal serum aminotransferases. CT of the abdomen and pelvis (CT A/P) showed a 7.1 cm heterogeneous mass with internal calcification in the right hepatic lobe, extending along the infrahepatic surface to form a 3.2 cm exophytic soft tissue component with hypoattenuation. Four-phase CT demonstrated lack of arterial enhancement and extension to the adjacent anterior abdominal wall and hepatic flexure of the colon. US-guided liver biopsy showed vaguely granulomatous inflammation with abundant reactive plasma cells. Further systemic granulomatous etiologies revealed a positive Brucella agglutination test with a titer of 1:80. Subsequent Karius testing confirmed Brucella melitensis. He completed a seven-day course of IV gentamicin and started a regimen of doxycycline and rifampin. A repeat CT A/P at six weeks showed interval decrease in brucelloma size. The antibiotic regimen was subsequently adjusted with treatment ongoing at the time of submission.
Discussion: Brucellosis affects the liver in various ways, ranging from benign subclinical increases in serum aminotransferase levels to more severe manifestations such as chronic suppurative disease. However, in this case, the patient presented unusually with a large liver mass associated with normal serum aminotransferases that raised significant concern for malignancy. Noninvasive diagnostic tools, including serological and radiological assessments, were critical in guiding the diagnosis. Different histologic patterns can be observed, the most common being granuloma formation. In our case, the diagnosis was confirmed by Karius testing, which detects microbial cell-free DNA in plasma and offers high sensitivity, especially when traditional cultures yield negative results. This case highlights the importance of considering hepatic brucelloma in the differential diagnosis of hepatic masses, even when they display invasive behavior, such as that seen in our patient.
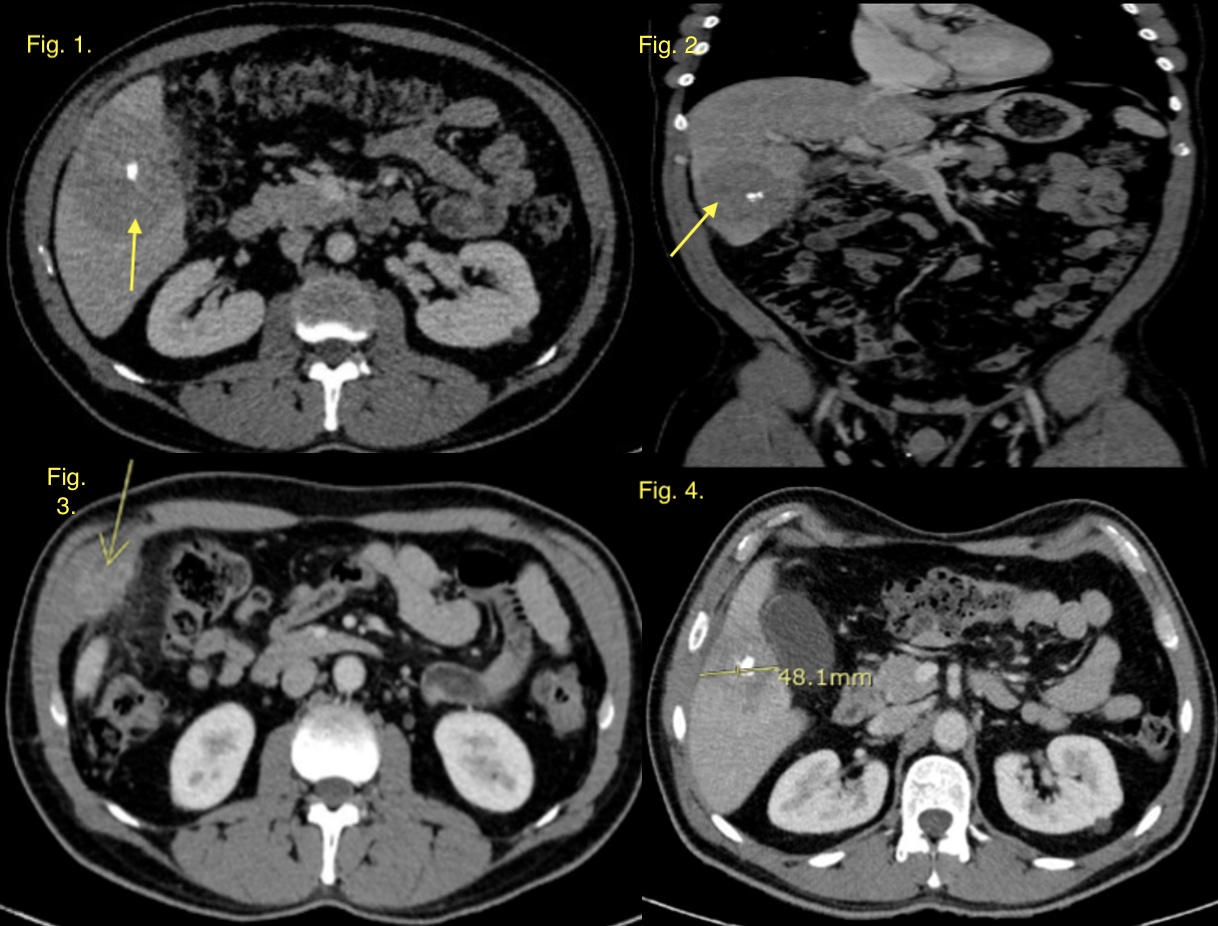
Figure: Fig. 1 and 2 CT A/P on 01/15/2025 showing a 7.1 cm heterogeneous mass with internal calcification in the right hepatic lobe, extending along the infrahepatic surface. Fig. 3 and 4 CT A/P on 04/02/2025 showing decreased centrally calcified hepatic segment 5/6 abscess, now measuring 6.2 cm
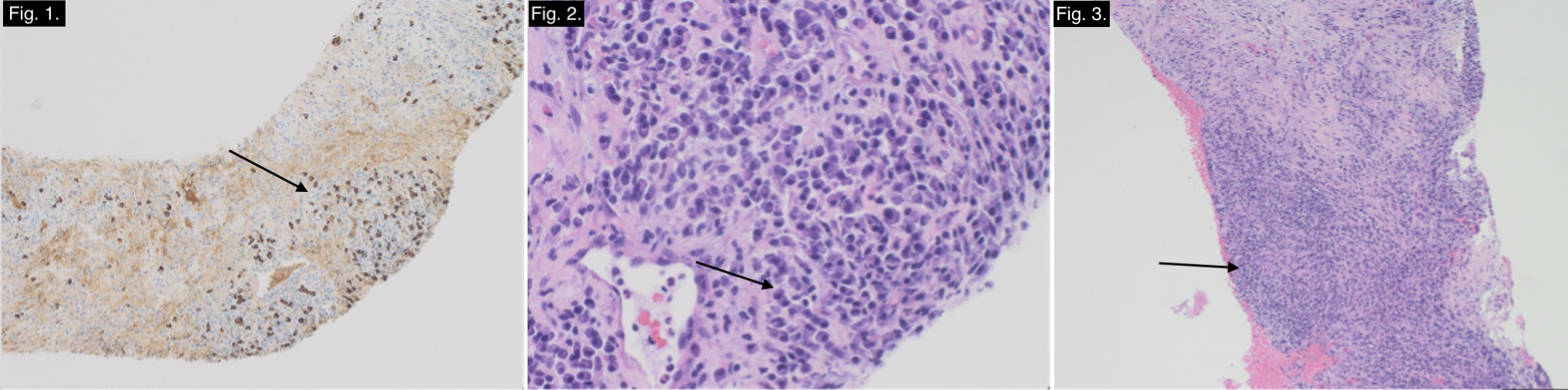
Figure: H&E stained sections of liver show marked inflammation (Fig. 1) consisting of numerous plasma cells (Fig. 2) including a subset of IgG4+ plasma cells (Fig. 3). Additional special stains (GMS and AFB) were negative for fungal organisms and acid fast bacilli.
Disclosures:
Grecia Dominguez Rivera indicated no relevant financial relationships.
Emilio Fernandez indicated no relevant financial relationships.
Fabian Rodas indicated no relevant financial relationships.
Eugenia Tsai indicated no relevant financial relationships.
Lisa D. Pedicone indicated no relevant financial relationships.
Andres Gomez-Aldana indicated no relevant financial relationships.
Carmen Landaverde indicated no relevant financial relationships.
Jan Petrasek indicated no relevant financial relationships.
Eric Lawitz: 89 Bio INC – Consultant, Grant/Research Support, Speakers Bureau. Abbvie – Speakers Bureau. Akero Therapeitics – Grant/Research Support. Alnylam Phamaceuticals INC – Grant/Research Support. Amgen – Grant/Research Support. Aztrazeneca – Consultant, Grant/Research Support. Bioscience – Grant/Research Support. Boehringer Ingelheim – Consultant, Grant/Research Support. Bristol-Myers Squibb – Grant/Research Support. Corcept Therapeutics – Consultant, Grant/Research Support. Cour Pharmaceuticals Inc – Grant/Research Support. Cymabay Therapeutics – Grant/Research Support. Eli Lily and Company – Consultant, Grant/Research Support. Enanta Pharmaceuticals – Grant/Research Support. Enyo Pharma – Grant/Research Support. Exalenz – Grant/Research Support. Galectin Therapeutics – Grant/Research Support. Galmed Pharmaceuticals – Grant/Research Support. Genfit – Grant/Research Support. Gilead Sciences – Grant/Research Support, Speakers Bureau. GlaxoSmithKline – Grant/Research Support. Hanmi Pharmaceuticals – Grant/Research Support. Hightide Biopharma – Grant/Research Support. Intercept Pharmaceuticals – Grant/Research Support, Speakers Bureau. Inventiva – Grant/Research Support. Ipsen – Grant/Research Support. Jansen Pharmaceuticals – Grant/Research Support. Madrigal Pharmaceuticals – Grant/Research Support, Speakers Bureau. Merck & Co – Consultant, Grant/Research Support. NGM Biopharmaceuticals Inc – Grant/Research Support. Northsea Therapeutics – Grant/Research Support. Novartis – Grant/Research Support. Novo Nordisk Inc – Consultant, Grant/Research Support. Organovo – Consultant, Grant/Research Support. Poxel Co – Grant/Research Support. Regeneron – Consultant, Grant/Research Support. Sagimet Biosciences – Consultant, Grant/Research Support. Takeda – Grant/Research Support. Terns pharmaceuticals – Grant/Research Support. Viking Therapeutics – Grant/Research Support. Zydus Pharmaceuticals – Grant/Research Support.
Fred Poordad indicated no relevant financial relationships.
Grecia Dominguez Rivera, MD1, Emilio Fernandez, MD1, Fabian Rodas, MD2, Eugenia Tsai, MD2, Lisa D. Pedicone, PhD2, Andres Gomez-Aldana, MD2, Carmen Landaverde, MD2, Jan Petrasek, MD, PhD2, Eric Lawitz, MD3, Fred Poordad, MD2. P1791 - Unmasking Hepatic Brucelloma: A Rare Mimic of Malignancy in a Case of <i>Brucella melitensis</i> Infection, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
