Sunday Poster Session
Category: Liver
P1857 - A Challenging Case of Budd-Chiari Syndrome in a Young Woman With Multiple Thrombophilic Mutations
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- VL
Vy Luong, DO
Ochsner University Hospital & Clinics
Lafayette, LA
Presenting Author(s)
Vy Luong, DO1, Amit Rajkarnikar, MD2, Manpreet Singh, MD2, Melanie Bienvenu, MD, MPH1
1Ochsner University Hospital & Clinics, Lafayette, LA; 2Ochsner LSU Health, Lafayette, LA
Introduction: Budd-Chiari syndrome (BCS) is a rare but serious condition caused by obstruction of the hepatic venous outflow. The clinical presentation often includes hepatomegaly, ascites, and abdominal pain, but diagnosis can be challenging due to its nonspecific symptoms and overlap with other liver conditions. We present the case of Budd-Chiari syndrome secondary to hypercoagulability, complicated by multiple comorbidities and a significant treatment journey.
Case Description/
Methods: We present the case of a 28-year-old female with no significant prior medical history, who was admitted for new-onset dyspnea and right upper back pain. She was initially managed for presumed decompensated liver disease with rapidly re-accumulating ascites. Ascites fluid assessment with protein >2.5 suggestive of possible cardiac ascites but unable to rule out chronic Budd-Chiari Syndrome. Imaging revealed hepatic and portal vein thrombosis, and liver biopsy showed sinusoidal dilatation and central zonal atrophy suggestive of venous outflow obstruction, minimal portal triaditis and periportal and pericellular fibrosis, consistent with venous outflow obstruction. Hypercoagulable workup was notable for protein S deficiency and heterozygous Factor V Leiden mutation. She later developed bilateral pulmonary emboli and had a confirmed history of heparin-induced thrombocytopenia (HIT). Venogram which demonstrated one possible atretic lateral going hepatic vein which was unable to be cannulated. Due to thrombosis and contraindications, she was not a candidate for TIPS. Anticoagulation was managed with warfarin bridged by fondaparinux. She required frequent large-volume paracenteses and was managed for hyponatremia, hypotension, and ascites-related complications. After a comprehensive inpatient evaluation, she was approved and listed for liver transplantation (MELD 22).
Discussion: BCS should be suspected in young patients with unexplained ascites and hepatic congestion. This case illustrates the complexity of managing Budd-Chiari syndrome, particularly in patients with multiple thrombotic risks and limited interventional options. The diagnosis was confirmed with imaging, liver biopsy, and a thorough thrombophilia workup. A combination of anticoagulation, symptomatic management, and potential liver transplantation offers the best chance for improved outcomes in patients with this rare disorder. Despite not being a candidate for TIPS or thrombolysis, the patient remained stable with medical therapy while awaiting transplant.
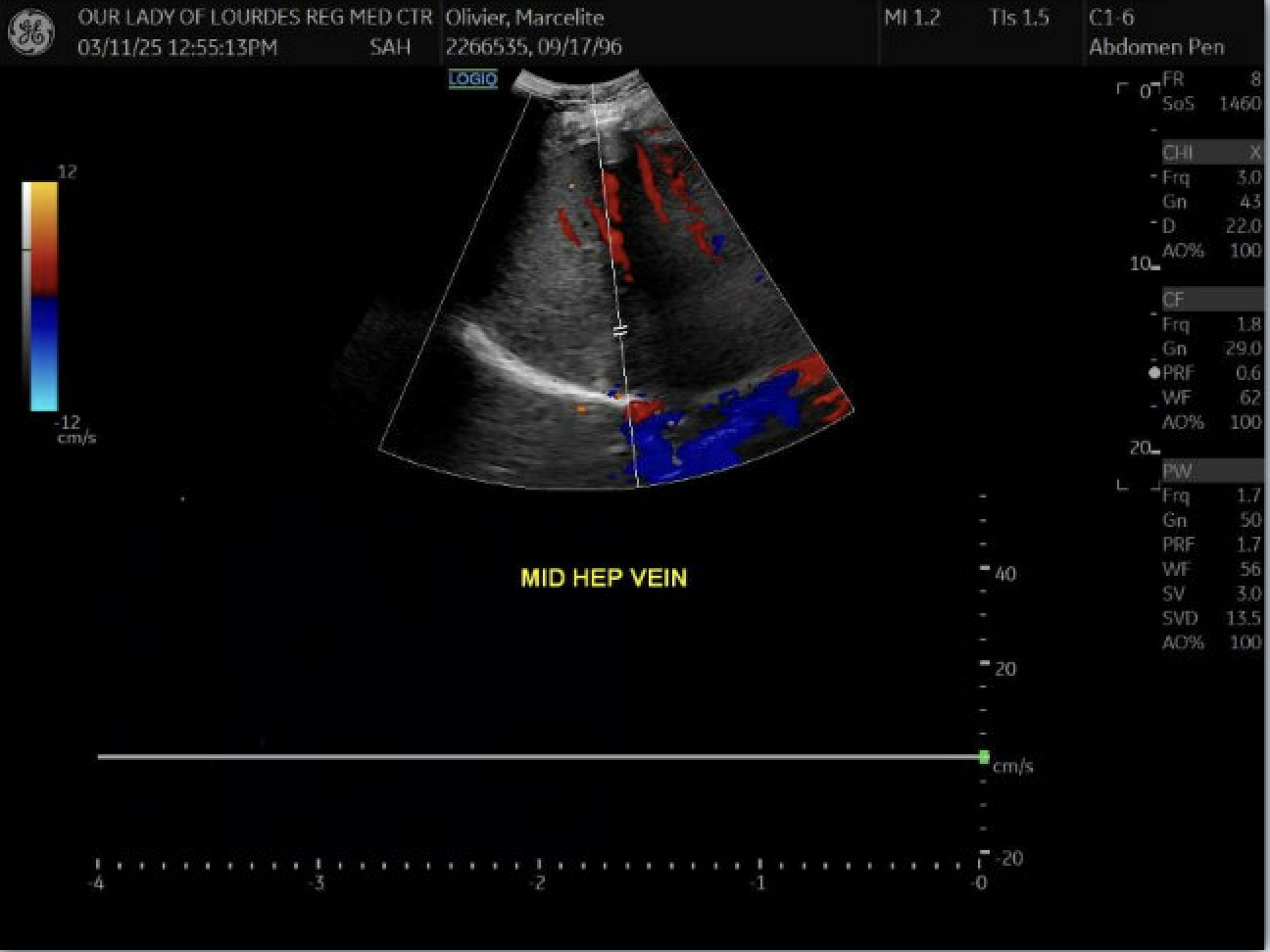
Figure: Suspect thrombosis within the mid hepatic vein
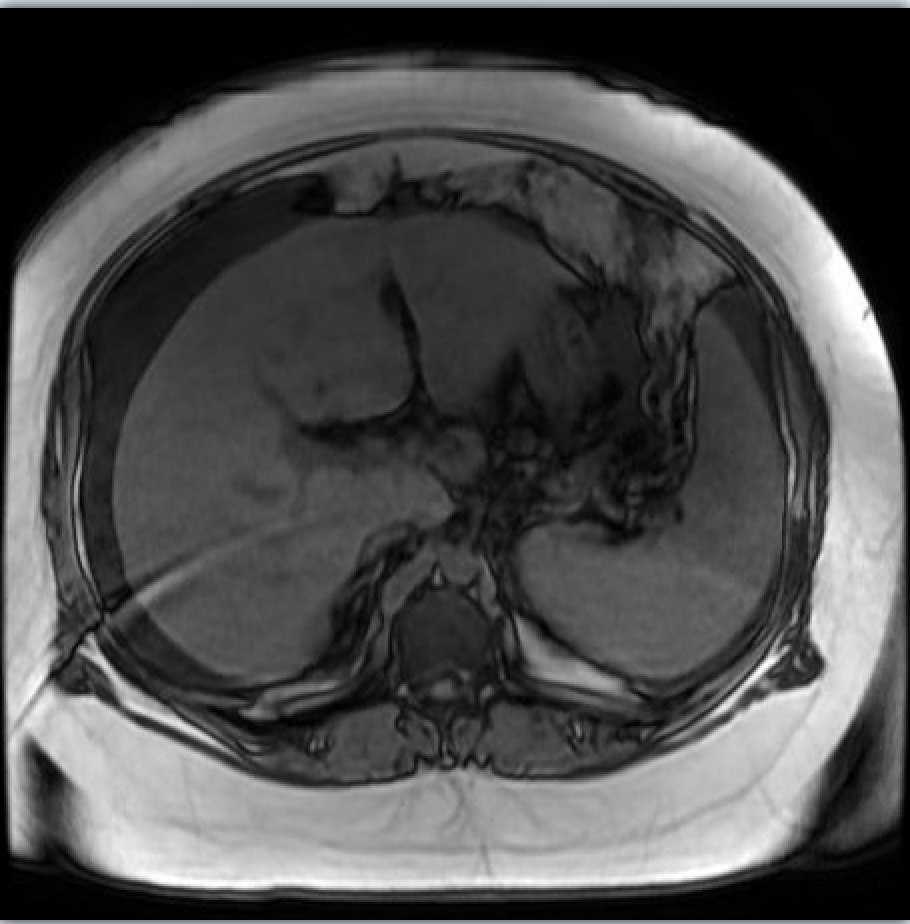
Figure: Hepatosplenomegaly. Inhomogeneous liver parenchyma. Ascites present
Disclosures:
Vy Luong indicated no relevant financial relationships.
Amit Rajkarnikar indicated no relevant financial relationships.
Manpreet Singh indicated no relevant financial relationships.
Melanie Bienvenu indicated no relevant financial relationships.
Vy Luong, DO1, Amit Rajkarnikar, MD2, Manpreet Singh, MD2, Melanie Bienvenu, MD, MPH1. P1857 - A Challenging Case of Budd-Chiari Syndrome in a Young Woman With Multiple Thrombophilic Mutations, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Ochsner University Hospital & Clinics, Lafayette, LA; 2Ochsner LSU Health, Lafayette, LA
Introduction: Budd-Chiari syndrome (BCS) is a rare but serious condition caused by obstruction of the hepatic venous outflow. The clinical presentation often includes hepatomegaly, ascites, and abdominal pain, but diagnosis can be challenging due to its nonspecific symptoms and overlap with other liver conditions. We present the case of Budd-Chiari syndrome secondary to hypercoagulability, complicated by multiple comorbidities and a significant treatment journey.
Case Description/
Methods: We present the case of a 28-year-old female with no significant prior medical history, who was admitted for new-onset dyspnea and right upper back pain. She was initially managed for presumed decompensated liver disease with rapidly re-accumulating ascites. Ascites fluid assessment with protein >2.5 suggestive of possible cardiac ascites but unable to rule out chronic Budd-Chiari Syndrome. Imaging revealed hepatic and portal vein thrombosis, and liver biopsy showed sinusoidal dilatation and central zonal atrophy suggestive of venous outflow obstruction, minimal portal triaditis and periportal and pericellular fibrosis, consistent with venous outflow obstruction. Hypercoagulable workup was notable for protein S deficiency and heterozygous Factor V Leiden mutation. She later developed bilateral pulmonary emboli and had a confirmed history of heparin-induced thrombocytopenia (HIT). Venogram which demonstrated one possible atretic lateral going hepatic vein which was unable to be cannulated. Due to thrombosis and contraindications, she was not a candidate for TIPS. Anticoagulation was managed with warfarin bridged by fondaparinux. She required frequent large-volume paracenteses and was managed for hyponatremia, hypotension, and ascites-related complications. After a comprehensive inpatient evaluation, she was approved and listed for liver transplantation (MELD 22).
Discussion: BCS should be suspected in young patients with unexplained ascites and hepatic congestion. This case illustrates the complexity of managing Budd-Chiari syndrome, particularly in patients with multiple thrombotic risks and limited interventional options. The diagnosis was confirmed with imaging, liver biopsy, and a thorough thrombophilia workup. A combination of anticoagulation, symptomatic management, and potential liver transplantation offers the best chance for improved outcomes in patients with this rare disorder. Despite not being a candidate for TIPS or thrombolysis, the patient remained stable with medical therapy while awaiting transplant.
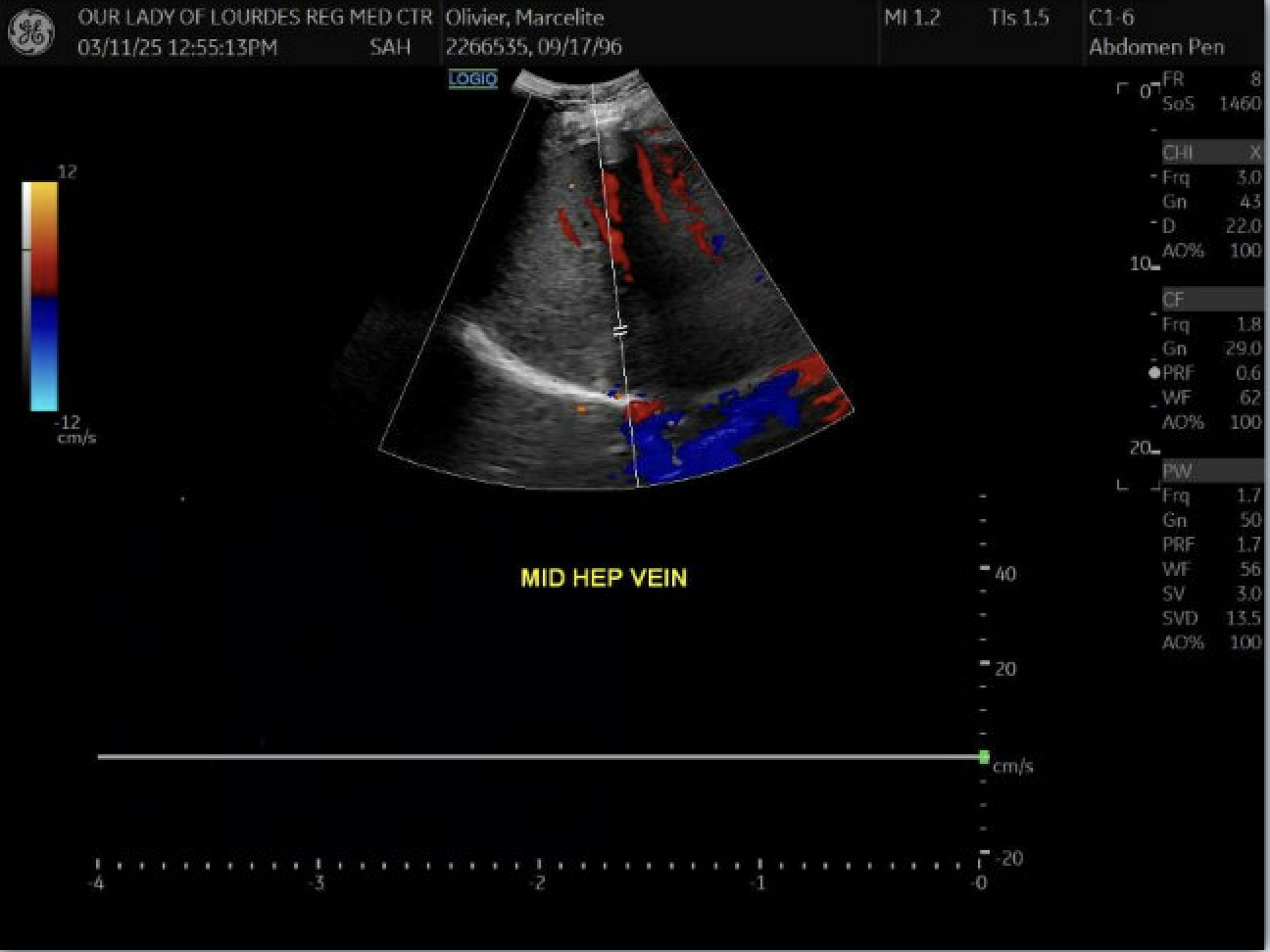
Figure: Suspect thrombosis within the mid hepatic vein
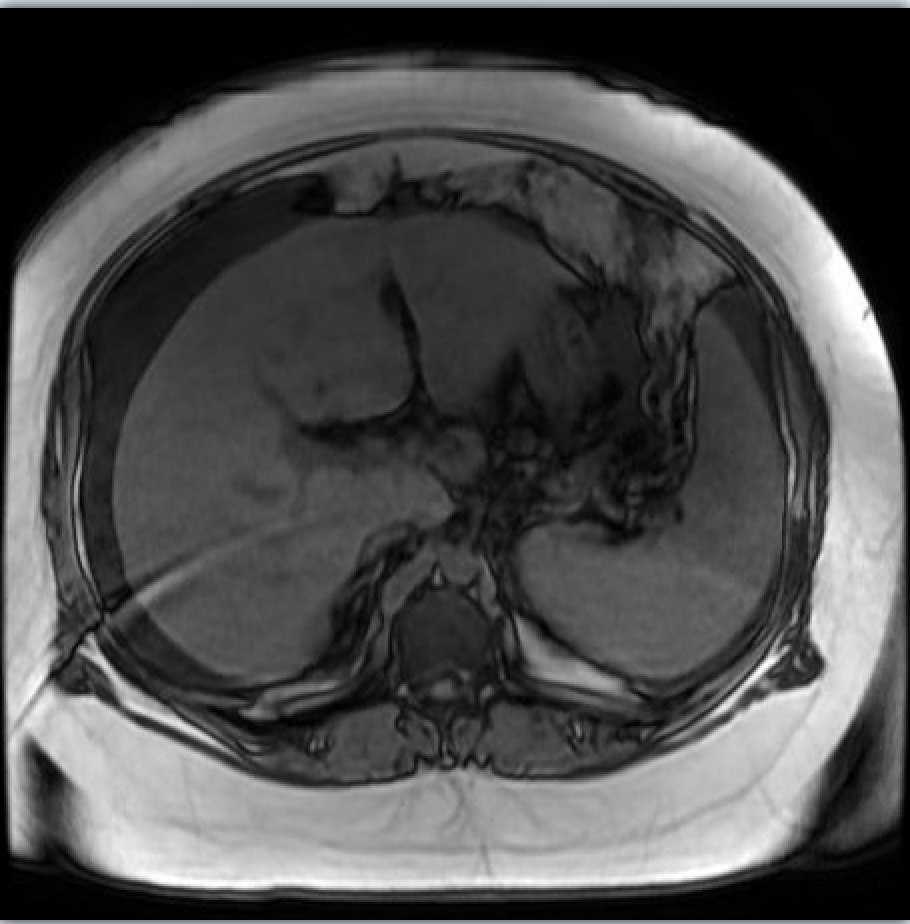
Figure: Hepatosplenomegaly. Inhomogeneous liver parenchyma. Ascites present
Disclosures:
Vy Luong indicated no relevant financial relationships.
Amit Rajkarnikar indicated no relevant financial relationships.
Manpreet Singh indicated no relevant financial relationships.
Melanie Bienvenu indicated no relevant financial relationships.
Vy Luong, DO1, Amit Rajkarnikar, MD2, Manpreet Singh, MD2, Melanie Bienvenu, MD, MPH1. P1857 - A Challenging Case of Budd-Chiari Syndrome in a Young Woman With Multiple Thrombophilic Mutations, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

