Sunday Poster Session
Category: Liver
P1856 - Rectal Bypass to Disaster: A Rare SPSS Revealed on Repeat Imaging
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- DK
Dheeraja Kota, MD
infirmary health
Mobile, AL
Presenting Author(s)
Meghana Kakarla, MD1, Dheeraja Kota, MD2, Moin U. Din, MD2, Giovannie Isaac-Coss, MD3, Zain Alnoah, MD2
1Infirmary Health, Mobile, AL; 2infirmary health, Mobile, AL; 3Rush University Medical Center, Chicago, IL
Introduction: Spontaneous portosystemic shunts (SPSS) are collateral vascular connections that divert portal blood away from the liver in response to portal hypertension. While splenorenal and gastrorenal shunts are commonly encountered, porto-rectal shunts are exceedingly rare and poorly characterized in the literature. We present a case of decompensated cirrhosis with dual pathology: upper GI bleeding from a Dieulafoy lesion and refractory hepatic encephalopathy caused by a SPSS in a rare location (Porto-rectal).
Case Description/
Methods: A 42-year-old man with decompensated cirrhosis secondary to chronic alcohol use presented to us with altered mental status, large-volume hematochezia, and features of decompensated cirrhosis. Initial labs revealed severe anemia, elevated creatinine, lactic acidosis, and hyperammonemia.
Despite identifying and treating a rare dieulafoy lesion in endoscopy, controlling infection and adequate volume resuscitation, the patient’s ammonia levels remained high, and he continued to exhibit stage IV encephalopathy. Given the clinical suspicion of an occult SPSS, we performed contrast-enhanced CT imaging. Common shunts, such as splenorenal or gastrorenal, were not seen. Just when we thought we had ruled out every cause, only a repeat CT scan revealed an SPSS in exceedingly rare location -in between portal vein and rectal vein. Targeted embolization of this shunt, even though it exacerbates other complications of portal hypertension, including worsening ascites or development of other varices, is the best chance we saw in improving his mental status. It led to a dramatic improvement in his mental status and successful extubation. Unfortunately, despite a high MELD score, the patient was not a candidate for liver transplantation due to ongoing alcohol use and poor socioeconomic support and ultimately succumbed to complications of end-stage liver disease.
Discussion: This case highlights the diagnostic challenge posed by SPSS in an unanticipated location like Porto-rectal shunt that is often missed on initial imaging. It also emphasizes the importance of repeat advanced imaging in revealing hidden culprit when initial workup fails to explain persistent encephalopathy. Recognizing and treating these hidden shunts can dramatically reverse the life-threatening neurocognitive decline in cirrhotic patients.
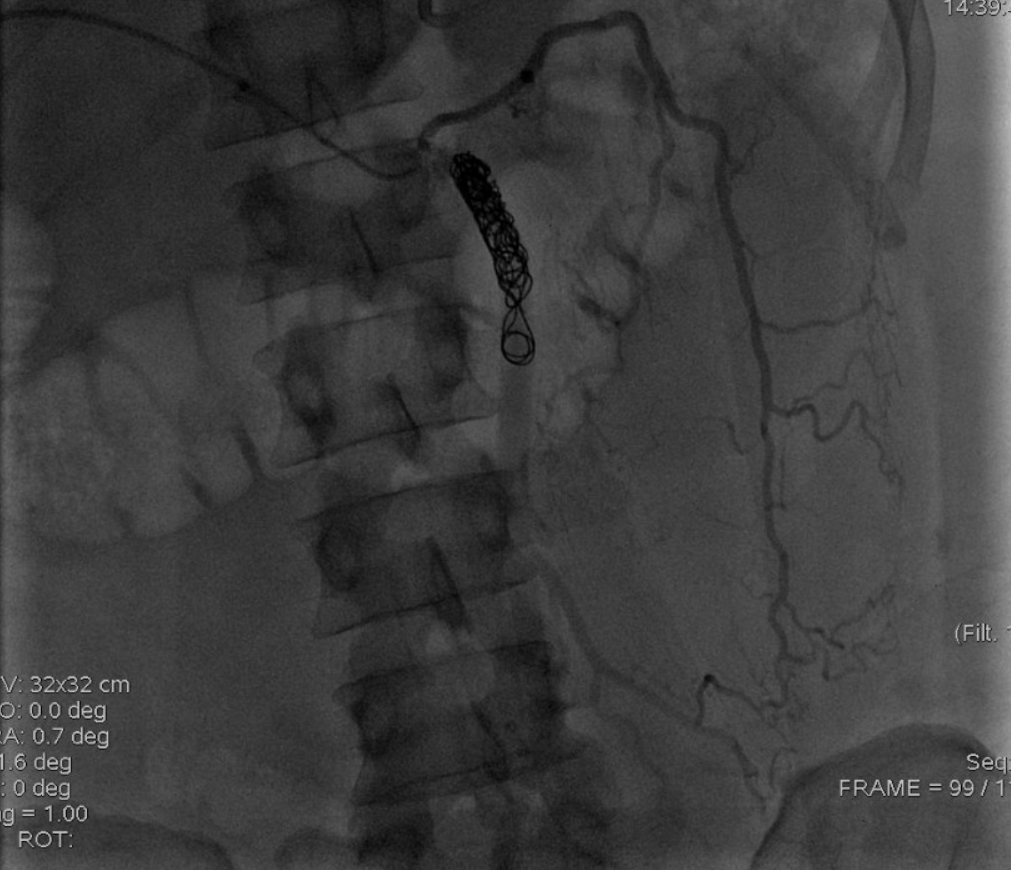
Figure: Portorectal shunt embolized
Disclosures:
Meghana Kakarla indicated no relevant financial relationships.
Dheeraja Kota indicated no relevant financial relationships.
Moin Din indicated no relevant financial relationships.
Giovannie Isaac-Coss indicated no relevant financial relationships.
Zain Alnoah indicated no relevant financial relationships.
Meghana Kakarla, MD1, Dheeraja Kota, MD2, Moin U. Din, MD2, Giovannie Isaac-Coss, MD3, Zain Alnoah, MD2. P1856 - Rectal Bypass to Disaster: A Rare SPSS Revealed on Repeat Imaging, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Infirmary Health, Mobile, AL; 2infirmary health, Mobile, AL; 3Rush University Medical Center, Chicago, IL
Introduction: Spontaneous portosystemic shunts (SPSS) are collateral vascular connections that divert portal blood away from the liver in response to portal hypertension. While splenorenal and gastrorenal shunts are commonly encountered, porto-rectal shunts are exceedingly rare and poorly characterized in the literature. We present a case of decompensated cirrhosis with dual pathology: upper GI bleeding from a Dieulafoy lesion and refractory hepatic encephalopathy caused by a SPSS in a rare location (Porto-rectal).
Case Description/
Methods: A 42-year-old man with decompensated cirrhosis secondary to chronic alcohol use presented to us with altered mental status, large-volume hematochezia, and features of decompensated cirrhosis. Initial labs revealed severe anemia, elevated creatinine, lactic acidosis, and hyperammonemia.
Despite identifying and treating a rare dieulafoy lesion in endoscopy, controlling infection and adequate volume resuscitation, the patient’s ammonia levels remained high, and he continued to exhibit stage IV encephalopathy. Given the clinical suspicion of an occult SPSS, we performed contrast-enhanced CT imaging. Common shunts, such as splenorenal or gastrorenal, were not seen. Just when we thought we had ruled out every cause, only a repeat CT scan revealed an SPSS in exceedingly rare location -in between portal vein and rectal vein. Targeted embolization of this shunt, even though it exacerbates other complications of portal hypertension, including worsening ascites or development of other varices, is the best chance we saw in improving his mental status. It led to a dramatic improvement in his mental status and successful extubation. Unfortunately, despite a high MELD score, the patient was not a candidate for liver transplantation due to ongoing alcohol use and poor socioeconomic support and ultimately succumbed to complications of end-stage liver disease.
Discussion: This case highlights the diagnostic challenge posed by SPSS in an unanticipated location like Porto-rectal shunt that is often missed on initial imaging. It also emphasizes the importance of repeat advanced imaging in revealing hidden culprit when initial workup fails to explain persistent encephalopathy. Recognizing and treating these hidden shunts can dramatically reverse the life-threatening neurocognitive decline in cirrhotic patients.
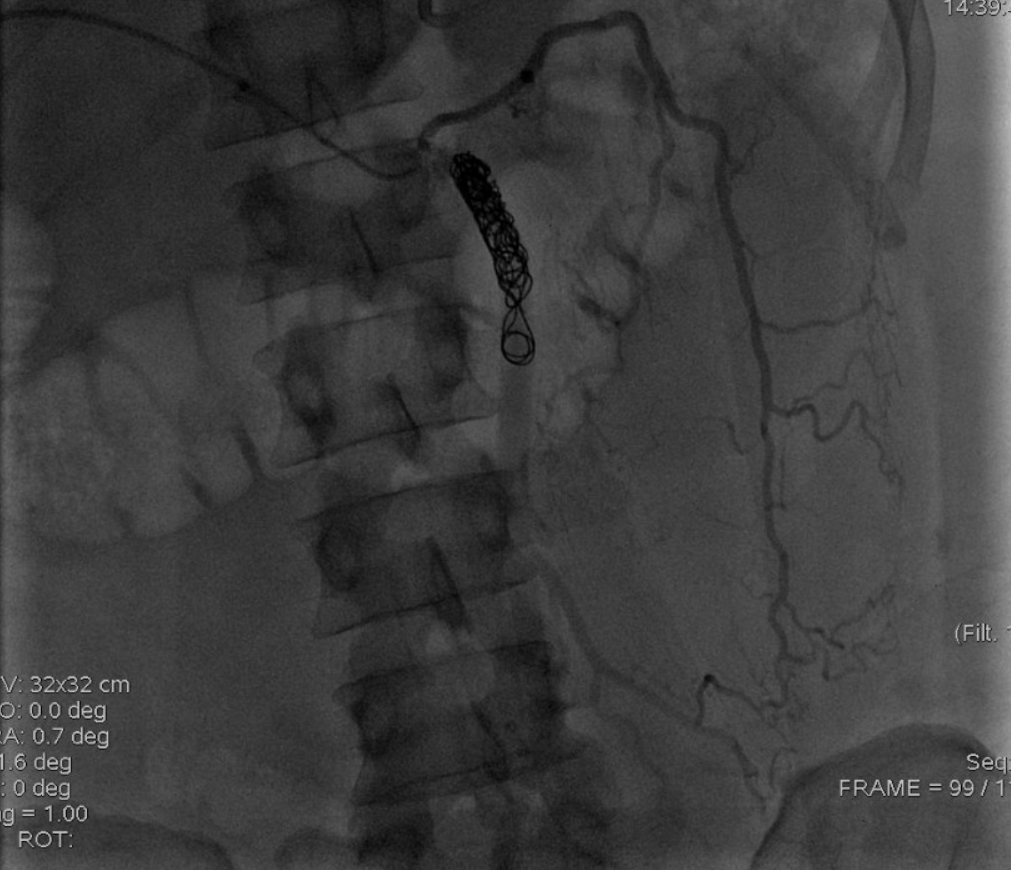
Figure: Portorectal shunt embolized
Disclosures:
Meghana Kakarla indicated no relevant financial relationships.
Dheeraja Kota indicated no relevant financial relationships.
Moin Din indicated no relevant financial relationships.
Giovannie Isaac-Coss indicated no relevant financial relationships.
Zain Alnoah indicated no relevant financial relationships.
Meghana Kakarla, MD1, Dheeraja Kota, MD2, Moin U. Din, MD2, Giovannie Isaac-Coss, MD3, Zain Alnoah, MD2. P1856 - Rectal Bypass to Disaster: A Rare SPSS Revealed on Repeat Imaging, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
