Sunday Poster Session
Category: Small Intestine
P1950 - Beyond the Gut: Nutcracker Syndrome as a Hidden Cause of Chronic Abdominal Pain in Surgically Altered Anatomy
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Zainab Rafaqat, MD
University of Oklahoma Health Sciences Center
Oklahoma City, OK
Presenting Author(s)
Zainab Rafaqat, MD1, Christopher Bouvette, MD2, Andrea Fernandez, MD1, Ijlal Akbar. Ali, MD3
1University of Oklahoma Health Sciences Center, Oklahoma City, OK; 2College of Medicine, University of Oklahoma Health Sciences Center, Oklahoma City, OK; 3University of Oklahoma, Oklahoma City, OK
Introduction: Nutcracker syndrome (NCS), defined by compression of the left renal vein between the superior mesenteric artery and the aorta, is a rare and underdiagnosed vascular disorder. While hematuria and flank pain are classic findings, gastrointestinal symptoms such as postprandial abdominal pain and nausea are underrecognized presentations that blur the line between vascular and visceral pathology. In patients with surgically altered GI anatomy, this overlap deepens diagnostic ambiguity, and anchoring bias may delay recognition. We present a diagnostically challenging case of NCS in a patient with complex post-surgical anatomy and longstanding unexplained abdominal pain.
Case Description/
Methods: A 38-year-old woman with a history of partial gastrectomy (Billroth II), vagotomy, and multiple interventions for H. pylori-associated peptic ulcer disease presented with worsening postprandial abdominal pain, nausea, vomiting, and poor oral intake. Labs revealed leukocytosis (16.5), hemoglobin of 10.5 g/dL, and urinalysis with 3+ blood, 1+ protein, and >50 RBCs per high-power field. Creatinine was 0.47 mg/dL. CT imaging showed no acute bowel pathology but noted post-surgical changes and moderate constipation. Renal Doppler ultrasound and subsequent renal sonogram revealed compression of the left renal vein between the SMA and aorta, with an aortomesenteric distance of 0.82 cm and elevated peak velocity—findings consistent with anterior nutcracker syndrome. The patient was referred to vascular surgery for venography and further management.
Discussion: This case highlights the diagnostic challenges of chronic abdominal pain in patients with altered GI anatomy, where symptoms often overlap and mislead. Nutcracker syndrome, though rare, should be considered when standard GI evaluations are inconclusive, especially with hematuria and supportive imaging. Recognizing vascular compression syndromes can prevent prolonged misdiagnosis and unnecessary procedures. A broadened differential and multidisciplinary approach are essential for complex cases of unexplained abdominal pain.

Figure: Axial View: CT shows compression of the left renal vein between the superior mesenteric artery and the aorta
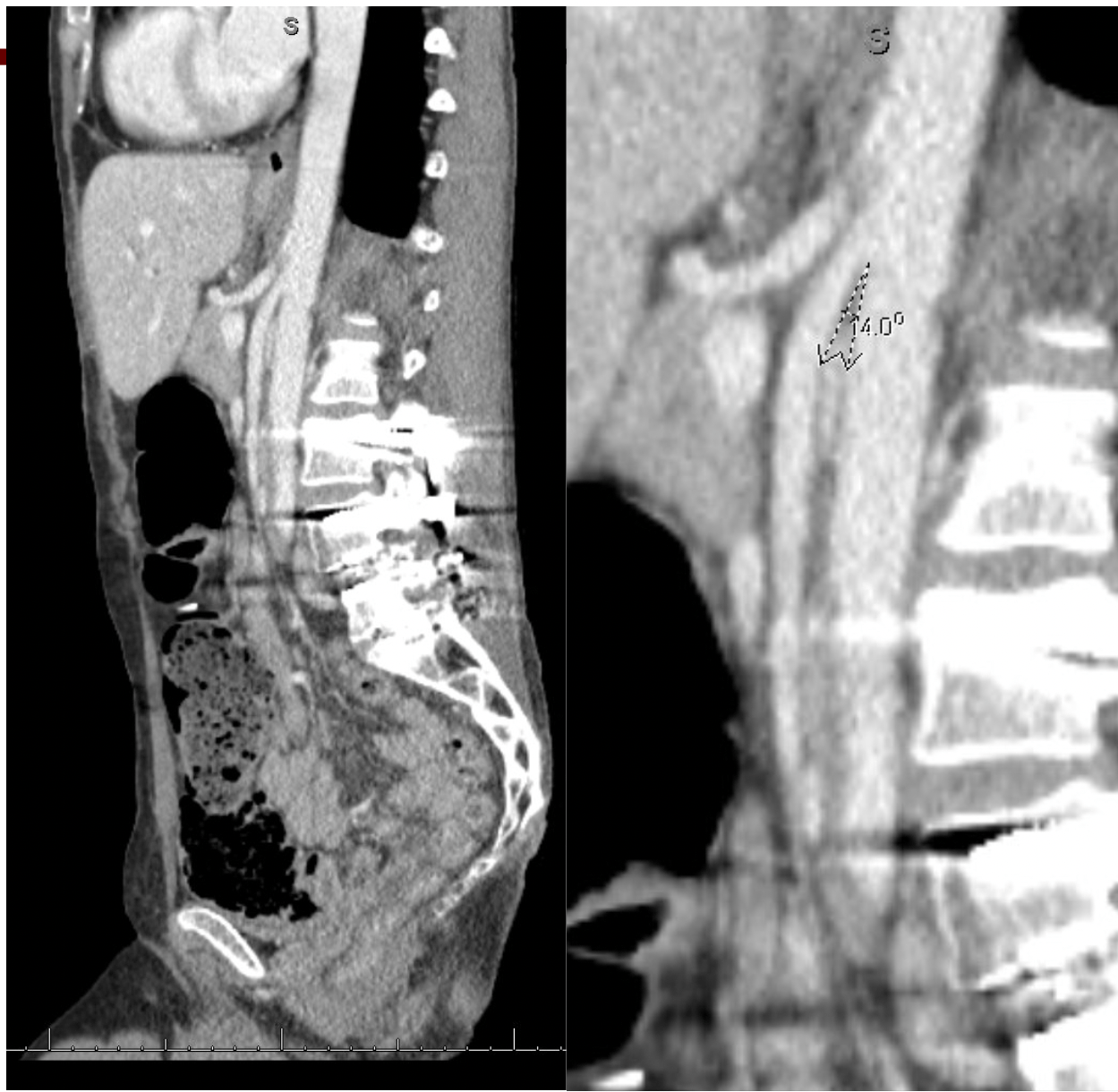
Figure: Sagittal View: CT demonstrates a reduced aortomesenteric angle of <40°, a key diagnostic feature of Nutcracker Syndrome
Disclosures:
Zainab Rafaqat indicated no relevant financial relationships.
Christopher Bouvette indicated no relevant financial relationships.
Andrea Fernandez indicated no relevant financial relationships.
Ijlal Ali indicated no relevant financial relationships.
Zainab Rafaqat, MD1, Christopher Bouvette, MD2, Andrea Fernandez, MD1, Ijlal Akbar. Ali, MD3. P1950 - Beyond the Gut: Nutcracker Syndrome as a Hidden Cause of Chronic Abdominal Pain in Surgically Altered Anatomy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Oklahoma Health Sciences Center, Oklahoma City, OK; 2College of Medicine, University of Oklahoma Health Sciences Center, Oklahoma City, OK; 3University of Oklahoma, Oklahoma City, OK
Introduction: Nutcracker syndrome (NCS), defined by compression of the left renal vein between the superior mesenteric artery and the aorta, is a rare and underdiagnosed vascular disorder. While hematuria and flank pain are classic findings, gastrointestinal symptoms such as postprandial abdominal pain and nausea are underrecognized presentations that blur the line between vascular and visceral pathology. In patients with surgically altered GI anatomy, this overlap deepens diagnostic ambiguity, and anchoring bias may delay recognition. We present a diagnostically challenging case of NCS in a patient with complex post-surgical anatomy and longstanding unexplained abdominal pain.
Case Description/
Methods: A 38-year-old woman with a history of partial gastrectomy (Billroth II), vagotomy, and multiple interventions for H. pylori-associated peptic ulcer disease presented with worsening postprandial abdominal pain, nausea, vomiting, and poor oral intake. Labs revealed leukocytosis (16.5), hemoglobin of 10.5 g/dL, and urinalysis with 3+ blood, 1+ protein, and >50 RBCs per high-power field. Creatinine was 0.47 mg/dL. CT imaging showed no acute bowel pathology but noted post-surgical changes and moderate constipation. Renal Doppler ultrasound and subsequent renal sonogram revealed compression of the left renal vein between the SMA and aorta, with an aortomesenteric distance of 0.82 cm and elevated peak velocity—findings consistent with anterior nutcracker syndrome. The patient was referred to vascular surgery for venography and further management.
Discussion: This case highlights the diagnostic challenges of chronic abdominal pain in patients with altered GI anatomy, where symptoms often overlap and mislead. Nutcracker syndrome, though rare, should be considered when standard GI evaluations are inconclusive, especially with hematuria and supportive imaging. Recognizing vascular compression syndromes can prevent prolonged misdiagnosis and unnecessary procedures. A broadened differential and multidisciplinary approach are essential for complex cases of unexplained abdominal pain.

Figure: Axial View: CT shows compression of the left renal vein between the superior mesenteric artery and the aorta
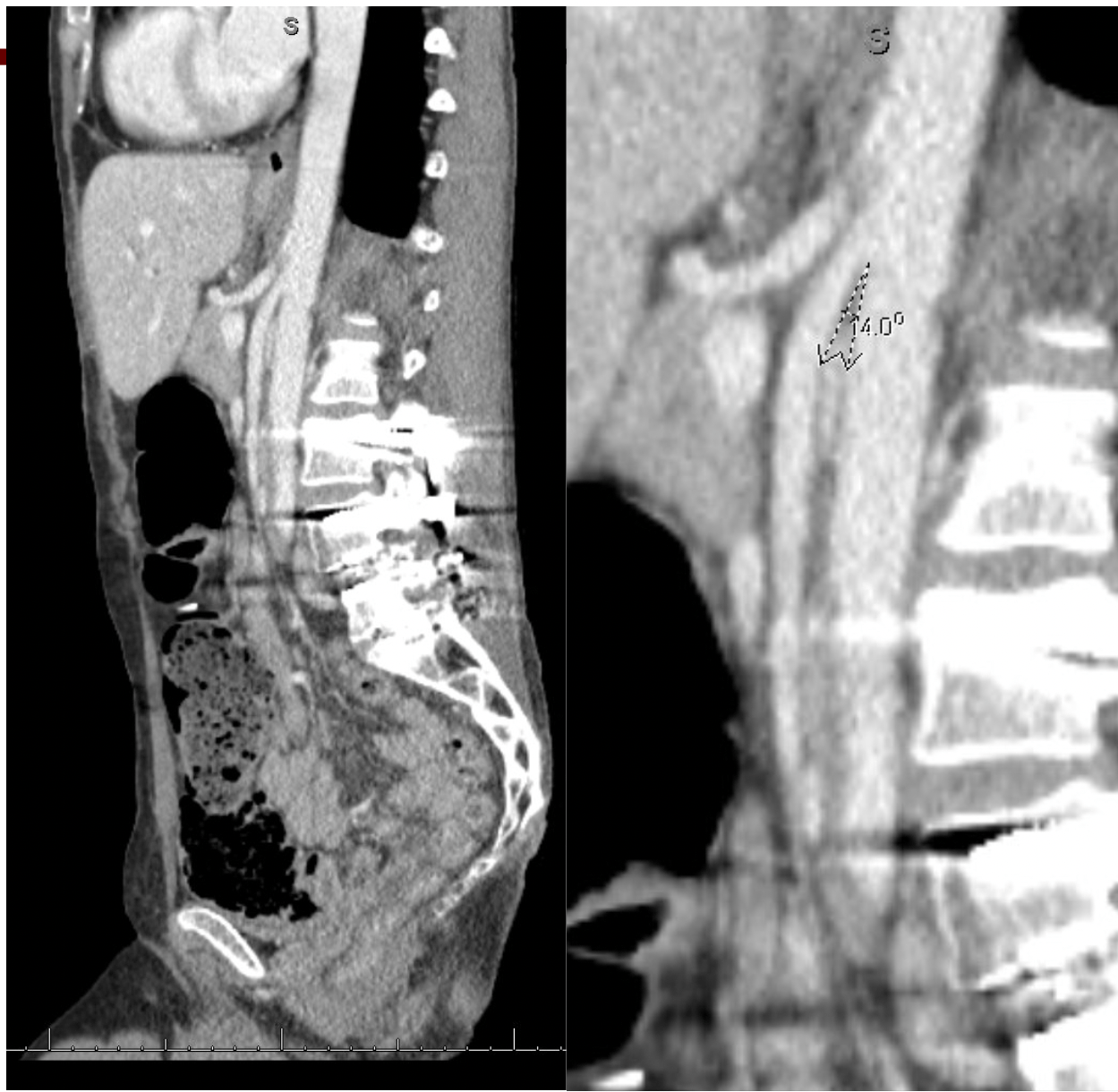
Figure: Sagittal View: CT demonstrates a reduced aortomesenteric angle of <40°, a key diagnostic feature of Nutcracker Syndrome
Disclosures:
Zainab Rafaqat indicated no relevant financial relationships.
Christopher Bouvette indicated no relevant financial relationships.
Andrea Fernandez indicated no relevant financial relationships.
Ijlal Ali indicated no relevant financial relationships.
Zainab Rafaqat, MD1, Christopher Bouvette, MD2, Andrea Fernandez, MD1, Ijlal Akbar. Ali, MD3. P1950 - Beyond the Gut: Nutcracker Syndrome as a Hidden Cause of Chronic Abdominal Pain in Surgically Altered Anatomy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
