Sunday Poster Session
Category: Small Intestine
P1948 - Duodenal Necrosis in Critical Illness: A Rare Endoscopic Finding With High Stakes Implications
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
Abel Sanchez, MD, MSc (he/him/his)
Hospital Roosevelt / Gastri-k
Guatemala City, San Marcos, Guatemala
Presenting Author(s)
Jorge Pacheco, 1, Ninoska Meléndez, 1, Abel Sanchez, MD, MSc2
11. Gastroenterology and Endoscopy Unit, Hospital Roosevelt Guatemala, Guatemala City, Quetzaltenango, Guatemala; 2Hospital Roosevelt / Gastri-k, Guatemala City, San Marcos, Guatemala
Introduction: Duodenal necrosis is a rare and life-threatening gastrointestinal complication, primarily linked to hypoperfusion, vasopressor use, and multi-organ dysfunction. Despite its infrequent documentation, its recognition during endoscopic evaluation is crucial to prevent catastrophic complications such as perforation or sepsis. This case highlights the diagnostic and therapeutic challenges posed by duodenal necrosis in critically ill patients, reinforcing the necessity of multidisciplinary strategies for optimizing outcomes
Case Description/
Methods: A 65-year-old female with hypertension, type 2 diabetes, and stage IV chronic kidney disease was referred to gastroenterology following recurrent cardiorespiratory arrests and two episodes of melena. The patient remained under mechanical ventilation and vasopressor support due to hemodynamic instability. Laboratory findings revealed anemia (Hb 8.1 g/dL), elevated creatinine (3.56 mg/dL), hypoalbuminemia (2.79 g/dL), and leukocytosis (GB 14.5 x 10³/µL), indicating systemic inflammation and metabolic distress.
An esophagogastroduodenoscopy (EGD) was performed to assess gastrointestinal bleeding. The procedure revealed extensive duodenal necrosis with mucosal sloughing and ischemic changes. Fig 1. Although no active bleeding was present, the necrotic tissue raised concerns for impending perforation and clinical deterioration. Immediate multidisciplinary consultation was initiated to determine the optimal management approach.
Discussion: Endoscopic detection of duodenal necrosis in critically ill patients presents a severe diagnostic and therapeutic challenge. This condition often results from profound circulatory compromise due to shock states, vasopressor use, and systemic vascular dysfunction. Given the few cases reported, clinical guidelines for management remain limited, necessitating a highly individualized approach
While conservative strategies such as hemodynamic stabilization, enteral support, and infection control may be appropriate in select cases, patients exhibiting progressive necrosis or peritoneal signs require early surgical consideration. The lack of standardized protocols highlights an urgent need for expanded research into duodenal ischemia and its critical care implications
This case underscores the importance of proactive endoscopic evaluation and a multidisciplinary strategy to optimize patient outcomes in this rare but severe condition
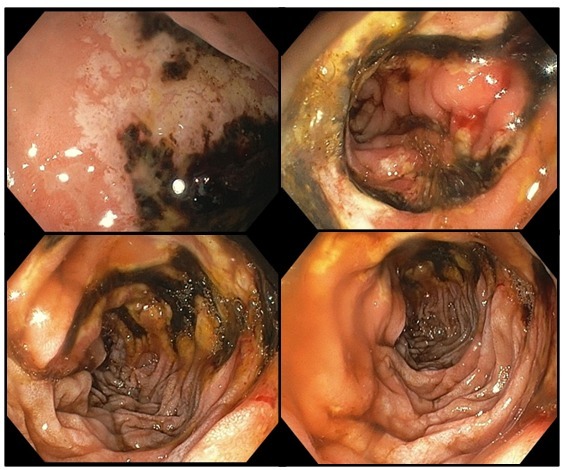
Figure: Figure 1. Loss of normal duodenal folds with black discoloration of the duodenal mucosa, indicating extensive necrosis, associated with friable, ulcerated mucosa with sloughing of necrotic tissue, and sharp demarcation between necrotic and viable tissue
Disclosures:
Jorge Pacheco indicated no relevant financial relationships.
Ninoska Meléndez indicated no relevant financial relationships.
Abel Sanchez indicated no relevant financial relationships.
Jorge Pacheco, 1, Ninoska Meléndez, 1, Abel Sanchez, MD, MSc2. P1948 - Duodenal Necrosis in Critical Illness: A Rare Endoscopic Finding With High Stakes Implications, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
11. Gastroenterology and Endoscopy Unit, Hospital Roosevelt Guatemala, Guatemala City, Quetzaltenango, Guatemala; 2Hospital Roosevelt / Gastri-k, Guatemala City, San Marcos, Guatemala
Introduction: Duodenal necrosis is a rare and life-threatening gastrointestinal complication, primarily linked to hypoperfusion, vasopressor use, and multi-organ dysfunction. Despite its infrequent documentation, its recognition during endoscopic evaluation is crucial to prevent catastrophic complications such as perforation or sepsis. This case highlights the diagnostic and therapeutic challenges posed by duodenal necrosis in critically ill patients, reinforcing the necessity of multidisciplinary strategies for optimizing outcomes
Case Description/
Methods: A 65-year-old female with hypertension, type 2 diabetes, and stage IV chronic kidney disease was referred to gastroenterology following recurrent cardiorespiratory arrests and two episodes of melena. The patient remained under mechanical ventilation and vasopressor support due to hemodynamic instability. Laboratory findings revealed anemia (Hb 8.1 g/dL), elevated creatinine (3.56 mg/dL), hypoalbuminemia (2.79 g/dL), and leukocytosis (GB 14.5 x 10³/µL), indicating systemic inflammation and metabolic distress.
An esophagogastroduodenoscopy (EGD) was performed to assess gastrointestinal bleeding. The procedure revealed extensive duodenal necrosis with mucosal sloughing and ischemic changes. Fig 1. Although no active bleeding was present, the necrotic tissue raised concerns for impending perforation and clinical deterioration. Immediate multidisciplinary consultation was initiated to determine the optimal management approach.
Discussion: Endoscopic detection of duodenal necrosis in critically ill patients presents a severe diagnostic and therapeutic challenge. This condition often results from profound circulatory compromise due to shock states, vasopressor use, and systemic vascular dysfunction. Given the few cases reported, clinical guidelines for management remain limited, necessitating a highly individualized approach
While conservative strategies such as hemodynamic stabilization, enteral support, and infection control may be appropriate in select cases, patients exhibiting progressive necrosis or peritoneal signs require early surgical consideration. The lack of standardized protocols highlights an urgent need for expanded research into duodenal ischemia and its critical care implications
This case underscores the importance of proactive endoscopic evaluation and a multidisciplinary strategy to optimize patient outcomes in this rare but severe condition
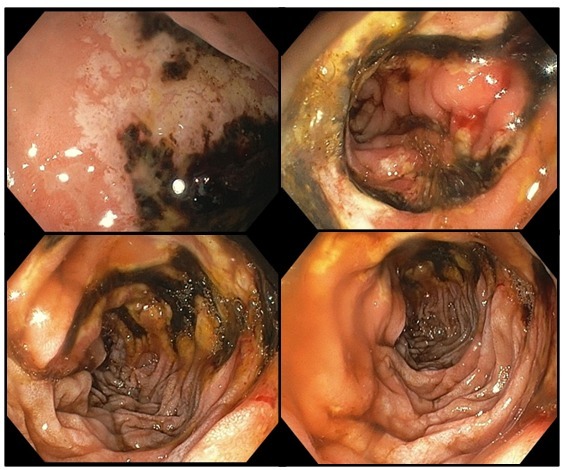
Figure: Figure 1. Loss of normal duodenal folds with black discoloration of the duodenal mucosa, indicating extensive necrosis, associated with friable, ulcerated mucosa with sloughing of necrotic tissue, and sharp demarcation between necrotic and viable tissue
Disclosures:
Jorge Pacheco indicated no relevant financial relationships.
Ninoska Meléndez indicated no relevant financial relationships.
Abel Sanchez indicated no relevant financial relationships.
Jorge Pacheco, 1, Ninoska Meléndez, 1, Abel Sanchez, MD, MSc2. P1948 - Duodenal Necrosis in Critical Illness: A Rare Endoscopic Finding With High Stakes Implications, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
