Sunday Poster Session
Category: Stomach and Spleen
P2093 - Diffuse Adenoma-like Lesion of the Gastric Mucosa with Multifocal Low-grade Dysplasia in a Patient with Hyper-IgE (Job’s) Syndrome
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- LK
Lekhya Kollu, BA
Lewis Katz School of Medicine at Temple University
Philadelphia, PA
Presenting Author(s)
Lekhya Kollu, BA1, Paola Goins, PA-C2, Disha Sharma, MBBS, MD3, Alexandra Freeman, MD4, Theo Heller, MD3, Philip Okafor, MD, MPH, FACG2
1Lewis Katz School of Medicine at Temple University, Philadelphia, PA; 2Mayo Clinic, Jacksonville, FL; 3National Institutes of Health, Bethesda, MD; 4NIAID/NIH, Bethesda, MD
Introduction: Hyper-IgE syndrome (HIES), or Job’s syndrome, is a rare immunodeficiency (≈1/1,000,000) marked by elevated IgE levels, recurrent pulmonary infections, cutaneous Staphylococcal infections, and atopic dermatitis. Most cases are sporadic or linked to autosomal dominant STAT3 mutations. In autosomal dominant HIES, non-lymphoma malignancies are rare. We report a case of HIES complicated by gastric adenomas and fundic gland polyps with multi-focal dysplasia.
Case Description/
Methods: A 55-year-old woman with HIES (STAT3 mutation) complicated by recurrent pulmonary infections, bronchiectasis, HFpEF and GERD on chronic proton pump inhibitors presents with early satiety, nausea, vomiting, and bloating. Upper endoscopy revealed a normal esophagus and a medium-sized, infiltrative, non-circumferential, non-bleeding mass in the gastric fundus (Figure 1). Multiple 4-20 mm pedunculated and sessile polyps with stigmata of recent bleeding were found in the fundus, body, and prepyloric region. A 6 mm, Paris Is mucosal papule was noted in the gastric antrum. Biopsies indicated gastric oxyntic mucosa with low grade dysplasia (diffuse adenoma-like lesion) in the fundus and focal low-grade dysplasia in the gastric body fundic gland polyps. Gastric antral mucosa showed complete type intestinal metaplasia and low-grade dysplasia (adenoma-like).
MRI abdomen showed rugal fold thickening, multiple small polypoid presumed enhancing areas, and several mass-like areas in the stomach, the largest measuring 2.1 x 2.2 x 1.7 cm along the posterior lateral fundus (Figure 2). She was referred for endoscopic ultrasound to rule out gastric adenocarcinoma and proximal polyposis of the stomach, and to assess candidacy for endoscopic resection as her significant cardiopulmonary disease limited candidacy for gastrectomy.
Discussion: This is the first case of diffuse gastric adenoma-like lesions and fundic gland polyps with multifocal low-grade dysplasia in a patient with HIES. While chronic PPI use may explain the fundic gland polyps, the multifocal dysplasia and diffuse adenoma-like lesions have not been previously described. Reports of malignancies in HIES outside of lymphomas are limited, and their pathogenesis is not fully understood. In addition to oncogenic effects of STAT3 mutations, immunodeficiency may impair tumor surveillance or increase chronic tumorigenic infections. This case underscores the need for research on the prevalence of gastric malignancies in patients with HIES and utility of screening/diagnostic endoscopies.
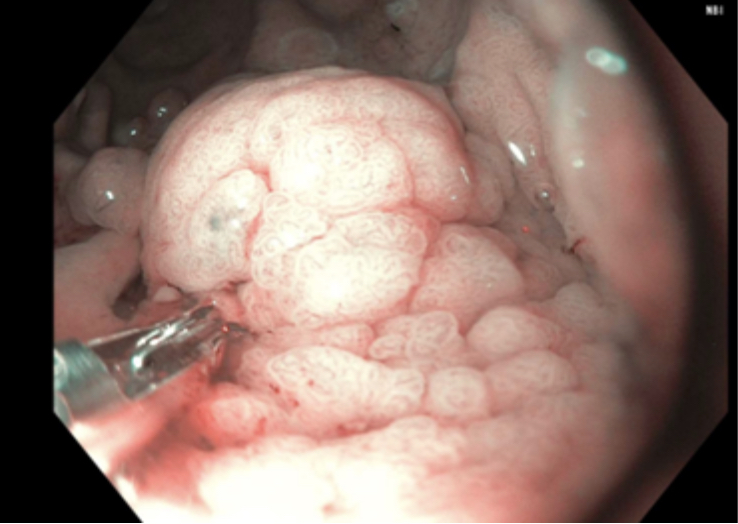
Figure: Figure 1: Diffuse adenoma-like lesion in gastric fundus
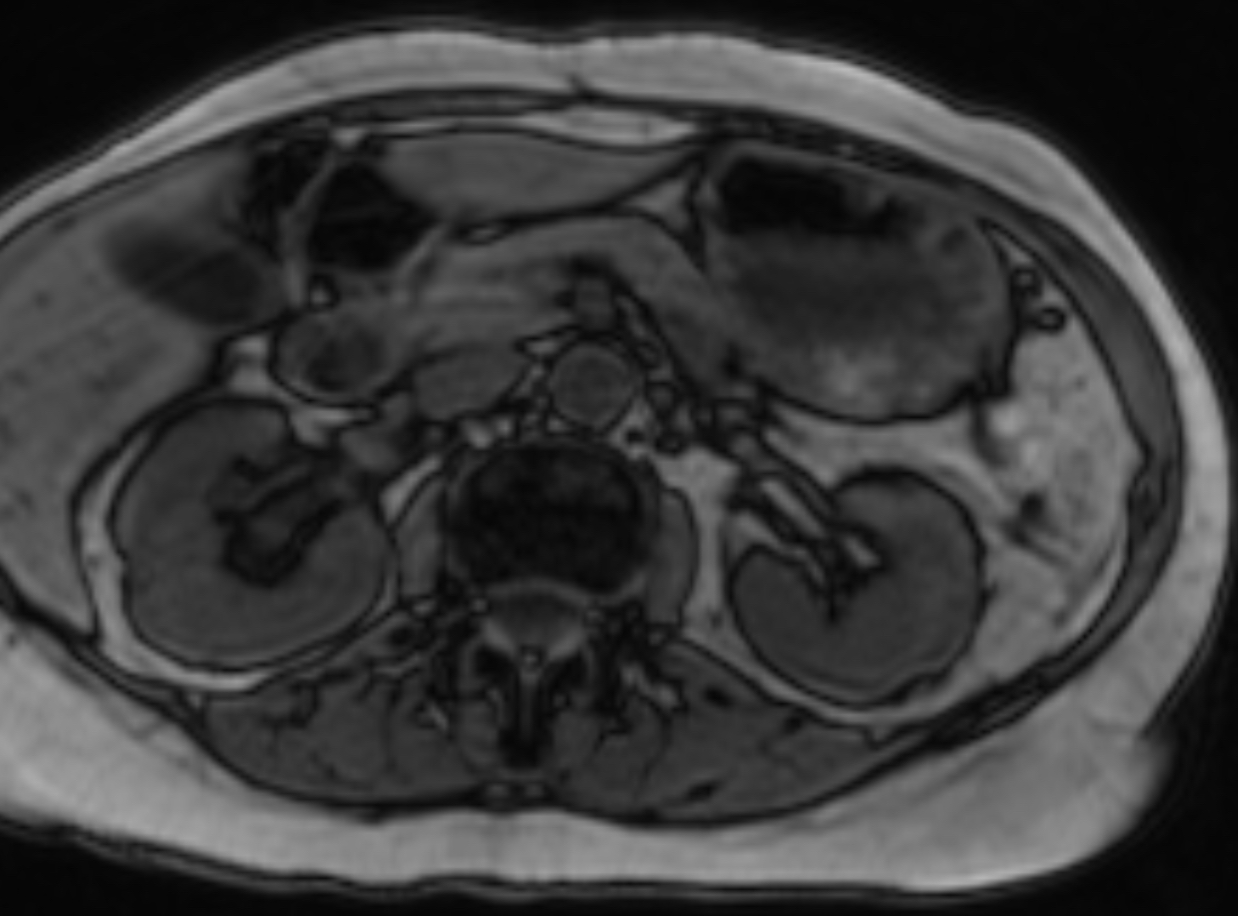
Figure: Figure 2: MRI abdomen showing rugal fold thickening
Disclosures:
Lekhya Kollu indicated no relevant financial relationships.
Paola Goins indicated no relevant financial relationships.
Disha Sharma indicated no relevant financial relationships.
Alexandra Freeman indicated no relevant financial relationships.
Theo Heller indicated no relevant financial relationships.
Philip Okafor indicated no relevant financial relationships.
Lekhya Kollu, BA1, Paola Goins, PA-C2, Disha Sharma, MBBS, MD3, Alexandra Freeman, MD4, Theo Heller, MD3, Philip Okafor, MD, MPH, FACG2. P2093 - Diffuse Adenoma-like Lesion of the Gastric Mucosa with Multifocal Low-grade Dysplasia in a Patient with Hyper-IgE (Job’s) Syndrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Lewis Katz School of Medicine at Temple University, Philadelphia, PA; 2Mayo Clinic, Jacksonville, FL; 3National Institutes of Health, Bethesda, MD; 4NIAID/NIH, Bethesda, MD
Introduction: Hyper-IgE syndrome (HIES), or Job’s syndrome, is a rare immunodeficiency (≈1/1,000,000) marked by elevated IgE levels, recurrent pulmonary infections, cutaneous Staphylococcal infections, and atopic dermatitis. Most cases are sporadic or linked to autosomal dominant STAT3 mutations. In autosomal dominant HIES, non-lymphoma malignancies are rare. We report a case of HIES complicated by gastric adenomas and fundic gland polyps with multi-focal dysplasia.
Case Description/
Methods: A 55-year-old woman with HIES (STAT3 mutation) complicated by recurrent pulmonary infections, bronchiectasis, HFpEF and GERD on chronic proton pump inhibitors presents with early satiety, nausea, vomiting, and bloating. Upper endoscopy revealed a normal esophagus and a medium-sized, infiltrative, non-circumferential, non-bleeding mass in the gastric fundus (Figure 1). Multiple 4-20 mm pedunculated and sessile polyps with stigmata of recent bleeding were found in the fundus, body, and prepyloric region. A 6 mm, Paris Is mucosal papule was noted in the gastric antrum. Biopsies indicated gastric oxyntic mucosa with low grade dysplasia (diffuse adenoma-like lesion) in the fundus and focal low-grade dysplasia in the gastric body fundic gland polyps. Gastric antral mucosa showed complete type intestinal metaplasia and low-grade dysplasia (adenoma-like).
MRI abdomen showed rugal fold thickening, multiple small polypoid presumed enhancing areas, and several mass-like areas in the stomach, the largest measuring 2.1 x 2.2 x 1.7 cm along the posterior lateral fundus (Figure 2). She was referred for endoscopic ultrasound to rule out gastric adenocarcinoma and proximal polyposis of the stomach, and to assess candidacy for endoscopic resection as her significant cardiopulmonary disease limited candidacy for gastrectomy.
Discussion: This is the first case of diffuse gastric adenoma-like lesions and fundic gland polyps with multifocal low-grade dysplasia in a patient with HIES. While chronic PPI use may explain the fundic gland polyps, the multifocal dysplasia and diffuse adenoma-like lesions have not been previously described. Reports of malignancies in HIES outside of lymphomas are limited, and their pathogenesis is not fully understood. In addition to oncogenic effects of STAT3 mutations, immunodeficiency may impair tumor surveillance or increase chronic tumorigenic infections. This case underscores the need for research on the prevalence of gastric malignancies in patients with HIES and utility of screening/diagnostic endoscopies.
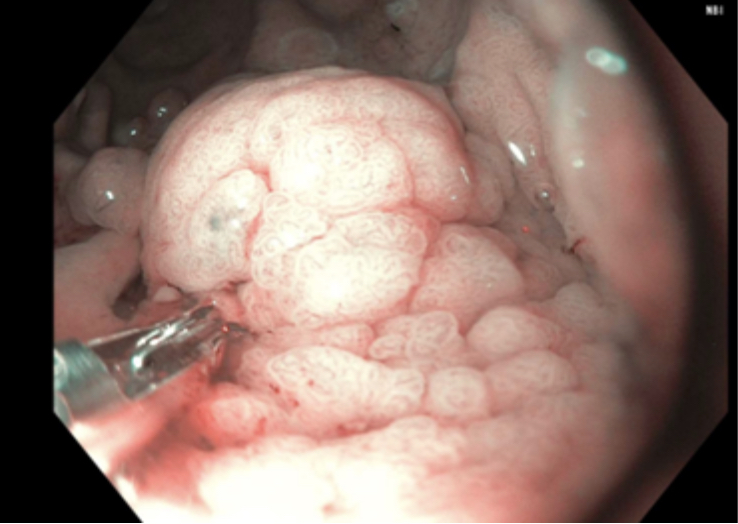
Figure: Figure 1: Diffuse adenoma-like lesion in gastric fundus
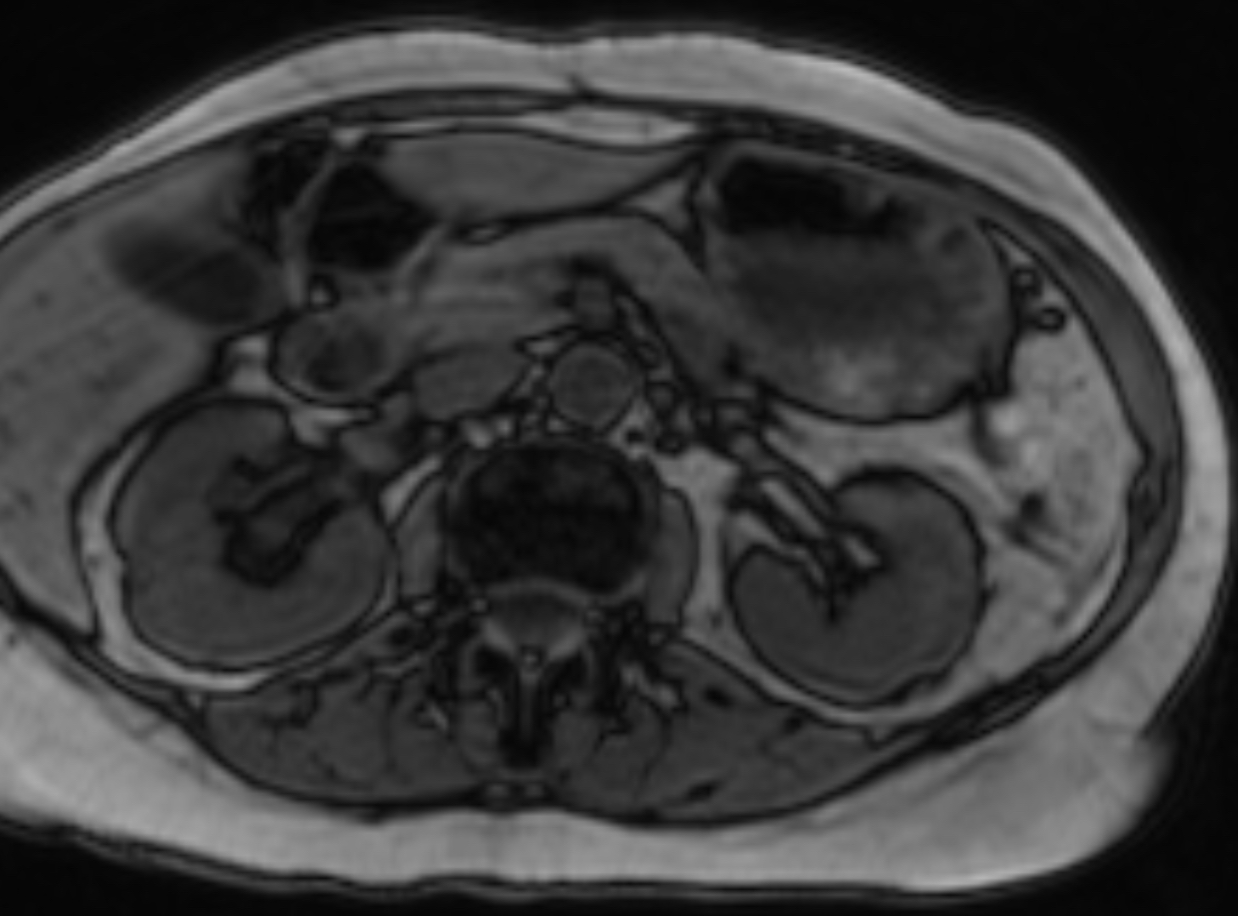
Figure: Figure 2: MRI abdomen showing rugal fold thickening
Disclosures:
Lekhya Kollu indicated no relevant financial relationships.
Paola Goins indicated no relevant financial relationships.
Disha Sharma indicated no relevant financial relationships.
Alexandra Freeman indicated no relevant financial relationships.
Theo Heller indicated no relevant financial relationships.
Philip Okafor indicated no relevant financial relationships.
Lekhya Kollu, BA1, Paola Goins, PA-C2, Disha Sharma, MBBS, MD3, Alexandra Freeman, MD4, Theo Heller, MD3, Philip Okafor, MD, MPH, FACG2. P2093 - Diffuse Adenoma-like Lesion of the Gastric Mucosa with Multifocal Low-grade Dysplasia in a Patient with Hyper-IgE (Job’s) Syndrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
