Sunday Poster Session
Category: Stomach and Spleen
P2087 - When Standard Diagnostics Fail: A Case of Gastric Linitis Plastica With Negative Work-Up
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- ZE
Zeyad Elharabi, MBBS, MS
Texas Tech University Health Sciences Center
Lubbock, TX
Presenting Author(s)
Zeyad Elharabi, MBBS, MS1, Akash Dev, MBA1, Krista Oliver-Jackson, BS2, Arman Vaghefi, BS3, Matthew Reyes, BS4, Houssam Kharrat, MD4
1Texas Tech University Health Sciences Center, Lubbock, TX; 2Caprock Gastro Research, LLC., Lubbock, TX; 3Rocky Vista University, Colorado Springs, CO; 4West Texas Digestive Disease Center, Lubbock, TX
Introduction: Gastric linitis plastica (GLP) is described as thickening of the gastric wall without notable ulceration. GLP can be particularly difficult to diagnose via endoscopy due to the submucosal infiltration of the malignancy. Here we present a case of GLP in a patient with a negative CT, EGD biopsy, and indeterminate upper GI series.
Case Description/
Methods: A 63-year-old male presented with a three-month history of epigastric pain with nocturnal awakening, dysphagia to solids, loss of appetite, acid reflux, and intermittent changes in stool consistency. His past medical history was significant for Parkinson’s disease. A CT scan of the abdomen and pelvis revealed only sigmoid diverticulosis and an inguinal hernia.
EGD identified a partially obstructing, infiltrative 44 mm gastric mass in the body of the stomach, with stigmata of recent bleeding. Initial biopsies showed reactive changes without malignancy, and initial laboratory tests, including CEA, were unremarkable.
Due to persistent symptoms, an upper GI series with a barium swallow was performed but yielded negative results. However, endoscopic ultrasound (EUS) revealed gastric wall thickening up to 22 mm, involving the luminal interface, superficial mucosa, and deep mucosa. Fine-needle aspiration (FNA) confirmed poorly differentiated adenocarcinoma with signet ring features. Follow-up pathology was negative for HER2, with CD117 and DOG1 also negative, ruling out gastrointestinal stromal tumor (GIST). PD-L1 testing was positive.
During surgical exploration, multiple peritoneal implants were discovered. Given the extent of the disease, the patient elected to initiate immunotherapy, which resulted in a poor response. Eventually, he was admitted to hospice care.
Discussion: Diagnosing gastric linitis plastica (GLP) can be particularly challenging, as the primary lesion often lies deep within the gastric wall. Up to 30% of initial cold forceps biopsies may yield false-negative results in GLP cases. In such situations, endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) is crucial for obtaining tissue samples from the submucosal and deeper layers. This case underscores the diagnostic difficulty of GLP, given its nonspecific symptoms—such as dysphagia, weight loss, and epigastric pain—and the often inconclusive findings on imaging, blood work, and initial biopsies.
While imaging studies are valuable tools in the diagnostic process, they should not replace careful clinical judgment
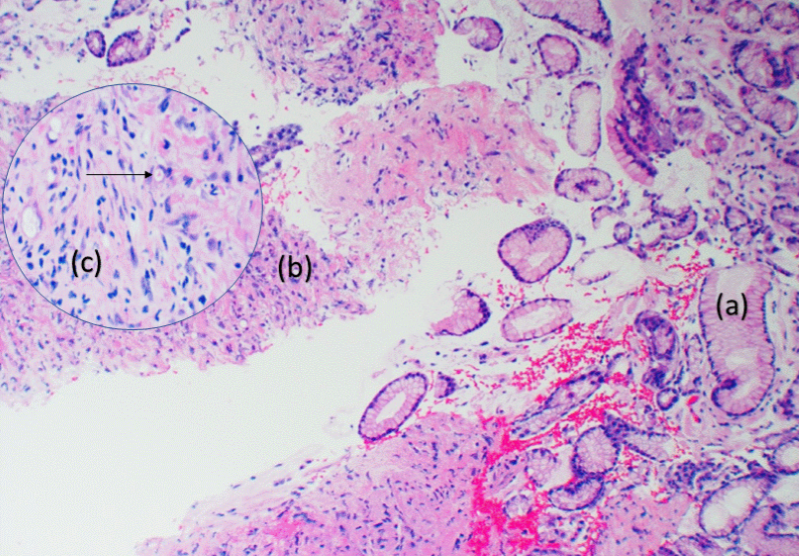
Figure: Cross-section pathology (a) hyperplastic polyp (b) tumor (c) 100x magnification of tumor tissue. Black arrow indicating signet-ring cells.

Figure: 1 Stomach wall thickening was observed, and no obvious mass was detected.
2 CT scan results normal.
3 Upper GI series provided poor visualization of a gastric mass.
4 Stomach wall thickening noted on EUS.
Disclosures:
Zeyad Elharabi indicated no relevant financial relationships.
Akash Dev indicated no relevant financial relationships.
Krista Oliver-Jackson indicated no relevant financial relationships.
Arman Vaghefi indicated no relevant financial relationships.
Matthew Reyes indicated no relevant financial relationships.
Houssam Kharrat indicated no relevant financial relationships.
Zeyad Elharabi, MBBS, MS1, Akash Dev, MBA1, Krista Oliver-Jackson, BS2, Arman Vaghefi, BS3, Matthew Reyes, BS4, Houssam Kharrat, MD4. P2087 - When Standard Diagnostics Fail: A Case of Gastric Linitis Plastica With Negative Work-Up, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Texas Tech University Health Sciences Center, Lubbock, TX; 2Caprock Gastro Research, LLC., Lubbock, TX; 3Rocky Vista University, Colorado Springs, CO; 4West Texas Digestive Disease Center, Lubbock, TX
Introduction: Gastric linitis plastica (GLP) is described as thickening of the gastric wall without notable ulceration. GLP can be particularly difficult to diagnose via endoscopy due to the submucosal infiltration of the malignancy. Here we present a case of GLP in a patient with a negative CT, EGD biopsy, and indeterminate upper GI series.
Case Description/
Methods: A 63-year-old male presented with a three-month history of epigastric pain with nocturnal awakening, dysphagia to solids, loss of appetite, acid reflux, and intermittent changes in stool consistency. His past medical history was significant for Parkinson’s disease. A CT scan of the abdomen and pelvis revealed only sigmoid diverticulosis and an inguinal hernia.
EGD identified a partially obstructing, infiltrative 44 mm gastric mass in the body of the stomach, with stigmata of recent bleeding. Initial biopsies showed reactive changes without malignancy, and initial laboratory tests, including CEA, were unremarkable.
Due to persistent symptoms, an upper GI series with a barium swallow was performed but yielded negative results. However, endoscopic ultrasound (EUS) revealed gastric wall thickening up to 22 mm, involving the luminal interface, superficial mucosa, and deep mucosa. Fine-needle aspiration (FNA) confirmed poorly differentiated adenocarcinoma with signet ring features. Follow-up pathology was negative for HER2, with CD117 and DOG1 also negative, ruling out gastrointestinal stromal tumor (GIST). PD-L1 testing was positive.
During surgical exploration, multiple peritoneal implants were discovered. Given the extent of the disease, the patient elected to initiate immunotherapy, which resulted in a poor response. Eventually, he was admitted to hospice care.
Discussion: Diagnosing gastric linitis plastica (GLP) can be particularly challenging, as the primary lesion often lies deep within the gastric wall. Up to 30% of initial cold forceps biopsies may yield false-negative results in GLP cases. In such situations, endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) is crucial for obtaining tissue samples from the submucosal and deeper layers. This case underscores the diagnostic difficulty of GLP, given its nonspecific symptoms—such as dysphagia, weight loss, and epigastric pain—and the often inconclusive findings on imaging, blood work, and initial biopsies.
While imaging studies are valuable tools in the diagnostic process, they should not replace careful clinical judgment
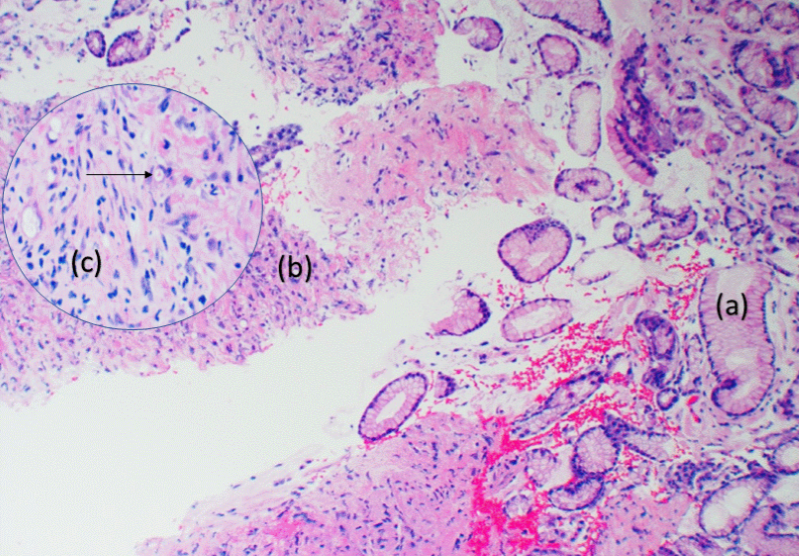
Figure: Cross-section pathology (a) hyperplastic polyp (b) tumor (c) 100x magnification of tumor tissue. Black arrow indicating signet-ring cells.

Figure: 1 Stomach wall thickening was observed, and no obvious mass was detected.
2 CT scan results normal.
3 Upper GI series provided poor visualization of a gastric mass.
4 Stomach wall thickening noted on EUS.
Disclosures:
Zeyad Elharabi indicated no relevant financial relationships.
Akash Dev indicated no relevant financial relationships.
Krista Oliver-Jackson indicated no relevant financial relationships.
Arman Vaghefi indicated no relevant financial relationships.
Matthew Reyes indicated no relevant financial relationships.
Houssam Kharrat indicated no relevant financial relationships.
Zeyad Elharabi, MBBS, MS1, Akash Dev, MBA1, Krista Oliver-Jackson, BS2, Arman Vaghefi, BS3, Matthew Reyes, BS4, Houssam Kharrat, MD4. P2087 - When Standard Diagnostics Fail: A Case of Gastric Linitis Plastica With Negative Work-Up, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
