Sunday Poster Session
Category: Stomach and Spleen
P2086 - Rare Presentation of Extrapulmonary Pneumocystis in the Lesser Curvature of the Stomach: A Case Report
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Erin Fannin, DO, MSPH
East Alabama Medical Center
Opelika, AL
Presenting Author(s)
Erin Fannin, DO, MSPH1, Stewart R. Malave, MD2, Nathan Douthit, MD3
1East Alabama Medical Center, Opelika, AL; 2East Alabama Medical Center, Auburn, AL; 3Edward Via College of Osteopathic Medicine, Opelika, AL
Introduction: Pneumocystis jirovecii pneumonia (PJP) is an opportunistic infection associated with HIV/AIDS. While lungs are the primary site of infection, extrapulmonary PJP can occur in approximately 3% of pneumocystis cases. Common sites of EPJP are liver, spleen, bone, skin, and lymph nodes. This case highlights a unique presentation of EPJP in the lesser curvature of the stomach.
Case Description/
Methods: A 47-year-old male with a past medical history of HIV/AIDS, alcohol and tobacco use, presented with complaints of greater than 20 lb. weight loss with daily postprandial epigastric pain for six months. Abdominal pain, mild dysphagia, nausea, vomiting, and reflux. He denied NSAID use or lower GI symptoms. Exam findings revealed diffuse epigastric tenderness. Three years ago, a large thick-walled cavitary lung mass was noted on CT. Bronchoscopy cultures were positive for candidiasis and BAL positive for Aspergillus antigen. CD4 count was 20 at that time. He reported compliance on Biktarvy. CD4 count was 8 at the initial GI appointment and endoscopy was scheduled.
Initial EGD noted candidiasis throughout the esophagus and a large, ulcerated mass on the lesser curvature of the stomach with deep ulceration and raised edges. Biopsy showed benign gastric mucosa with ulcer formation, acute and chronic inflammation, and necrosis. GMS stains demonstrated fungal yeast and hyphae.
Repeat EGD again noted an ulcerated mass and diffuse candidiasis. Biopsy revealed gastric adenoma, foveolar type, prompting partial gastrectomy. Pathology reported a benign stomach with multifocal abscess and focal necrotizing granuloma formation throughout all levels of the wall, consistent with EPJP infection. GMS stain showed uniform yeast-like cystic structures consistent with PJP. Special stains were positive for the following: CD68, H. pylori, Ki-67, and Pneumocystis immunoperoxidase. The patient left AMA prior to ID evaluation.
Discussion: Involvement of the GI tract with PJP is rare. Risk factors include a CD4 count < 50 often in the setting of ART-naive or advanced HIV/AIDS progression. Prior pulmonary infection, seen in this case, may serve as a source for hematogenous spread to extrapulmonary sites.
Clinical presentation is variable. Definitive diagnosis is made by GMS and immunofluorescence stains. TMP-SMX is the first-line therapy for EPJP. This patient received TMP-SMX IV treatment prior to discharge but did not complete the recommended 21-day course. Early recognition and treatment are essential to improve overall outcome.
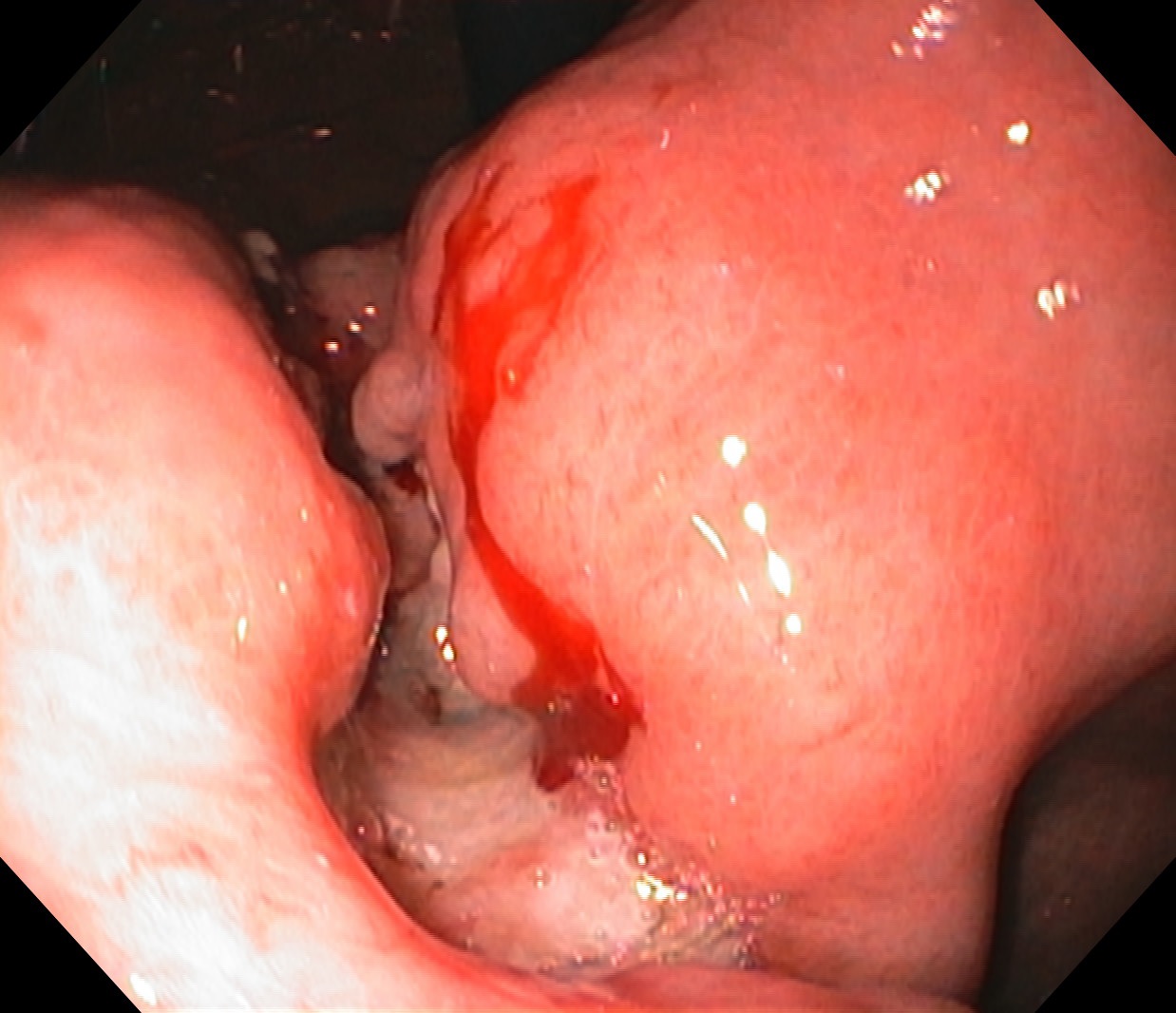
Figure: Figure 1: Ulcerated mass, measuring 4.8 cm x 4.3 cm, on initial EGD.
Disclosures:
Erin Fannin indicated no relevant financial relationships.
Stewart Malave indicated no relevant financial relationships.
Nathan Douthit indicated no relevant financial relationships.
Erin Fannin, DO, MSPH1, Stewart R. Malave, MD2, Nathan Douthit, MD3. P2086 - Rare Presentation of Extrapulmonary Pneumocystis in the Lesser Curvature of the Stomach: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1East Alabama Medical Center, Opelika, AL; 2East Alabama Medical Center, Auburn, AL; 3Edward Via College of Osteopathic Medicine, Opelika, AL
Introduction: Pneumocystis jirovecii pneumonia (PJP) is an opportunistic infection associated with HIV/AIDS. While lungs are the primary site of infection, extrapulmonary PJP can occur in approximately 3% of pneumocystis cases. Common sites of EPJP are liver, spleen, bone, skin, and lymph nodes. This case highlights a unique presentation of EPJP in the lesser curvature of the stomach.
Case Description/
Methods: A 47-year-old male with a past medical history of HIV/AIDS, alcohol and tobacco use, presented with complaints of greater than 20 lb. weight loss with daily postprandial epigastric pain for six months. Abdominal pain, mild dysphagia, nausea, vomiting, and reflux. He denied NSAID use or lower GI symptoms. Exam findings revealed diffuse epigastric tenderness. Three years ago, a large thick-walled cavitary lung mass was noted on CT. Bronchoscopy cultures were positive for candidiasis and BAL positive for Aspergillus antigen. CD4 count was 20 at that time. He reported compliance on Biktarvy. CD4 count was 8 at the initial GI appointment and endoscopy was scheduled.
Initial EGD noted candidiasis throughout the esophagus and a large, ulcerated mass on the lesser curvature of the stomach with deep ulceration and raised edges. Biopsy showed benign gastric mucosa with ulcer formation, acute and chronic inflammation, and necrosis. GMS stains demonstrated fungal yeast and hyphae.
Repeat EGD again noted an ulcerated mass and diffuse candidiasis. Biopsy revealed gastric adenoma, foveolar type, prompting partial gastrectomy. Pathology reported a benign stomach with multifocal abscess and focal necrotizing granuloma formation throughout all levels of the wall, consistent with EPJP infection. GMS stain showed uniform yeast-like cystic structures consistent with PJP. Special stains were positive for the following: CD68, H. pylori, Ki-67, and Pneumocystis immunoperoxidase. The patient left AMA prior to ID evaluation.
Discussion: Involvement of the GI tract with PJP is rare. Risk factors include a CD4 count < 50 often in the setting of ART-naive or advanced HIV/AIDS progression. Prior pulmonary infection, seen in this case, may serve as a source for hematogenous spread to extrapulmonary sites.
Clinical presentation is variable. Definitive diagnosis is made by GMS and immunofluorescence stains. TMP-SMX is the first-line therapy for EPJP. This patient received TMP-SMX IV treatment prior to discharge but did not complete the recommended 21-day course. Early recognition and treatment are essential to improve overall outcome.
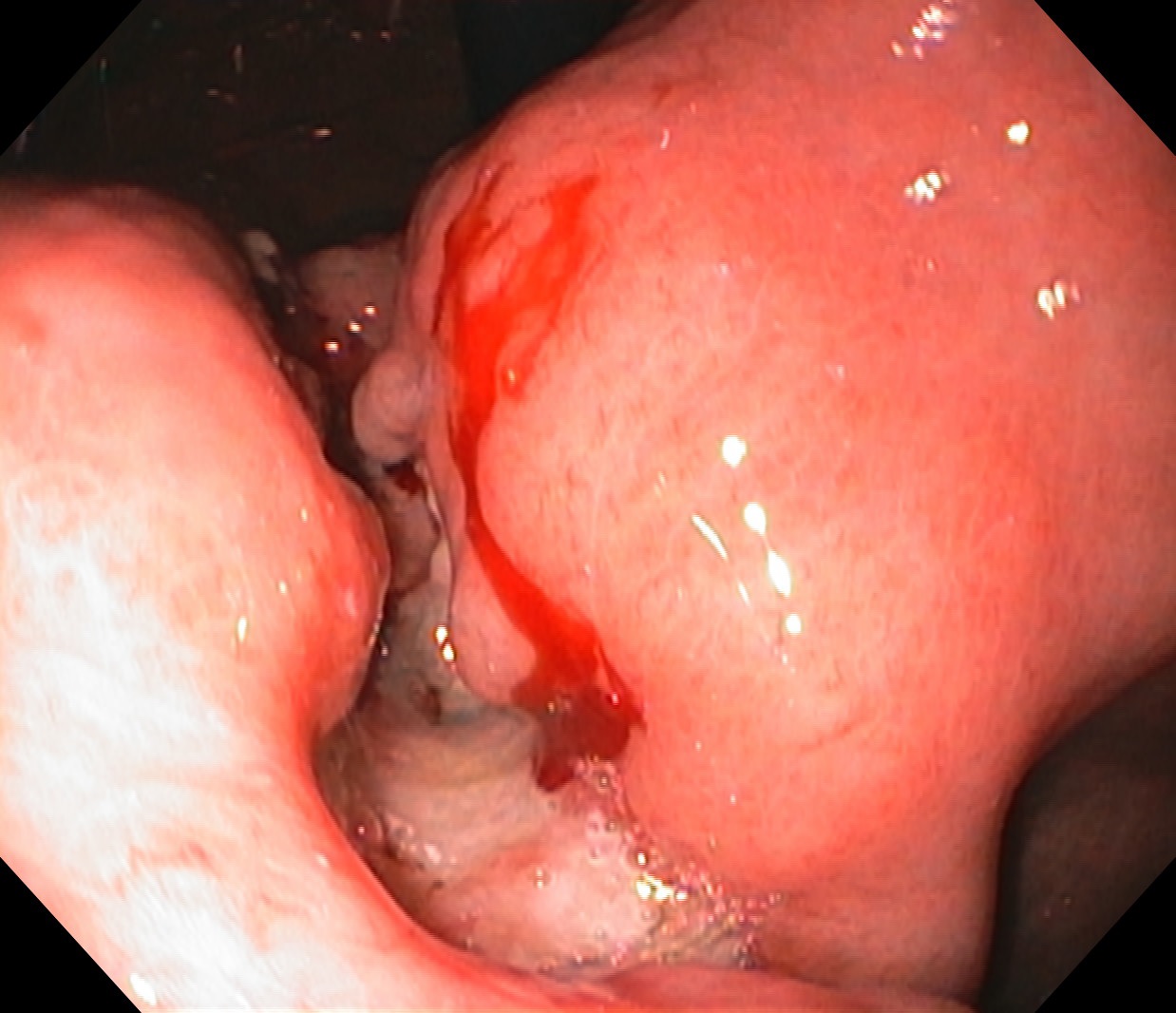
Figure: Figure 1: Ulcerated mass, measuring 4.8 cm x 4.3 cm, on initial EGD.
Disclosures:
Erin Fannin indicated no relevant financial relationships.
Stewart Malave indicated no relevant financial relationships.
Nathan Douthit indicated no relevant financial relationships.
Erin Fannin, DO, MSPH1, Stewart R. Malave, MD2, Nathan Douthit, MD3. P2086 - Rare Presentation of Extrapulmonary Pneumocystis in the Lesser Curvature of the Stomach: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
