Sunday Poster Session
Category: Stomach and Spleen
P2084 - Endoscopic Closure of Gastric Leak and Wound Dehiscence After Biliopancreatic Diversion With Duodenal Switch
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Ronan Allencherril, MD
Houston Methodist Hospital
Houston, TX
Presenting Author(s)
Ronan Allencherril, MD, Thomas R. McCarty, MD, MPH
Houston Methodist Hospital, Houston, TX
Introduction: Multiple options for endoscopic closure of mucosal defects, leaks, and fistulae exist, including clips and suturing devices. Selection of the appropriate device depends on several factors including size of the defect and the condition of the surrounding mucosa. Here we present a unique case of successful closure of a complete wound dehiscence after biliopancreatic diversion with duodenal switch using a combined endoscopic approach.
Case Description/
Methods: A 41-year-old woman with a history of class III obesity underwent Roux-en-Y conversion to biliopancreatic diversion with duodenal switch for weight regain. Her post-op course was complicated immediate post-surgical leak with large intraabdominal fluid collection. She was immediately taken back to the operating room by the surgical team and found to have a perforation along the staple line with placement of a 10 cm fully-covered metal stent and drain placement. Over the following months, the stent was exchanged multiple times, and she underwent placement of a jejunal feeding tube and JP drain; however, the leak persisted. She was then referred to gastroenterology for possible endoscopic closure. Esophagogastroduodenoscopy (EGD) revealed complete dehiscence of the staple line and retained suture material with JP drain visualization within the gastric lumen (Figure 1). Argon plasma coagulation of the fistula site was performed to de-epithelialize the tract. Next, the distal full-thickness defect was closed with a full-thickness endoscopic suturing device. Given severe friability and difficult positioning in the proximal stomach, the decision was made to use an endoscopic helical tack-based system to close the remaining proximal gastric defect (Figure 2B). Fluoroscopy showed no contrast extravasation immediately post-closure with marked decrease in peritoneal drain output over the next 2 weeks. Two months after endoscopic closure, repeat EGD showed complete closure of prior wound dehiscence with minimal ulceration along the staple line – confirming successful endoscopic closure (Figure 2C). Fluoroscopy again showed resolution of the prior gastric leak. She tolerated oral intake and the J tube was removed.
Discussion: This case highlights a challenging case of an endoscopic closure of a complete surgical dehiscence using both a full-thickness suturing device and a helical tack-based suturing system. Selection of an appropriate modality in such cases can be difficult, and the use of multiple devices is sometimes necessary.
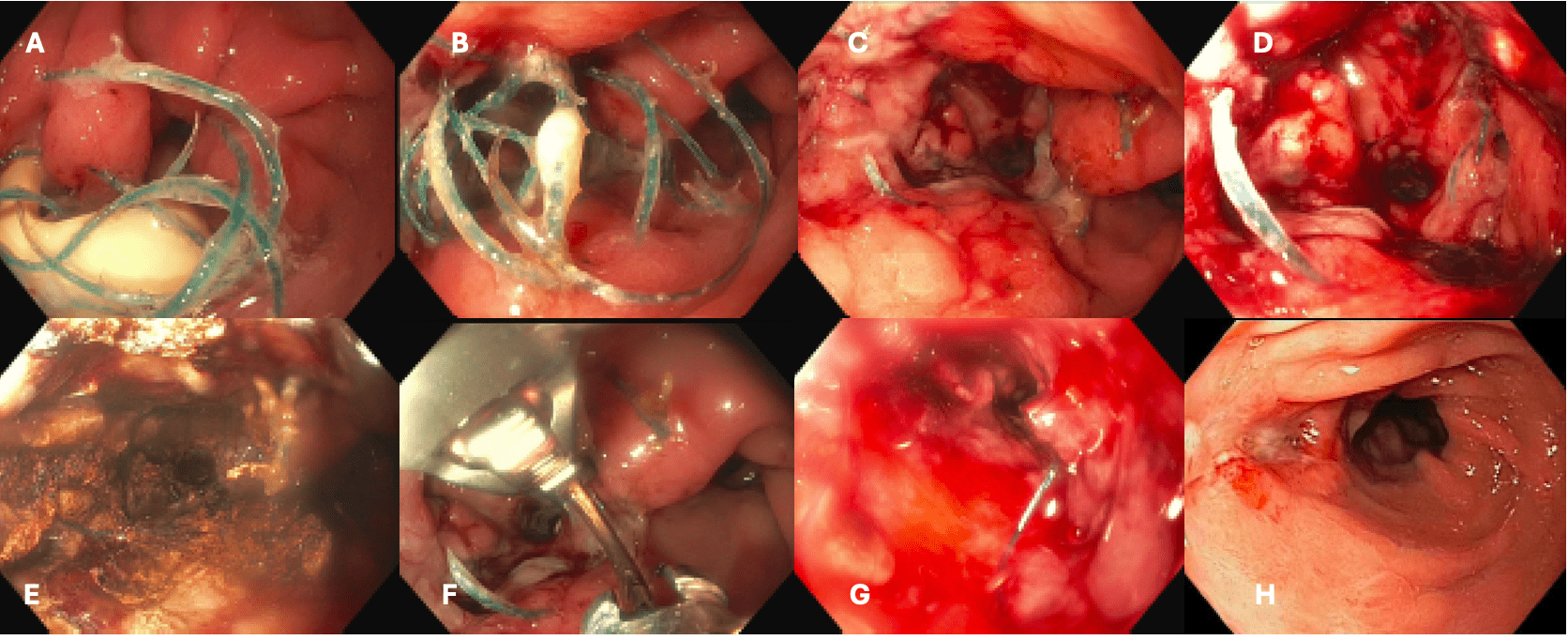
Figure: Figure 1. Endoscopic evaluation showing complete dehiscence after biliopancreatic diversion with duodenal switch. (A,B) Retained suture from prior surgical closure and intraluminal drain. (C,D) Staple line after external drain withdrawal into peritoneal space and endoscopic suture removal. (E) Argon plasma coagulation to staple line/defect to de-epithelialize the tract. (F,G) Endoscopic closure using a full-thickness endoscopic suturing device and helical tack-based endoscopic device. (H) Successful closure at 2 month-follow up demonstrating resolved dehiscence.
Disclosures:
Ronan Allencherril indicated no relevant financial relationships.
Thomas McCarty: Covidien/Medtronic – Consultant. Endoquest Robotics – Consultant.
Ronan Allencherril, MD, Thomas R. McCarty, MD, MPH. P2084 - Endoscopic Closure of Gastric Leak and Wound Dehiscence After Biliopancreatic Diversion With Duodenal Switch, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Houston Methodist Hospital, Houston, TX
Introduction: Multiple options for endoscopic closure of mucosal defects, leaks, and fistulae exist, including clips and suturing devices. Selection of the appropriate device depends on several factors including size of the defect and the condition of the surrounding mucosa. Here we present a unique case of successful closure of a complete wound dehiscence after biliopancreatic diversion with duodenal switch using a combined endoscopic approach.
Case Description/
Methods: A 41-year-old woman with a history of class III obesity underwent Roux-en-Y conversion to biliopancreatic diversion with duodenal switch for weight regain. Her post-op course was complicated immediate post-surgical leak with large intraabdominal fluid collection. She was immediately taken back to the operating room by the surgical team and found to have a perforation along the staple line with placement of a 10 cm fully-covered metal stent and drain placement. Over the following months, the stent was exchanged multiple times, and she underwent placement of a jejunal feeding tube and JP drain; however, the leak persisted. She was then referred to gastroenterology for possible endoscopic closure. Esophagogastroduodenoscopy (EGD) revealed complete dehiscence of the staple line and retained suture material with JP drain visualization within the gastric lumen (Figure 1). Argon plasma coagulation of the fistula site was performed to de-epithelialize the tract. Next, the distal full-thickness defect was closed with a full-thickness endoscopic suturing device. Given severe friability and difficult positioning in the proximal stomach, the decision was made to use an endoscopic helical tack-based system to close the remaining proximal gastric defect (Figure 2B). Fluoroscopy showed no contrast extravasation immediately post-closure with marked decrease in peritoneal drain output over the next 2 weeks. Two months after endoscopic closure, repeat EGD showed complete closure of prior wound dehiscence with minimal ulceration along the staple line – confirming successful endoscopic closure (Figure 2C). Fluoroscopy again showed resolution of the prior gastric leak. She tolerated oral intake and the J tube was removed.
Discussion: This case highlights a challenging case of an endoscopic closure of a complete surgical dehiscence using both a full-thickness suturing device and a helical tack-based suturing system. Selection of an appropriate modality in such cases can be difficult, and the use of multiple devices is sometimes necessary.
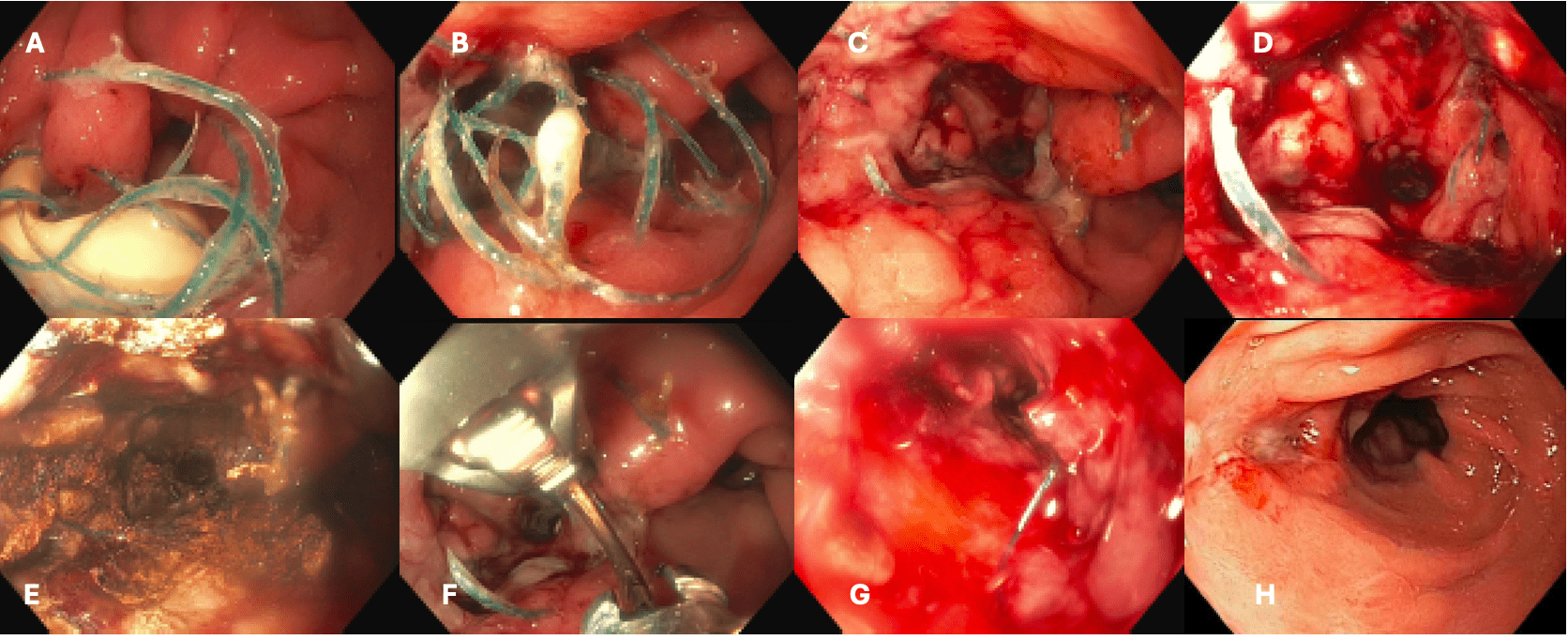
Figure: Figure 1. Endoscopic evaluation showing complete dehiscence after biliopancreatic diversion with duodenal switch. (A,B) Retained suture from prior surgical closure and intraluminal drain. (C,D) Staple line after external drain withdrawal into peritoneal space and endoscopic suture removal. (E) Argon plasma coagulation to staple line/defect to de-epithelialize the tract. (F,G) Endoscopic closure using a full-thickness endoscopic suturing device and helical tack-based endoscopic device. (H) Successful closure at 2 month-follow up demonstrating resolved dehiscence.
Disclosures:
Ronan Allencherril indicated no relevant financial relationships.
Thomas McCarty: Covidien/Medtronic – Consultant. Endoquest Robotics – Consultant.
Ronan Allencherril, MD, Thomas R. McCarty, MD, MPH. P2084 - Endoscopic Closure of Gastric Leak and Wound Dehiscence After Biliopancreatic Diversion With Duodenal Switch, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
