Monday Poster Session
Category: Biliary/Pancreas
P2225 - Timing of Intervention: Assessing Early vs Late Endoscopic and Surgical Interventions in Acute Cholangitis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Silpa Choday, MD (she/her/hers)
Creighton University School of Medicine
Phoenix, AZ
Presenting Author(s)
Silpa Choday, MD, Jad Alsheikh, MD, Paul Kang, MPH, Neil Vyas, MD
Creighton University School of Medicine, Phoenix, AZ
Introduction: Acute cholangitis (AC) is characterized by infection and inflammation of the biliary tree, often resulting from acute biliary obstruction. This study evaluates outcomes of endoscopic retrograde cholangiopancreatography (ERCP) and laparoscopic common bile duct exploration (LCBDE) in the management of acute cholangitis, focusing on timing, complications, and hospital resource utilization.
Methods: Using the Nationwide Readmissions Database (NRD) from 2016 to 2021, we identified AC hospitalizations. This population was further subdivided based on the timing into 4 groups, namely urgent (within 24 hours), early (24-48 hours), late ( >48 hours), or no ERCP/LCBDE. Outcomes included all-cause 30-day readmission rate, length of stay (LOS) in the hospital, total cost (adjusted to inflation in 2021), and in-hospital mortality. P-value ≤ 0.05 was considered statistically significant.
Results: Between 2016-2021, A total of 31,817 patients were included, with 30,330 (95.3%) undergoing ERCP and 1,487 (4.67%) undergoing LCBDE. ERCP patients were older (mean age 64.5 vs. 59.7 years; p < 0.001) with higher Medicare use (56.1% vs. 48.1%) compared to LCBDE patients. LCBDE patients had more elective admissions (19.6% vs. 11.7%; p < 0.001) and were treated more often in non-teaching hospitals (p < 0.001).Complication rates differed significantly: LCBDE patients had higher respiratory failure (3.34% vs. 2.34%; p = 0.026) and bile duct perforation (1.55% vs. 0.64%; p = 0.026), while ERCP patients had higher rates of pancreatitis (p < 0.001) and jaundice (p = 0.002).Late ERCP was associated with higher rates of septic shock (1.23%), respiratory failure (3.80%), and bile duct perforation (0.93%) compared to earlier timing. Patients undergoing late ERCP also had longer hospital stays and higher costs (p < 0.001). LCBDE patients experienced significantly longer hospital stays (mean 8.92 vs. 4.89 days) and higher costs, particularly in late interventions (p < 0.001).
Discussion: ERCP remains the preferred intervention for AC, with earlier procedures resulting in better outcomes and lower resource utilization. LCBDE, while less common, is associated with longer hospital stays and higher costs, particularly when performed late. Optimizing timing for both ERCP and LCBDE is critical to improving patient outcomes and reducing healthcare expenditures.
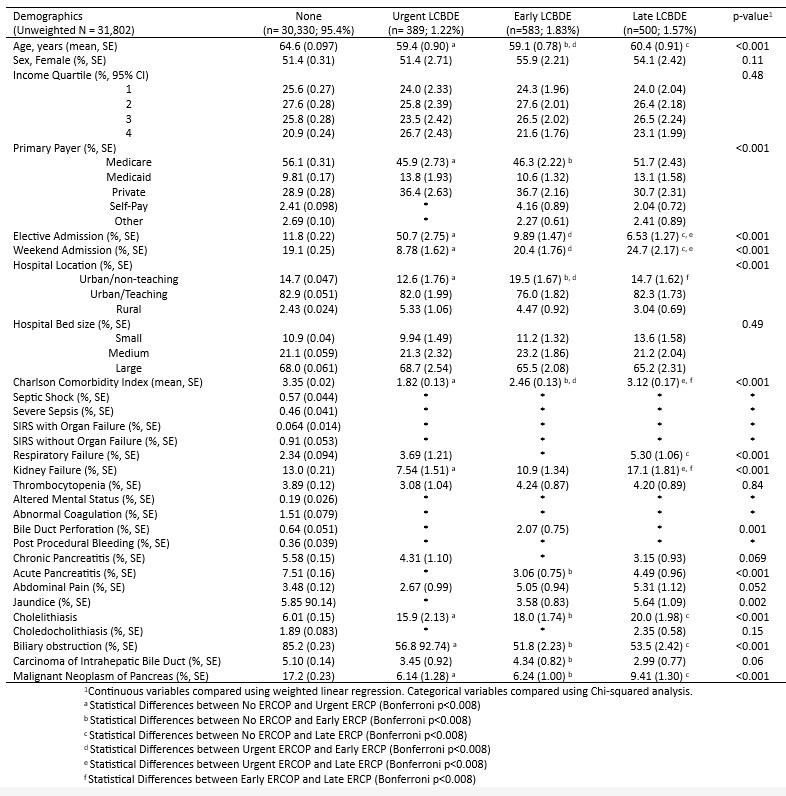
Figure: Table 1: Demographics and clinical characteristics by ERCP Timing
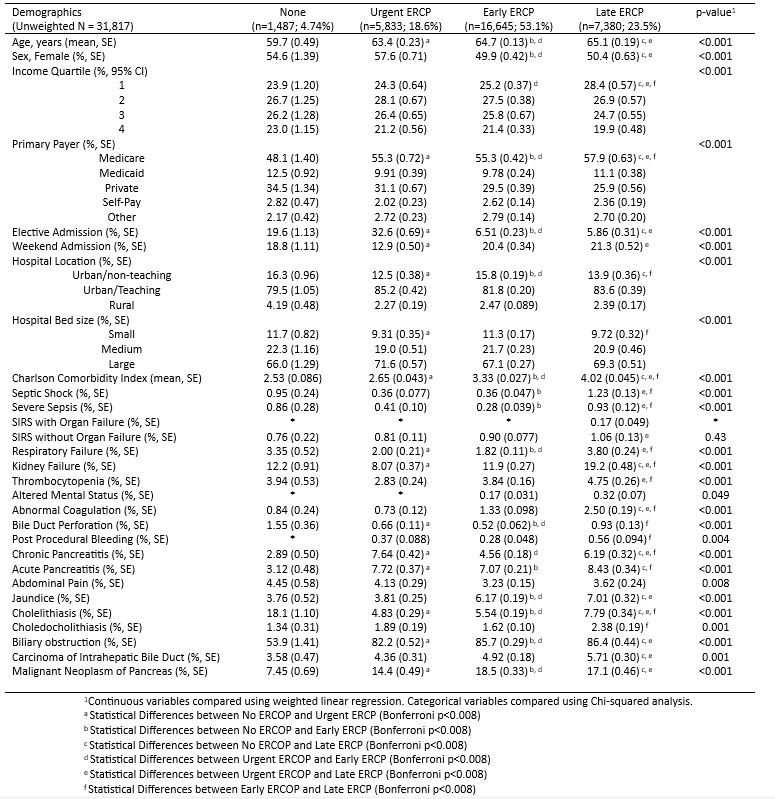
Figure: Table 2: Demographics and clinical characteristics by LCBDE Timing
Disclosures:
Silpa Choday indicated no relevant financial relationships.
Jad Alsheikh indicated no relevant financial relationships.
Paul Kang indicated no relevant financial relationships.
Neil Vyas indicated no relevant financial relationships.
Silpa Choday, MD, Jad Alsheikh, MD, Paul Kang, MPH, Neil Vyas, MD. P2225 - Timing of Intervention: Assessing Early vs Late Endoscopic and Surgical Interventions in Acute Cholangitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Creighton University School of Medicine, Phoenix, AZ
Introduction: Acute cholangitis (AC) is characterized by infection and inflammation of the biliary tree, often resulting from acute biliary obstruction. This study evaluates outcomes of endoscopic retrograde cholangiopancreatography (ERCP) and laparoscopic common bile duct exploration (LCBDE) in the management of acute cholangitis, focusing on timing, complications, and hospital resource utilization.
Methods: Using the Nationwide Readmissions Database (NRD) from 2016 to 2021, we identified AC hospitalizations. This population was further subdivided based on the timing into 4 groups, namely urgent (within 24 hours), early (24-48 hours), late ( >48 hours), or no ERCP/LCBDE. Outcomes included all-cause 30-day readmission rate, length of stay (LOS) in the hospital, total cost (adjusted to inflation in 2021), and in-hospital mortality. P-value ≤ 0.05 was considered statistically significant.
Results: Between 2016-2021, A total of 31,817 patients were included, with 30,330 (95.3%) undergoing ERCP and 1,487 (4.67%) undergoing LCBDE. ERCP patients were older (mean age 64.5 vs. 59.7 years; p < 0.001) with higher Medicare use (56.1% vs. 48.1%) compared to LCBDE patients. LCBDE patients had more elective admissions (19.6% vs. 11.7%; p < 0.001) and were treated more often in non-teaching hospitals (p < 0.001).Complication rates differed significantly: LCBDE patients had higher respiratory failure (3.34% vs. 2.34%; p = 0.026) and bile duct perforation (1.55% vs. 0.64%; p = 0.026), while ERCP patients had higher rates of pancreatitis (p < 0.001) and jaundice (p = 0.002).Late ERCP was associated with higher rates of septic shock (1.23%), respiratory failure (3.80%), and bile duct perforation (0.93%) compared to earlier timing. Patients undergoing late ERCP also had longer hospital stays and higher costs (p < 0.001). LCBDE patients experienced significantly longer hospital stays (mean 8.92 vs. 4.89 days) and higher costs, particularly in late interventions (p < 0.001).
Discussion: ERCP remains the preferred intervention for AC, with earlier procedures resulting in better outcomes and lower resource utilization. LCBDE, while less common, is associated with longer hospital stays and higher costs, particularly when performed late. Optimizing timing for both ERCP and LCBDE is critical to improving patient outcomes and reducing healthcare expenditures.
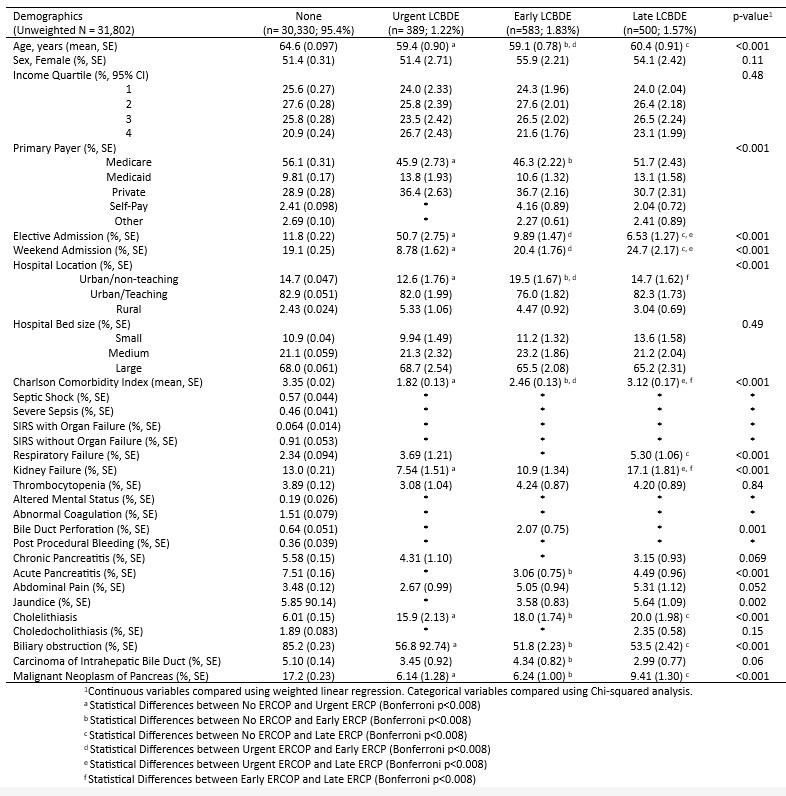
Figure: Table 1: Demographics and clinical characteristics by ERCP Timing
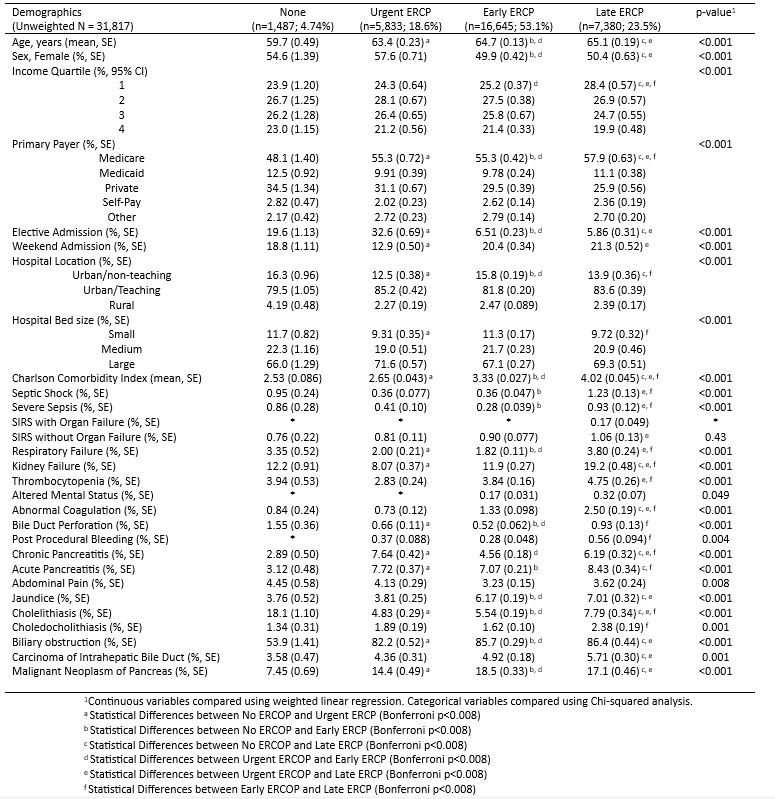
Figure: Table 2: Demographics and clinical characteristics by LCBDE Timing
Disclosures:
Silpa Choday indicated no relevant financial relationships.
Jad Alsheikh indicated no relevant financial relationships.
Paul Kang indicated no relevant financial relationships.
Neil Vyas indicated no relevant financial relationships.
Silpa Choday, MD, Jad Alsheikh, MD, Paul Kang, MPH, Neil Vyas, MD. P2225 - Timing of Intervention: Assessing Early vs Late Endoscopic and Surgical Interventions in Acute Cholangitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
