Monday Poster Session
Category: Biliary/Pancreas
P2220 - Is It Beneficial to Dilate the Lumen-Apposing Metal Stent After Placement for EUS-Guided Gallbladder Drainage?
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- FG
Fady Gendy, DO
Geisinger Health System
Danville, PA
Presenting Author(s)
Fady Gendy, DO1, Michael Makar, MD1, Michael Yodice, MD1, Andrea Berger, MSc1, David L.. Diehl, MD1, Harshit S. Khara, MD2, Bradley D. Confer, DO1
1Geisinger Health System, Danville, PA; 2Geisinger Health System, Danville, NJ
Introduction: Endoscopic ultrasound-guided gallbladder drainage (EUS-GB) using lumen-apposing metal stents (LAMS) has become an important treatment option for patients with cholecystitis who are not surgical candidates. Immediate dilation of the LAMS during the procedure has been suggested to allow for better drainage and improve clinical outcomes. However, potential adverse events such as bleeding or stent migration may occur. There is no current data on the risk and benefit of LAMS immediate dilation. This study aimed to compare the clinical outcomes and adverse events of EUS-GB LAMS with dilation (LAMS-D) and LAMS without dilation (LAMS-ND).
Methods: Endoscopic ultrasound-guided gallbladder drainage (EUS-GB) using lumen-apposing metal stents (LAMS) has become an important treatment option for patients with cholecystitis who are not surgical candidates. Immediate dilation of the LAMS during the procedure has been suggested to allow for better drainage and improve clinical outcomes. However, potential adverse events such as bleeding or stent migration may occur. There is no current data on the risk and benefit of LAMS immediate dilation. This study aimed to compare the clinical outcomes and adverse events of EUS-GB LAMS with dilation (LAMS-D) and LAMS without dilation (LAMS-ND).
Results: A total of 214 patients were included of which 46.3% were female and the median age was 79.6 years. The LAMS was dilated in 122 (57%) of patients. Technical success was achieved in 100% of the LAMS-D group vs 96.7% for LAMS-ND (p=0.08). Clinical success was achieved in 98.4% of LAMS-D vs 94.6% in LAMS-ND (p=0.14). Patients with LAMS-D were more likely to have a 15mm LAMS compared to LAMS-ND (86.1% vs 59.8%, p< 0.001). There was no significant difference in 30-day post-procedure overall adverse events between the two groups (16.4% vs 12.0%, p=0.36). There was no significant difference in LAMS occlusion (0% vs 1.1%, p=0.43), LAMS migration (1.6% vs 0%, p=0.51), bleeding (4.9% vs 2.2%, p=0.47) or recurrent cholecystitis (4.1% vs 5.4%, p=0.53) between the two groups.
Discussion: Dilation of the LAMS in EUS-GB did not affect adverse events or clinical outcomes. An individualized approach to dilate the LAMS should be based on patient’s clinical presentation and gallbladder characteristics. Additional larger studies are necessary to confirm these findings.
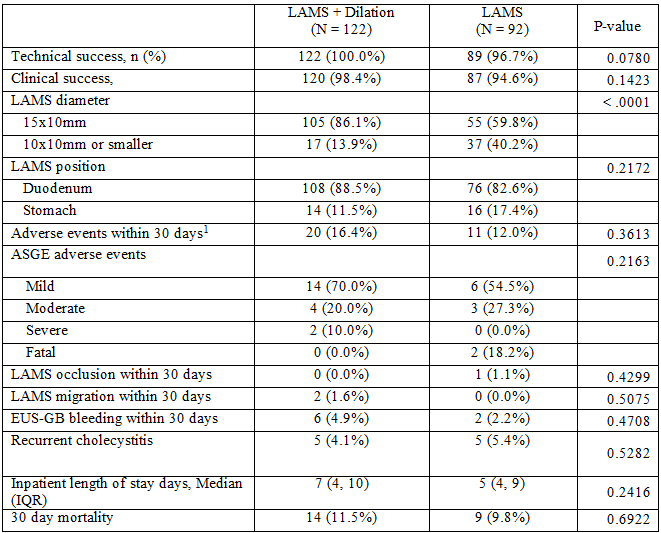
Figure: Comparison of outcomes between LAMS+Dilation and LAMS alone, showing that there was no significant difference in outcomes.
1: pneumoperitoneum, stent migration, bleeding, stent occlusion, abdominal pain, nausea/vomiting, cardiopulmonary, misdeployed stent
Disclosures:
Fady Gendy indicated no relevant financial relationships.
Michael Makar indicated no relevant financial relationships.
Michael Yodice indicated no relevant financial relationships.
Andrea Berger indicated no relevant financial relationships.
David Diehl indicated no relevant financial relationships.
Harshit Khara indicated no relevant financial relationships.
Bradley Confer indicated no relevant financial relationships.
Fady Gendy, DO1, Michael Makar, MD1, Michael Yodice, MD1, Andrea Berger, MSc1, David L.. Diehl, MD1, Harshit S. Khara, MD2, Bradley D. Confer, DO1. P2220 - Is It Beneficial to Dilate the Lumen-Apposing Metal Stent After Placement for EUS-Guided Gallbladder Drainage?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Geisinger Health System, Danville, PA; 2Geisinger Health System, Danville, NJ
Introduction: Endoscopic ultrasound-guided gallbladder drainage (EUS-GB) using lumen-apposing metal stents (LAMS) has become an important treatment option for patients with cholecystitis who are not surgical candidates. Immediate dilation of the LAMS during the procedure has been suggested to allow for better drainage and improve clinical outcomes. However, potential adverse events such as bleeding or stent migration may occur. There is no current data on the risk and benefit of LAMS immediate dilation. This study aimed to compare the clinical outcomes and adverse events of EUS-GB LAMS with dilation (LAMS-D) and LAMS without dilation (LAMS-ND).
Methods: Endoscopic ultrasound-guided gallbladder drainage (EUS-GB) using lumen-apposing metal stents (LAMS) has become an important treatment option for patients with cholecystitis who are not surgical candidates. Immediate dilation of the LAMS during the procedure has been suggested to allow for better drainage and improve clinical outcomes. However, potential adverse events such as bleeding or stent migration may occur. There is no current data on the risk and benefit of LAMS immediate dilation. This study aimed to compare the clinical outcomes and adverse events of EUS-GB LAMS with dilation (LAMS-D) and LAMS without dilation (LAMS-ND).
Results: A total of 214 patients were included of which 46.3% were female and the median age was 79.6 years. The LAMS was dilated in 122 (57%) of patients. Technical success was achieved in 100% of the LAMS-D group vs 96.7% for LAMS-ND (p=0.08). Clinical success was achieved in 98.4% of LAMS-D vs 94.6% in LAMS-ND (p=0.14). Patients with LAMS-D were more likely to have a 15mm LAMS compared to LAMS-ND (86.1% vs 59.8%, p< 0.001). There was no significant difference in 30-day post-procedure overall adverse events between the two groups (16.4% vs 12.0%, p=0.36). There was no significant difference in LAMS occlusion (0% vs 1.1%, p=0.43), LAMS migration (1.6% vs 0%, p=0.51), bleeding (4.9% vs 2.2%, p=0.47) or recurrent cholecystitis (4.1% vs 5.4%, p=0.53) between the two groups.
Discussion: Dilation of the LAMS in EUS-GB did not affect adverse events or clinical outcomes. An individualized approach to dilate the LAMS should be based on patient’s clinical presentation and gallbladder characteristics. Additional larger studies are necessary to confirm these findings.
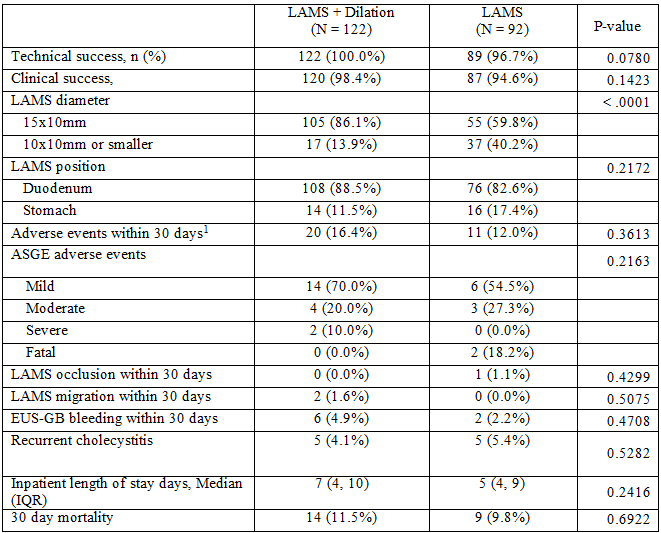
Figure: Comparison of outcomes between LAMS+Dilation and LAMS alone, showing that there was no significant difference in outcomes.
1: pneumoperitoneum, stent migration, bleeding, stent occlusion, abdominal pain, nausea/vomiting, cardiopulmonary, misdeployed stent
Disclosures:
Fady Gendy indicated no relevant financial relationships.
Michael Makar indicated no relevant financial relationships.
Michael Yodice indicated no relevant financial relationships.
Andrea Berger indicated no relevant financial relationships.
David Diehl indicated no relevant financial relationships.
Harshit Khara indicated no relevant financial relationships.
Bradley Confer indicated no relevant financial relationships.
Fady Gendy, DO1, Michael Makar, MD1, Michael Yodice, MD1, Andrea Berger, MSc1, David L.. Diehl, MD1, Harshit S. Khara, MD2, Bradley D. Confer, DO1. P2220 - Is It Beneficial to Dilate the Lumen-Apposing Metal Stent After Placement for EUS-Guided Gallbladder Drainage?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
