Monday Poster Session
Category: Biliary/Pancreas
P2191 - IgG4-Related Sclerosing Cholangitis (IgG4-SC) versus Primary Sclerosing Cholangitis (PSC): A Systematic Review and Meta-Analysis of Comparative Studies
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mark C. Wang, MD (he/him/his)
Keck School of Medicine of the University of Southern California
Los Angeles, CA
Presenting Author(s)
Mark C. Wang, MD1, Albert Chong, MD, MPH2, Erick Cruz Grave, MD1, Abby Kunitsky, DO3, Kabir Rahal, 4, Lucas Nastaskin, 5, James Buxbaum, MD1
1Keck School of Medicine of the University of Southern California, Los Angeles, CA; 2Mayo Clinic College of Medicine and Science, Scottsdale, AZ; 3McLaren Macomb Hospital, Mt Clemens, MI; 4University of California Los Angeles, Los Angeles, CA; 5University of Southern California, Los Angeles, CA
Introduction: IgG4-related sclerosing cholangitis (IgG4-SC) is challenging to distinguish from PSC due to similar clinical and radiographic features and thus may be overlooked by clinicians. Consequently, IgG4-SC patients have been misdiagnosed with PSC, which is critical as IgG4-SC improves with steroids while PSC requires liver transplantation for definitive management. Thus, we aimed to identify features distinguishing IgG4-SC from PSC by systematic review and meta-analysis of comparative studies.
Methods: A systematic literature search identified articles comparing IgG4-SC and PSC. PubMed, Embase, and Web of Science were searched from inception to November 2023. Included studies consisted of primary sources comparing patients with IgG4-SC and PSC that were published in journals or presented at scientific meetings. Clinical, laboratory, endoscopic, radiologic, and histologic data were collected. Meta-analyses were performed with the random effects model. For continuous variables, pooled means and standard mean differences were generated. For categorical variables, pooled proportions and odds ratios were generated. All data is presented with 95% confidence intervals (CI).
Results: The literature search yielded 866 abstracts, with 38 studies meeting criteria. We identified IgG4-SC patients to be older, more male (OR 2.80 [2.01-3.90]), and have history of pancreatic pathology, while PSC was more associated with IBD and cholangiocarcinoma (Table 1). Otherwise, they had similar clinical presentations. In addition to higher serum IgG4 (486.8 vs 50.5 mg/dL, p< 0.001), IgG4-SC patients had higher CRP, total IgG, IgG2, and bile IgG4 levels (Table 2). Distinctive structural findings of IgG4-SC included long biliary strictures (OR 31.5 [1.71-578.1]), distal strictures, swelling of the ampulla, and symmetric regular biliary mucosa (Table 2). PSC was more likely to demonstrate diverticulum-like outpouching and beaded appearance. IgG4-SC was associated with biopsies showing IgG4 plasma cells and portal inflammatory nodules, yet other histologic findings were similar (Table 1).
Discussion: This comprehensive meta-analysis underscores features that should suggest IgG4-SC as an alternative diagnosis to PSC. These include older age at onset, male sex, history of pancreatic pathology, long strictures with symmetric thickening, and swelling of the ampulla. As IgG4-SC is treatable with steroids, this study supports thorough serologic testing and staining of histologic specimens for IgG4 in patients with these features.
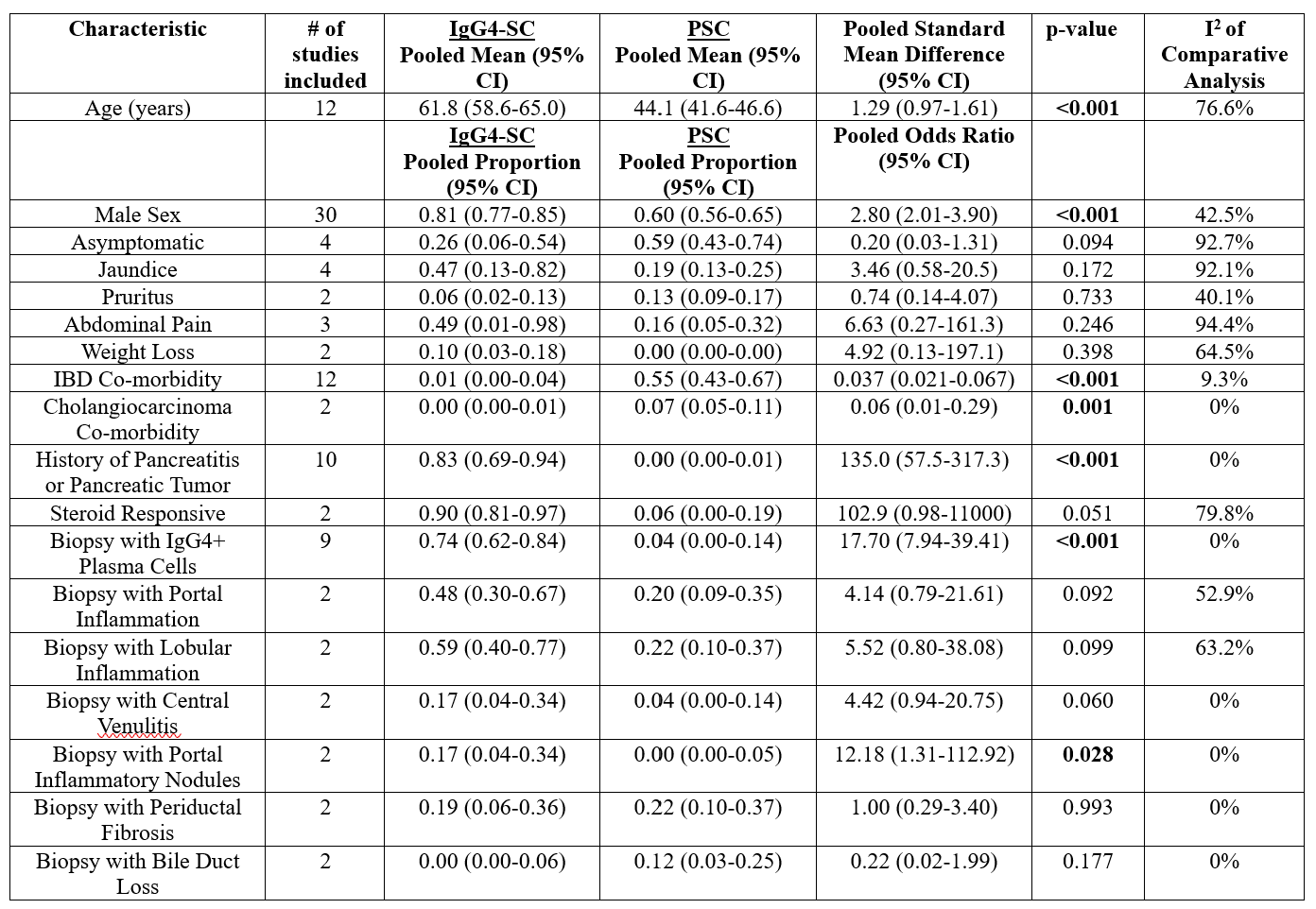
Figure: Table 1: Clinical and Histologic Characteristics of IgG4-SC versus PSC
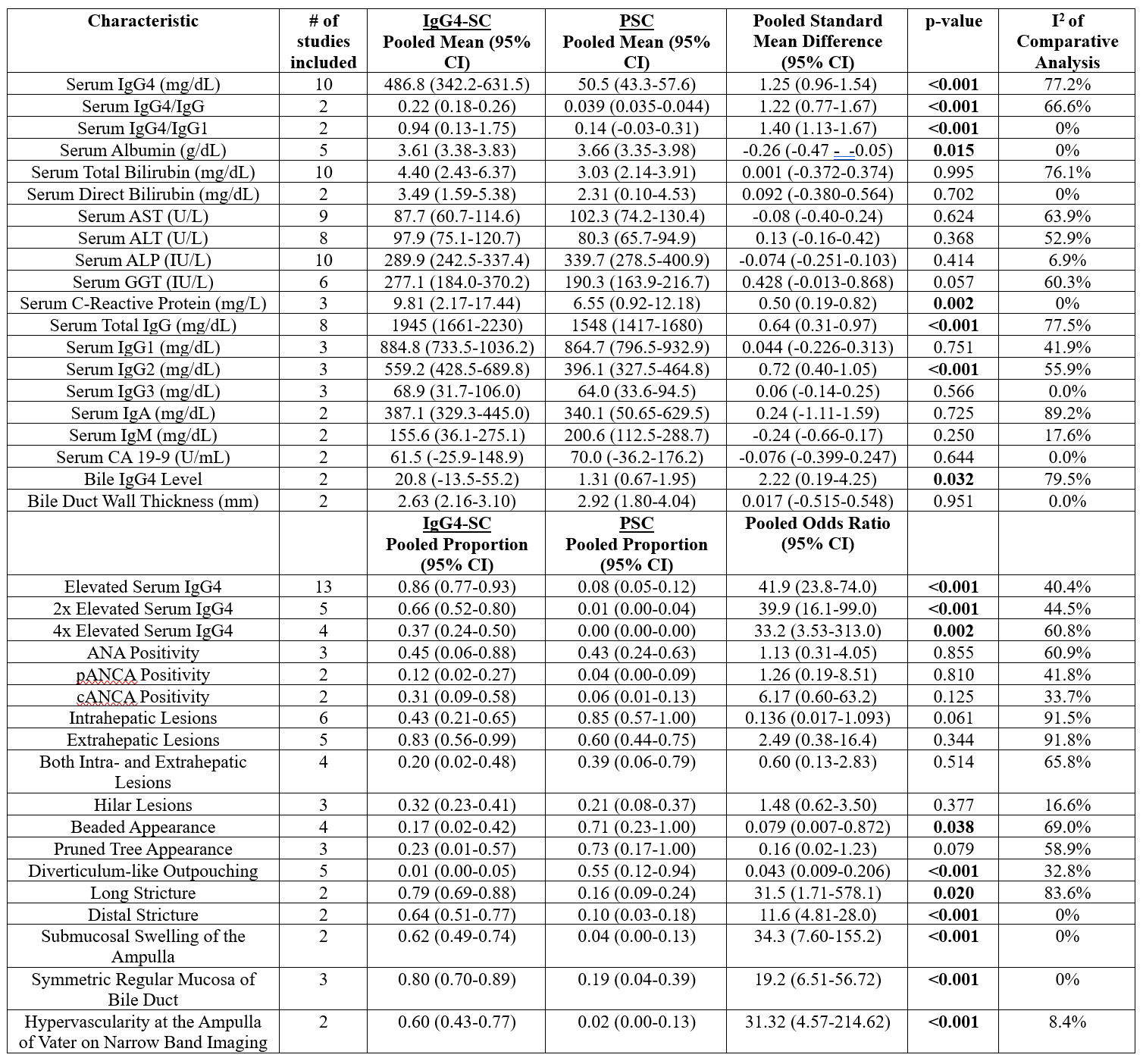
Figure: Table 2: Laboratory and Structural Characteristics of IgG4-SC versus PSC
Disclosures:
Mark Wang indicated no relevant financial relationships.
Albert Chong indicated no relevant financial relationships.
Erick Cruz Grave indicated no relevant financial relationships.
Abby Kunitsky indicated no relevant financial relationships.
Kabir Rahal indicated no relevant financial relationships.
Lucas Nastaskin indicated no relevant financial relationships.
James Buxbaum: Boston Scientific – Consultant. Olympus – Consultant.
Mark C. Wang, MD1, Albert Chong, MD, MPH2, Erick Cruz Grave, MD1, Abby Kunitsky, DO3, Kabir Rahal, 4, Lucas Nastaskin, 5, James Buxbaum, MD1. P2191 - IgG4-Related Sclerosing Cholangitis (IgG4-SC) versus Primary Sclerosing Cholangitis (PSC): A Systematic Review and Meta-Analysis of Comparative Studies, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Keck School of Medicine of the University of Southern California, Los Angeles, CA; 2Mayo Clinic College of Medicine and Science, Scottsdale, AZ; 3McLaren Macomb Hospital, Mt Clemens, MI; 4University of California Los Angeles, Los Angeles, CA; 5University of Southern California, Los Angeles, CA
Introduction: IgG4-related sclerosing cholangitis (IgG4-SC) is challenging to distinguish from PSC due to similar clinical and radiographic features and thus may be overlooked by clinicians. Consequently, IgG4-SC patients have been misdiagnosed with PSC, which is critical as IgG4-SC improves with steroids while PSC requires liver transplantation for definitive management. Thus, we aimed to identify features distinguishing IgG4-SC from PSC by systematic review and meta-analysis of comparative studies.
Methods: A systematic literature search identified articles comparing IgG4-SC and PSC. PubMed, Embase, and Web of Science were searched from inception to November 2023. Included studies consisted of primary sources comparing patients with IgG4-SC and PSC that were published in journals or presented at scientific meetings. Clinical, laboratory, endoscopic, radiologic, and histologic data were collected. Meta-analyses were performed with the random effects model. For continuous variables, pooled means and standard mean differences were generated. For categorical variables, pooled proportions and odds ratios were generated. All data is presented with 95% confidence intervals (CI).
Results: The literature search yielded 866 abstracts, with 38 studies meeting criteria. We identified IgG4-SC patients to be older, more male (OR 2.80 [2.01-3.90]), and have history of pancreatic pathology, while PSC was more associated with IBD and cholangiocarcinoma (Table 1). Otherwise, they had similar clinical presentations. In addition to higher serum IgG4 (486.8 vs 50.5 mg/dL, p< 0.001), IgG4-SC patients had higher CRP, total IgG, IgG2, and bile IgG4 levels (Table 2). Distinctive structural findings of IgG4-SC included long biliary strictures (OR 31.5 [1.71-578.1]), distal strictures, swelling of the ampulla, and symmetric regular biliary mucosa (Table 2). PSC was more likely to demonstrate diverticulum-like outpouching and beaded appearance. IgG4-SC was associated with biopsies showing IgG4 plasma cells and portal inflammatory nodules, yet other histologic findings were similar (Table 1).
Discussion: This comprehensive meta-analysis underscores features that should suggest IgG4-SC as an alternative diagnosis to PSC. These include older age at onset, male sex, history of pancreatic pathology, long strictures with symmetric thickening, and swelling of the ampulla. As IgG4-SC is treatable with steroids, this study supports thorough serologic testing and staining of histologic specimens for IgG4 in patients with these features.
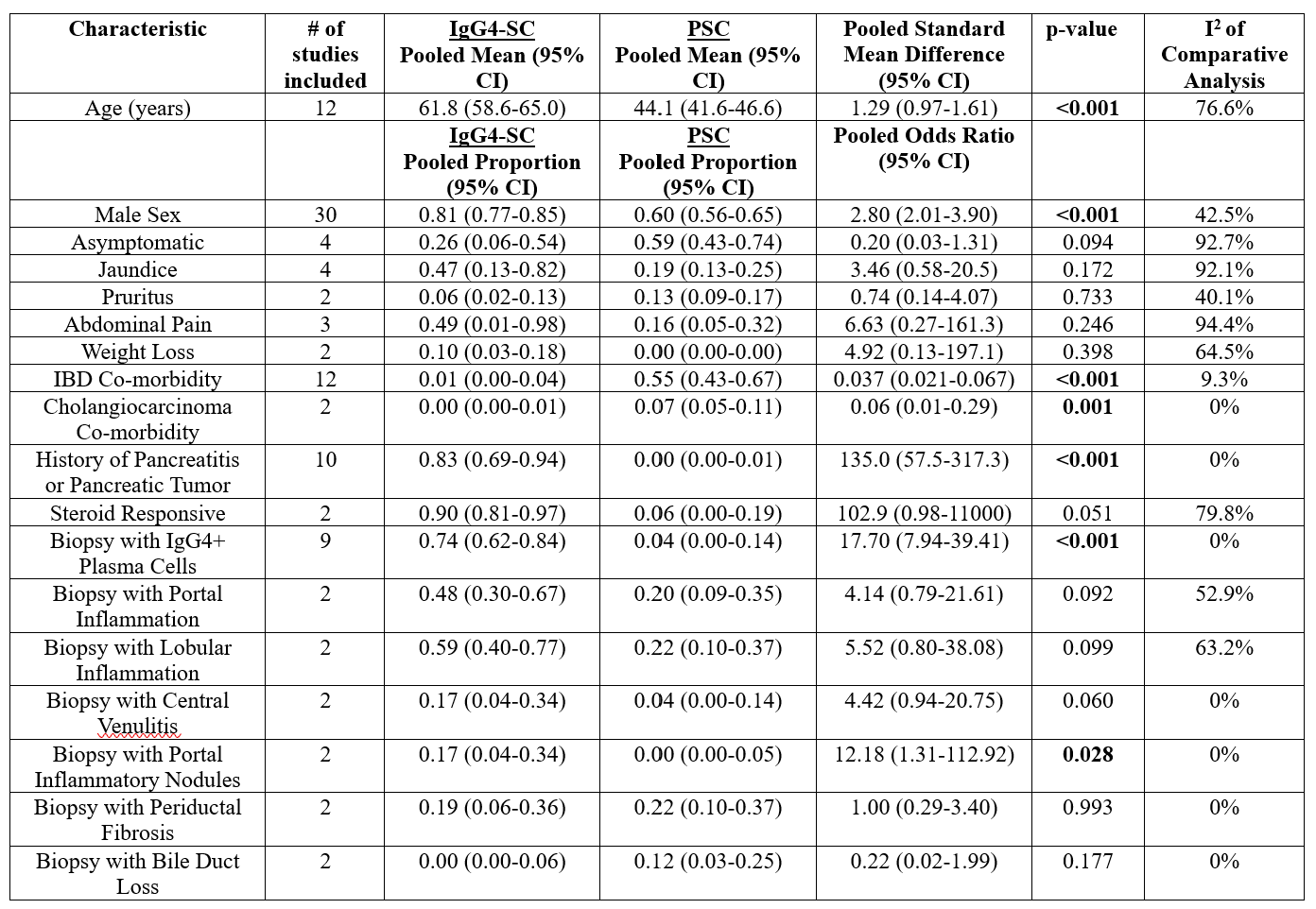
Figure: Table 1: Clinical and Histologic Characteristics of IgG4-SC versus PSC
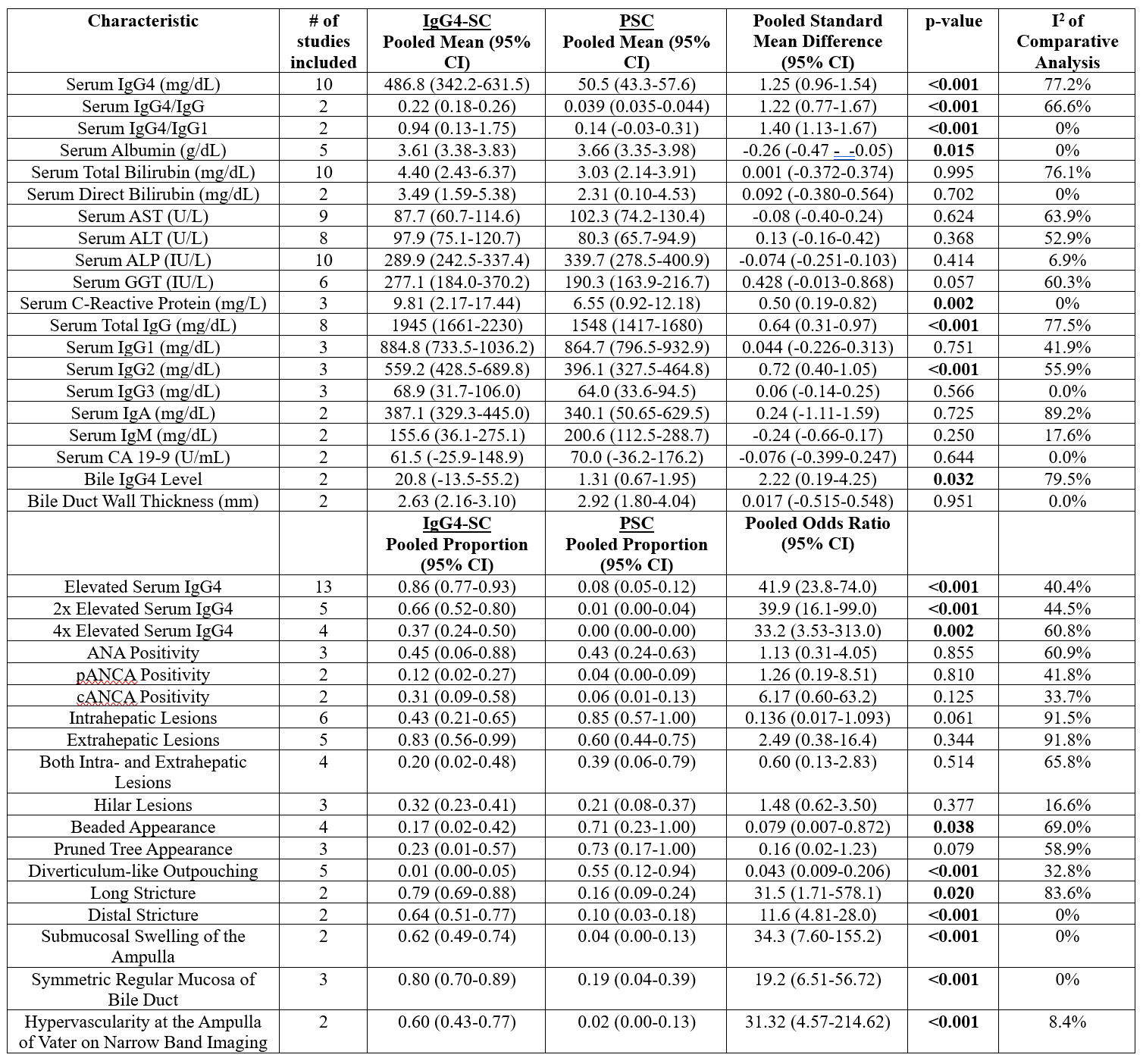
Figure: Table 2: Laboratory and Structural Characteristics of IgG4-SC versus PSC
Disclosures:
Mark Wang indicated no relevant financial relationships.
Albert Chong indicated no relevant financial relationships.
Erick Cruz Grave indicated no relevant financial relationships.
Abby Kunitsky indicated no relevant financial relationships.
Kabir Rahal indicated no relevant financial relationships.
Lucas Nastaskin indicated no relevant financial relationships.
James Buxbaum: Boston Scientific – Consultant. Olympus – Consultant.
Mark C. Wang, MD1, Albert Chong, MD, MPH2, Erick Cruz Grave, MD1, Abby Kunitsky, DO3, Kabir Rahal, 4, Lucas Nastaskin, 5, James Buxbaum, MD1. P2191 - IgG4-Related Sclerosing Cholangitis (IgG4-SC) versus Primary Sclerosing Cholangitis (PSC): A Systematic Review and Meta-Analysis of Comparative Studies, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
