Monday Poster Session
Category: Biliary/Pancreas
P2387 - Acute Pancreatitis Following a Recent COVID-19 Infection and Antimicrobial Therapy: A Case for Pharmacovigilance
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Shirley Perez Añel, MD (she/her/hers)
St. Mary's General Hospital, New York Medical College
Passaic, NJ
Presenting Author(s)
Shirley Perez Añel, MD1, Hamza S. Ansari, MBBS1, Maidelin Cabrera Morales, DM1, Shawn Shaji, MBBS1, Giulio Quarta, MD2, Jennifer Gilmore, MD, MBA1, Joseph Roth, MD3, Frantz Pierre-Louis, MD3
1St. Mary's General Hospital, New York Medical College, Passaic, NJ; 2Gastroenterology Associates of New Jersey, Clifton, NJ; 3Saint Mary’s General Hospital, Passaic, NJ
Introduction: Drug-induced acute pancreatitis (DIAP) is an underrecognized condition due to its diagnostic challenges. While a large number of medications has been associated with DIAP, the incidence of this entity remains underestimated. We report a case of tail-predominant acute pancreatitis mimicking renal pathology in a patient following a recent COVID-19 infection and use of Paxlovid and cephalexin.
Case Description/
Methods: A 67-year-old woman with a history of hypertension, recently treated with Paxlovid for COVID-19 (Feb 25–Mar 2) and Cephalexin for a urinary tract infection (Mar 6–8), presented on Mar 9 with severe left flank pain. Initial evaluation revealed temperature 100.2°F, heart rate 125 bpm, respiratory rate 26 rpm, and left flank tenderness. Further assessment showed elevated white blood cell count (WBC 17,000/μL), ESR (18 mm/h), CRP (9.4 mg/L), amylase (191 U/L) and lipase (139 U/L), with normal triglycerides. Urolithiasis and acute pyelonephritis were strongly suspected prompting imaging of the abdomen. Surprisingly, computer tomography (CT) revealed acute pancreatitis localized to the pancreatic tail, with early pseudocyst formation and extension into the left perirenal space. Magnetic resonance cholangiopancreatography (MRCP) confirmed a 1.5 cm hyperintense lesion in the tail consistent with focal pancreatitis. Management included discontinuation of the agents, bowel rest, intravenous fluids, and analgesia, which resulted in resolution of the pain and tolerance of oral intake by hospital day 2. Discharge occurred on day 3. A two-week outpatient follow-up CT confirmed a stable pseudocyst. Endoscopic ultrasound (EUS) revealed a side-branch intraductal papillary mucinous neoplasm (IPMN) in the pancreatic tail, which did not communicate with the main pancreatic duct.
Discussion: This case underscores a rare but clinically relevant condition—drug-induced acute pancreatitis—potentially associated with the sequential use of Paxlovid and Cephalexin following a COVID-19 infection. The close association between infection, initiation of each agent, and symptoms onset suggest a possible idiosyncratic or accumulative toxic effect, rather than the impact of the incidental non-communicating IPMN. Tail-dominant acute pancreatitis may mimic renal pathology, which can only be unmasked by high-quality care including detailed imaging. Reconsidering the presumptive diagnosis, suspecting a medication interaction, and contributing to pharmacovigilance efforts should be priority to healthcare providers.
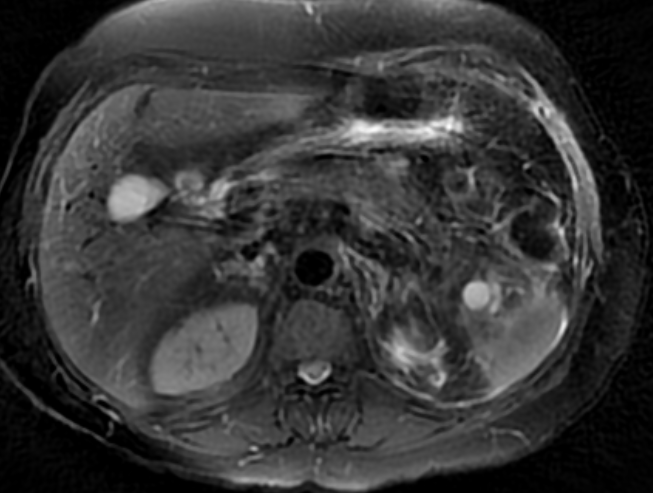
Figure: Figure 1. Computed tomography (CT) of Abdomen and Pelvis revealing acute pancreatitis localized to the pancreatic tail, with early pseudocyst formation and extension into the left perirenal space.
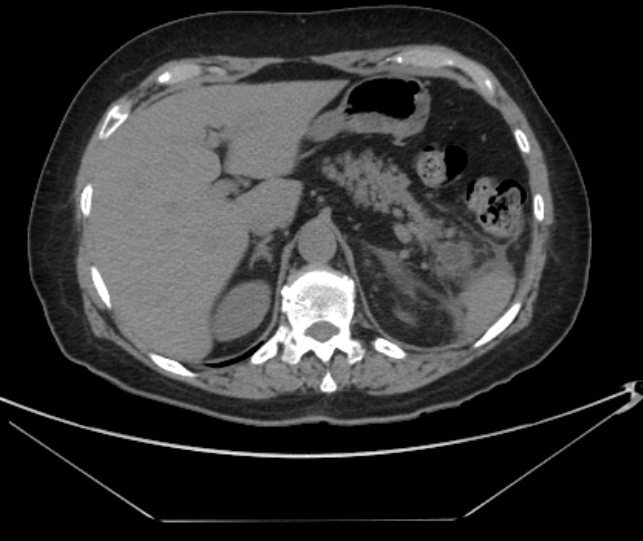
Figure: Figure 2. Magnetic Resonance cholangiopancreatography (MRCP) showing 1.5 cm hypertense lesion in the tail consistent with focal pancreatitis.
Disclosures:
Shirley Perez Añel indicated no relevant financial relationships.
Hamza Ansari indicated no relevant financial relationships.
Maidelin Cabrera Morales indicated no relevant financial relationships.
Shawn Shaji indicated no relevant financial relationships.
Giulio Quarta indicated no relevant financial relationships.
Jennifer Gilmore indicated no relevant financial relationships.
Joseph Roth indicated no relevant financial relationships.
Frantz Pierre-Louis indicated no relevant financial relationships.
Shirley Perez Añel, MD1, Hamza S. Ansari, MBBS1, Maidelin Cabrera Morales, DM1, Shawn Shaji, MBBS1, Giulio Quarta, MD2, Jennifer Gilmore, MD, MBA1, Joseph Roth, MD3, Frantz Pierre-Louis, MD3. P2387 - Acute Pancreatitis Following a Recent COVID-19 Infection and Antimicrobial Therapy: A Case for Pharmacovigilance, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1St. Mary's General Hospital, New York Medical College, Passaic, NJ; 2Gastroenterology Associates of New Jersey, Clifton, NJ; 3Saint Mary’s General Hospital, Passaic, NJ
Introduction: Drug-induced acute pancreatitis (DIAP) is an underrecognized condition due to its diagnostic challenges. While a large number of medications has been associated with DIAP, the incidence of this entity remains underestimated. We report a case of tail-predominant acute pancreatitis mimicking renal pathology in a patient following a recent COVID-19 infection and use of Paxlovid and cephalexin.
Case Description/
Methods: A 67-year-old woman with a history of hypertension, recently treated with Paxlovid for COVID-19 (Feb 25–Mar 2) and Cephalexin for a urinary tract infection (Mar 6–8), presented on Mar 9 with severe left flank pain. Initial evaluation revealed temperature 100.2°F, heart rate 125 bpm, respiratory rate 26 rpm, and left flank tenderness. Further assessment showed elevated white blood cell count (WBC 17,000/μL), ESR (18 mm/h), CRP (9.4 mg/L), amylase (191 U/L) and lipase (139 U/L), with normal triglycerides. Urolithiasis and acute pyelonephritis were strongly suspected prompting imaging of the abdomen. Surprisingly, computer tomography (CT) revealed acute pancreatitis localized to the pancreatic tail, with early pseudocyst formation and extension into the left perirenal space. Magnetic resonance cholangiopancreatography (MRCP) confirmed a 1.5 cm hyperintense lesion in the tail consistent with focal pancreatitis. Management included discontinuation of the agents, bowel rest, intravenous fluids, and analgesia, which resulted in resolution of the pain and tolerance of oral intake by hospital day 2. Discharge occurred on day 3. A two-week outpatient follow-up CT confirmed a stable pseudocyst. Endoscopic ultrasound (EUS) revealed a side-branch intraductal papillary mucinous neoplasm (IPMN) in the pancreatic tail, which did not communicate with the main pancreatic duct.
Discussion: This case underscores a rare but clinically relevant condition—drug-induced acute pancreatitis—potentially associated with the sequential use of Paxlovid and Cephalexin following a COVID-19 infection. The close association between infection, initiation of each agent, and symptoms onset suggest a possible idiosyncratic or accumulative toxic effect, rather than the impact of the incidental non-communicating IPMN. Tail-dominant acute pancreatitis may mimic renal pathology, which can only be unmasked by high-quality care including detailed imaging. Reconsidering the presumptive diagnosis, suspecting a medication interaction, and contributing to pharmacovigilance efforts should be priority to healthcare providers.
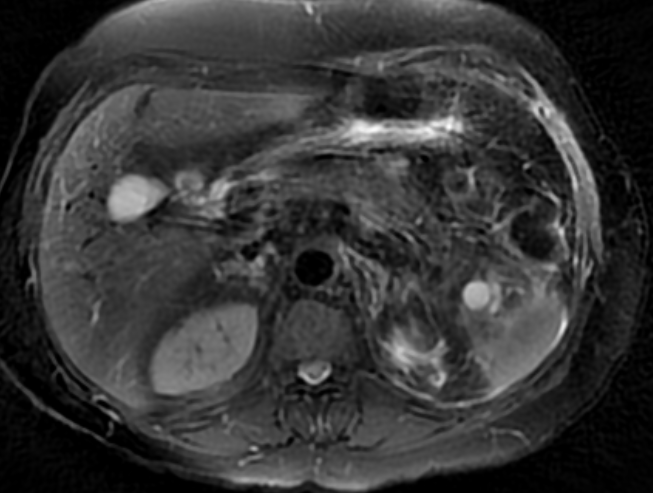
Figure: Figure 1. Computed tomography (CT) of Abdomen and Pelvis revealing acute pancreatitis localized to the pancreatic tail, with early pseudocyst formation and extension into the left perirenal space.
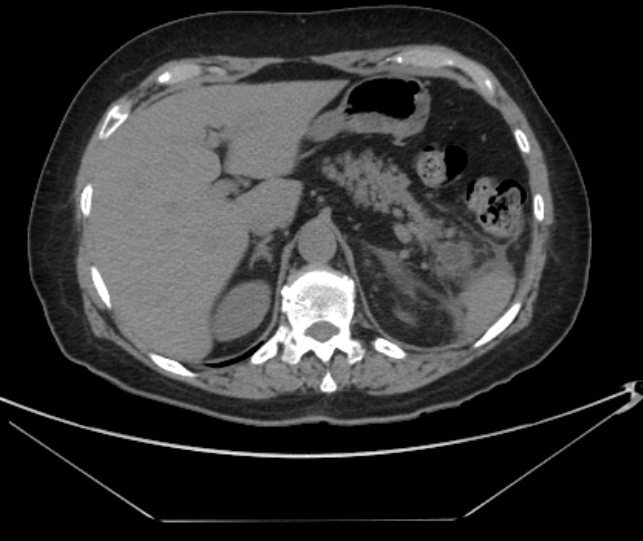
Figure: Figure 2. Magnetic Resonance cholangiopancreatography (MRCP) showing 1.5 cm hypertense lesion in the tail consistent with focal pancreatitis.
Disclosures:
Shirley Perez Añel indicated no relevant financial relationships.
Hamza Ansari indicated no relevant financial relationships.
Maidelin Cabrera Morales indicated no relevant financial relationships.
Shawn Shaji indicated no relevant financial relationships.
Giulio Quarta indicated no relevant financial relationships.
Jennifer Gilmore indicated no relevant financial relationships.
Joseph Roth indicated no relevant financial relationships.
Frantz Pierre-Louis indicated no relevant financial relationships.
Shirley Perez Añel, MD1, Hamza S. Ansari, MBBS1, Maidelin Cabrera Morales, DM1, Shawn Shaji, MBBS1, Giulio Quarta, MD2, Jennifer Gilmore, MD, MBA1, Joseph Roth, MD3, Frantz Pierre-Louis, MD3. P2387 - Acute Pancreatitis Following a Recent COVID-19 Infection and Antimicrobial Therapy: A Case for Pharmacovigilance, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
