Monday Poster Session
Category: Esophagus
P2769 - Trends and Outcomes of Endoscopic vs Surgical Management of Boerhaave Syndrome: A National Inpatient Sample Analysis (2018–2022)
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Daniel Alejandro Gonzalez Mosquera, MD (he/him/his)
NYC Health + Hospitals/Lincoln
Bronx, NY
Presenting Author(s)
Daniel Alejandro. Gonzalez Mosquera, MD1, Maria Belen Mateo, MD2, Mariana Nunes Ferreira, MD1, Carolina Gonzalez Mosquera, MD3, Juan Martinez-Ortega, MD4, Yassine Kilani, MD5, Cynthia Victor-Prophete, MD4
1NYC Health + Hospitals/Lincoln, Bronx, NY; 2Knowledge and Research Evaluation Unit, Mayo Clinic, Rochester, Minnesota, USA, Rochester, MN; 3Universidad Católica Santiago de Guayaquil, Guayaquil, Guayas, Ecuador; 4New York Health + Hospitals | Lincoln–Weill Cornell Medical College Affiliate, New York, USA, Bronx, NY; 5Saint Louis University School of Medicine, Saint Louis, MO
Introduction: Boerhaave syndrome, is a rare but life-threatening gastrointestinal emergency. Management strategies typically involve surgical repair or increasingly common endoscopic intervention. Data comparing national trends and inpatient outcomes between these approaches remain limited.
Understanding how these strategies differ in terms of mortality, complications, and resource utilization is critical for optimizing patient care.
Methods: We used the National Inpatient Sample (2018–2022) to identify adult hospitalizations with a principal diagnosis of Boerhaave syndrome (ICD-10: K22.3). Patients were stratified into endoscopic or surgical management groups using ICD-10-PCS procedure codes. Outcomes included inpatient mortality, length of stay (LOS), and complications (sepsis, mediastinitis, ICU-level care). Multivariable survey-weighted logistic and linear regressions were used to compare outcomes between groups and assess trends over time.
Results: Among 2,865 hospitalizations, 1,340 (46.8%) underwent endoscopic management, 1,080 (37.7%) surgical, and 445 (15.5%) both. Mortality was highest with endoscopic management (8.6%) compared to surgical (6.9%) and combined approaches (3.4%). Endoscopic management was associated with higher mortality odds (aOR 1.61, 95% CI: 1.01–2.59). ICU admissions were significantly more common in surgical and combined groups (p< 0.001). Surgical management showed notably higher sepsis complications (aOR 4.06, 95% CI: 2.88–5.71). Mediastinitis was rare across groups. LOS was shortest with endoscopic management (11.2 days vs. 18.8–19.0 days).
Endoscopic management increased from 44.4% in 2018 to 54.1% in 2022, while surgical interventions declined. Mortality odds did not significantly differ year-to-year.
Discussion: In this large, real-world cohort, endoscopic management of Boerhaave syndrome, though less invasive, was associated with higher inpatient mortality and lower ICU utilization compared to surgical approaches. Surgical and combined interventions demonstrated higher resource use and sepsis rates but lower mortality. These findings shows the importance of individualized treatment selection and suggest that while endoscopy may be appropriate in selected patients, outcomes may vary based on clinical severity and timing of intervention. Further studies are warranted to define optimal management strategies better.
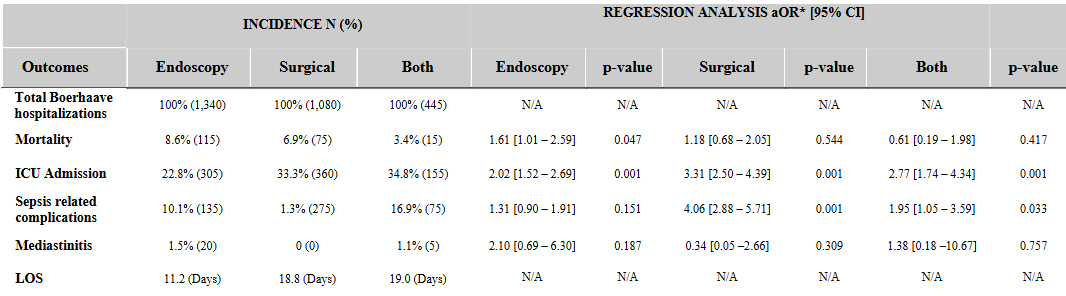
Figure: Table 1. Inpatient Outcomes and Risk-Adjusted Mortality and Complication Rates by Management Strategy for Boerhaave Syndrome
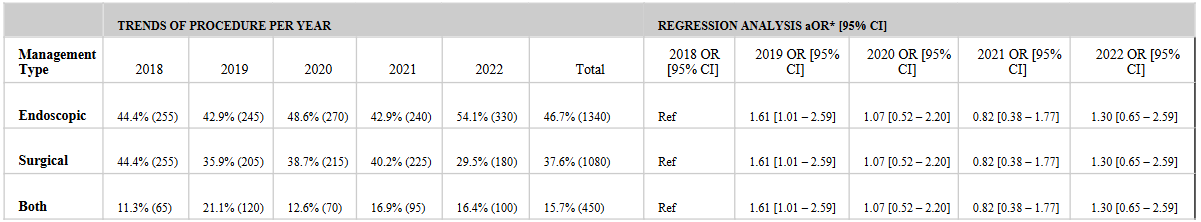
Figure: Table 2 Annual Trends in Management Strategy for Boerhaave Syndrome and Associated Risk-Adjusted Mortality
Disclosures:
Daniel Gonzalez Mosquera indicated no relevant financial relationships.
Maria Belen Mateo indicated no relevant financial relationships.
Mariana Nunes Ferreira indicated no relevant financial relationships.
Carolina Gonzalez Mosquera indicated no relevant financial relationships.
Juan Martinez-Ortega indicated no relevant financial relationships.
Yassine Kilani indicated no relevant financial relationships.
Cynthia Victor-Prophete indicated no relevant financial relationships.
Daniel Alejandro. Gonzalez Mosquera, MD1, Maria Belen Mateo, MD2, Mariana Nunes Ferreira, MD1, Carolina Gonzalez Mosquera, MD3, Juan Martinez-Ortega, MD4, Yassine Kilani, MD5, Cynthia Victor-Prophete, MD4. P2769 - Trends and Outcomes of Endoscopic vs Surgical Management of Boerhaave Syndrome: A National Inpatient Sample Analysis (2018–2022), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1NYC Health + Hospitals/Lincoln, Bronx, NY; 2Knowledge and Research Evaluation Unit, Mayo Clinic, Rochester, Minnesota, USA, Rochester, MN; 3Universidad Católica Santiago de Guayaquil, Guayaquil, Guayas, Ecuador; 4New York Health + Hospitals | Lincoln–Weill Cornell Medical College Affiliate, New York, USA, Bronx, NY; 5Saint Louis University School of Medicine, Saint Louis, MO
Introduction: Boerhaave syndrome, is a rare but life-threatening gastrointestinal emergency. Management strategies typically involve surgical repair or increasingly common endoscopic intervention. Data comparing national trends and inpatient outcomes between these approaches remain limited.
Understanding how these strategies differ in terms of mortality, complications, and resource utilization is critical for optimizing patient care.
Methods: We used the National Inpatient Sample (2018–2022) to identify adult hospitalizations with a principal diagnosis of Boerhaave syndrome (ICD-10: K22.3). Patients were stratified into endoscopic or surgical management groups using ICD-10-PCS procedure codes. Outcomes included inpatient mortality, length of stay (LOS), and complications (sepsis, mediastinitis, ICU-level care). Multivariable survey-weighted logistic and linear regressions were used to compare outcomes between groups and assess trends over time.
Results: Among 2,865 hospitalizations, 1,340 (46.8%) underwent endoscopic management, 1,080 (37.7%) surgical, and 445 (15.5%) both. Mortality was highest with endoscopic management (8.6%) compared to surgical (6.9%) and combined approaches (3.4%). Endoscopic management was associated with higher mortality odds (aOR 1.61, 95% CI: 1.01–2.59). ICU admissions were significantly more common in surgical and combined groups (p< 0.001). Surgical management showed notably higher sepsis complications (aOR 4.06, 95% CI: 2.88–5.71). Mediastinitis was rare across groups. LOS was shortest with endoscopic management (11.2 days vs. 18.8–19.0 days).
Endoscopic management increased from 44.4% in 2018 to 54.1% in 2022, while surgical interventions declined. Mortality odds did not significantly differ year-to-year.
Discussion: In this large, real-world cohort, endoscopic management of Boerhaave syndrome, though less invasive, was associated with higher inpatient mortality and lower ICU utilization compared to surgical approaches. Surgical and combined interventions demonstrated higher resource use and sepsis rates but lower mortality. These findings shows the importance of individualized treatment selection and suggest that while endoscopy may be appropriate in selected patients, outcomes may vary based on clinical severity and timing of intervention. Further studies are warranted to define optimal management strategies better.
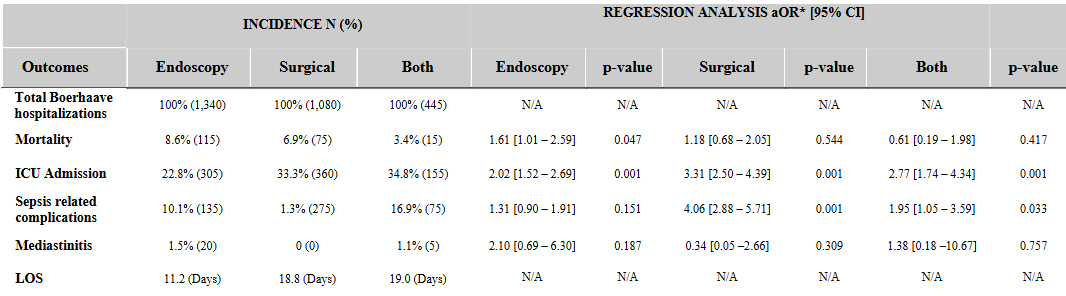
Figure: Table 1. Inpatient Outcomes and Risk-Adjusted Mortality and Complication Rates by Management Strategy for Boerhaave Syndrome
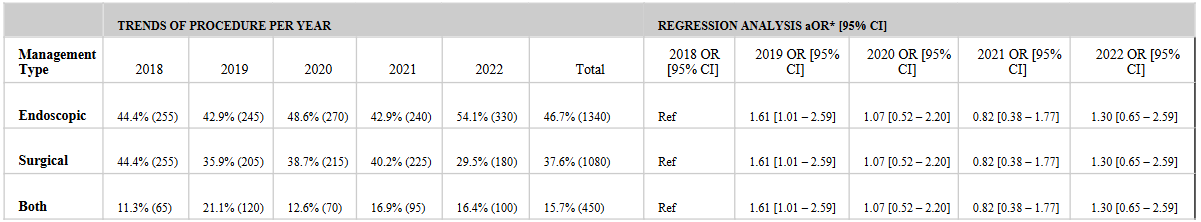
Figure: Table 2 Annual Trends in Management Strategy for Boerhaave Syndrome and Associated Risk-Adjusted Mortality
Disclosures:
Daniel Gonzalez Mosquera indicated no relevant financial relationships.
Maria Belen Mateo indicated no relevant financial relationships.
Mariana Nunes Ferreira indicated no relevant financial relationships.
Carolina Gonzalez Mosquera indicated no relevant financial relationships.
Juan Martinez-Ortega indicated no relevant financial relationships.
Yassine Kilani indicated no relevant financial relationships.
Cynthia Victor-Prophete indicated no relevant financial relationships.
Daniel Alejandro. Gonzalez Mosquera, MD1, Maria Belen Mateo, MD2, Mariana Nunes Ferreira, MD1, Carolina Gonzalez Mosquera, MD3, Juan Martinez-Ortega, MD4, Yassine Kilani, MD5, Cynthia Victor-Prophete, MD4. P2769 - Trends and Outcomes of Endoscopic vs Surgical Management of Boerhaave Syndrome: A National Inpatient Sample Analysis (2018–2022), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
