Monday Poster Session
Category: Esophagus
P2765 - A Community Center's Experience With WATS3D and the Use of Artificial Intelligence for Diagnosis and Surveillance of Barrett's Esophagus
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Rockford G. Yapp, III, MD, MPH (he/him/his)
Digestive Health Services, GI Partners of Illinois
Downers Grove, IL., IL
Presenting Author(s)
Rockford G.. Yapp, MD, MPH, Therese Loleng, MA, BA, BS
Digestive Health Services, GI Partners of Illinois, Downers Grove, IL
Introduction: Barrett's esophagus (BE), the change of stratified squamous epithelium to columnar epithelium with intestinal metaplasia in the distal esophagus, is a recognized risk factor for the majority of patients (pt) diagnosed with esophageal adenocarcinoma (EAC). Current recommendations for BE surveillance suggest an upper endoscopy (EGD) with Seattle Protocol biopsies every 3-5 years for pt with no dysplasia, shorter intervals for those with low-grade (LGD) and high-grade dysplasia (HGD) patients. Despite these guidelines, the incidence of EAC in the United States continues to increase. Traditional methods often miss areas of dysplasia due to limited sampling. This study evaluates wide-area transepithelial sampling with computer-assisted 3-dimensional analysis (WATS3D) in conjunction with standard tissue sampling for BE during EGD.
Methods: All pt of this study gave informed consent and were enrolled at the Midwest Center for Day Surgery between May 2021 to July 2024. Pt were evaluated by 4 BC gastroenterologists with extensive experience in evaluation of BE. Of the 1000 evaluated pt, 502 pt qualified and enrolled in the study (55% male, 45% female, mean age 61.3 years). All pt underwent standard Seattle Protocol surveillance of BE with four quadrant biopsies every 1-2 cm and WATS3D brushings. Biopsies were analyzed by experienced GI pathologists, and brush biopsies were sent to CDx Diagnostics’ central lab. Clinical, endoscopic, and pathological data were collected from electronic health records. The National Clinical Trial number is NCT04312633.
Results: Results showed that 30.7% of patients (154) had Non-Dysplastic Barrett’s Esophagus (NDBE) on biopsy alone, while WATS3D detected an additional 13.9% pt (70), improving diagnostic yield. WATS3D also identified 2 patients with low-grade dysplasia (LGD) and 5 patients with indefinite dysplasia, significantly increasing detection (↑ yield 100%, ↑ yield 250% respectively).
Discussion: The results of our study suggest WATS3D is an effective adjunct to standard Seattle Protocol biopsies, enhancing BE detection by 13.9% and identifying a subset of patients with advanced BE that might otherwise be missed. The use of forceps alone would have led to undetected BE, risking pt not being appropriately screened, and possibly increasing risk for EAC. While further studies are needed, this study suggests that WATS3D can significantly increase BE detection and surveillance across practice settings.
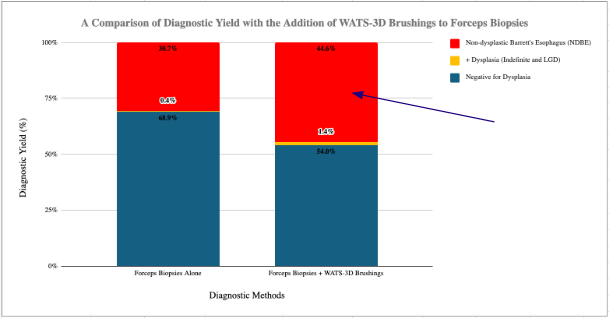
Figure: Graph 1. A comparison of diagnostic yield with the addition of WATS3D brushings to forceps biopsies.
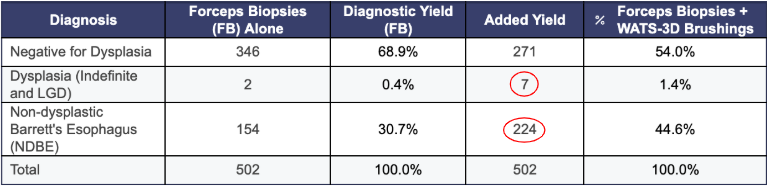
Figure: Data Table 1. Comparison of diagnostic results for both WATS3D brushings and forceps biopsies.
Disclosures:
Rockford Yapp: CDx – Grant/Research Support. Exact Science – Advisor or Review Panel Member, Grant/Research Support. Gilead – Advisory Committee/Board Member, Speakers Bureau. Ipsen – Advisory Committee/Board Member. Madigral – Advisor or Review Panel Member, Speakers Bureau.
Therese Loleng indicated no relevant financial relationships.
Rockford G.. Yapp, MD, MPH, Therese Loleng, MA, BA, BS. P2765 - A Community Center's Experience With WATS3D and the Use of Artificial Intelligence for Diagnosis and Surveillance of Barrett's Esophagus, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Digestive Health Services, GI Partners of Illinois, Downers Grove, IL
Introduction: Barrett's esophagus (BE), the change of stratified squamous epithelium to columnar epithelium with intestinal metaplasia in the distal esophagus, is a recognized risk factor for the majority of patients (pt) diagnosed with esophageal adenocarcinoma (EAC). Current recommendations for BE surveillance suggest an upper endoscopy (EGD) with Seattle Protocol biopsies every 3-5 years for pt with no dysplasia, shorter intervals for those with low-grade (LGD) and high-grade dysplasia (HGD) patients. Despite these guidelines, the incidence of EAC in the United States continues to increase. Traditional methods often miss areas of dysplasia due to limited sampling. This study evaluates wide-area transepithelial sampling with computer-assisted 3-dimensional analysis (WATS3D) in conjunction with standard tissue sampling for BE during EGD.
Methods: All pt of this study gave informed consent and were enrolled at the Midwest Center for Day Surgery between May 2021 to July 2024. Pt were evaluated by 4 BC gastroenterologists with extensive experience in evaluation of BE. Of the 1000 evaluated pt, 502 pt qualified and enrolled in the study (55% male, 45% female, mean age 61.3 years). All pt underwent standard Seattle Protocol surveillance of BE with four quadrant biopsies every 1-2 cm and WATS3D brushings. Biopsies were analyzed by experienced GI pathologists, and brush biopsies were sent to CDx Diagnostics’ central lab. Clinical, endoscopic, and pathological data were collected from electronic health records. The National Clinical Trial number is NCT04312633.
Results: Results showed that 30.7% of patients (154) had Non-Dysplastic Barrett’s Esophagus (NDBE) on biopsy alone, while WATS3D detected an additional 13.9% pt (70), improving diagnostic yield. WATS3D also identified 2 patients with low-grade dysplasia (LGD) and 5 patients with indefinite dysplasia, significantly increasing detection (↑ yield 100%, ↑ yield 250% respectively).
Discussion: The results of our study suggest WATS3D is an effective adjunct to standard Seattle Protocol biopsies, enhancing BE detection by 13.9% and identifying a subset of patients with advanced BE that might otherwise be missed. The use of forceps alone would have led to undetected BE, risking pt not being appropriately screened, and possibly increasing risk for EAC. While further studies are needed, this study suggests that WATS3D can significantly increase BE detection and surveillance across practice settings.
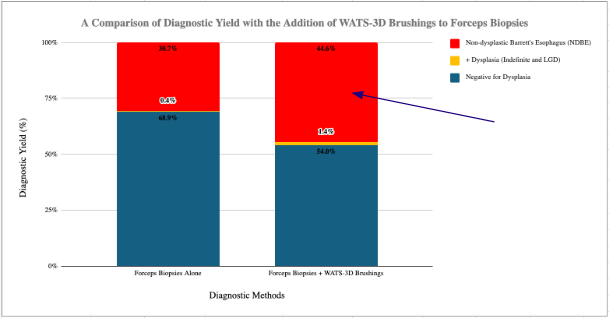
Figure: Graph 1. A comparison of diagnostic yield with the addition of WATS3D brushings to forceps biopsies.
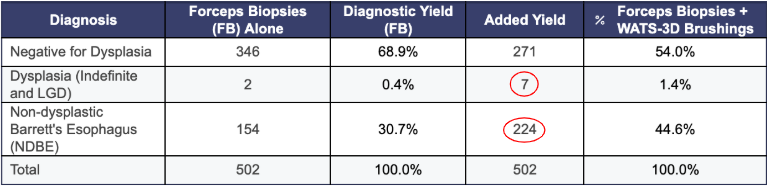
Figure: Data Table 1. Comparison of diagnostic results for both WATS3D brushings and forceps biopsies.
Disclosures:
Rockford Yapp: CDx – Grant/Research Support. Exact Science – Advisor or Review Panel Member, Grant/Research Support. Gilead – Advisory Committee/Board Member, Speakers Bureau. Ipsen – Advisory Committee/Board Member. Madigral – Advisor or Review Panel Member, Speakers Bureau.
Therese Loleng indicated no relevant financial relationships.
Rockford G.. Yapp, MD, MPH, Therese Loleng, MA, BA, BS. P2765 - A Community Center's Experience With WATS3D and the Use of Artificial Intelligence for Diagnosis and Surveillance of Barrett's Esophagus, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
