Monday Poster Session
Category: Esophagus
P2736 - Rural-Urban Disparities in Esophageal Varices Mortality in the United States -- 1999-2021
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

George S. Blewusi, MD (he/him/his)
Johns Hopkins Bloomberg School of Public Health
Baltimore, MD
Presenting Author(s)
John K. Appiah, MD1, George S. Blewusi, MD2, Richeal Asante, MD3, Emmanuel Asiedu, MD4, Emmanuel Asare, 5
1Geisinger Wyoming Valley Medical Center, Wilkes-Barre, PA; 2Johns Hopkins Bloomberg School of Public Health, Baltimore, MD; 3Geisinger Wyoming Valley Medical Center, Kingston, PA; 4Mother and Child Hospital, Accra, Central, Ghana; 5Montefiore hospital, Bronx, NY
Introduction: Esophageal varices are a life-threatening complication of portal hypertension. Despite known disparities in healthcare access, rural–urban differences in esophageal varices mortality have not been thoroughly examined at the national level. This study evaluates temporal trends and geographic disparities in U.S. mortality from esophageal varices between 1999 and 2021.
Methods: We analyzed mortality data from the CDC WONDER Multiple Cause of Death database spanning 1999 to 2021. Deaths attributed to esophageal varices (ICD-10: I85.0, I85.9) were extracted and stratified using the 2013 National Center for Health Statistics (NCHS) urban–rural classification system. Counties were categorized as urban (Large Central Metro, Large Fringe Metro, Medium Metro, and Small Metro) or rural (Micropolitan and Noncore). Crude death rates per 100,000 population were calculated annually for each geographic category.
Results: A total of 20,871 deaths from esophageal varices were identified over the 23-year period. Mortality rates increased substantially in both urban and rural areas, with rural regions experiencing disproportionately greater increases. The average rural crude death rate rose from 0.094 per 100,000 in 1999–2005 to 0.972 in 2017–2021, representing a 935% increase. Urban rates rose from 0.064 to 0.642 over the same periods, a 908% increase. By the most recent period, rural mortality rates were 1.51 times higher than urban rates. The COVID-19 pandemic revealed pronounced mortality spikes, with peak crude death rates in 2021 reaching 2.06 per 100,000 in rural areas compared to 1.36 in urban settings.
Discussion: Esophageal varices mortality has increased dramatically over the past two decades, with persistent and widening rural–urban disparities. Rural populations face significantly higher mortality risk, likely due to geographic barriers to specialized gastroenterology care, limited endoscopic capabilities in rural hospitals, and delays in emergency intervention. These findings highlight critical gaps in rural healthcare infrastructure and underscore the need for targeted efforts to improve access to specialized care for patients with portal hypertension and variceal bleeding in rural communities.
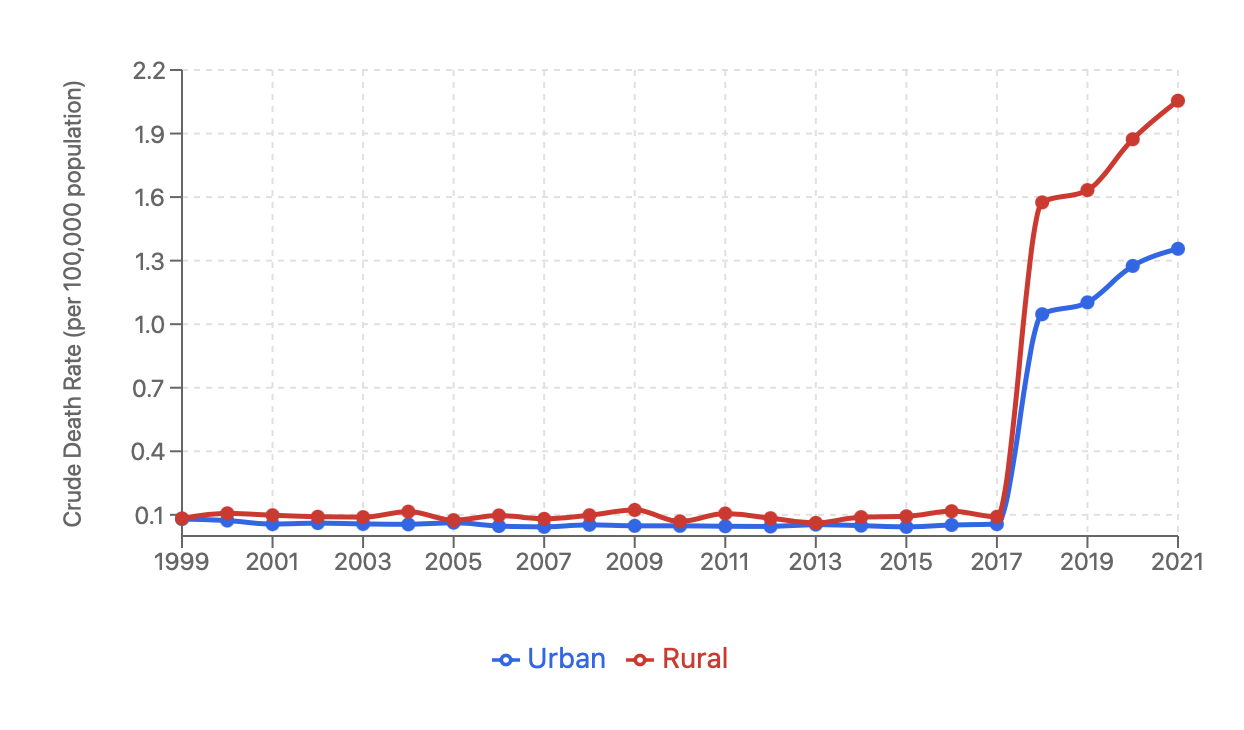
Figure: Figure 1. Crude death rates from esophageal varices by rural and urban classification in the United States, 1999–2021. Rates remained low and stable through 2017, followed by sharp increases in both settings. Rural areas experienced a steeper rise, with mortality peaking in 2021 at 2.06 per 100,000 compared to 1.36 per 100,000 in urban areas.

Figure: Table 1. Average annual crude death rates from esophageal varices (per 100,000 population) in rural and urban counties across three time periods, 1999–2021. Rural mortality increased more sharply than urban, widening the absolute mortality gap. The rural-to-urban rate ratio remained elevated throughout.
Disclosures:
John Appiah indicated no relevant financial relationships.
George Blewusi indicated no relevant financial relationships.
Richeal Asante indicated no relevant financial relationships.
Emmanuel Asiedu indicated no relevant financial relationships.
Emmanuel Asare indicated no relevant financial relationships.
John K. Appiah, MD1, George S. Blewusi, MD2, Richeal Asante, MD3, Emmanuel Asiedu, MD4, Emmanuel Asare, 5. P2736 - Rural-Urban Disparities in Esophageal Varices Mortality in the United States -- 1999-2021, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Geisinger Wyoming Valley Medical Center, Wilkes-Barre, PA; 2Johns Hopkins Bloomberg School of Public Health, Baltimore, MD; 3Geisinger Wyoming Valley Medical Center, Kingston, PA; 4Mother and Child Hospital, Accra, Central, Ghana; 5Montefiore hospital, Bronx, NY
Introduction: Esophageal varices are a life-threatening complication of portal hypertension. Despite known disparities in healthcare access, rural–urban differences in esophageal varices mortality have not been thoroughly examined at the national level. This study evaluates temporal trends and geographic disparities in U.S. mortality from esophageal varices between 1999 and 2021.
Methods: We analyzed mortality data from the CDC WONDER Multiple Cause of Death database spanning 1999 to 2021. Deaths attributed to esophageal varices (ICD-10: I85.0, I85.9) were extracted and stratified using the 2013 National Center for Health Statistics (NCHS) urban–rural classification system. Counties were categorized as urban (Large Central Metro, Large Fringe Metro, Medium Metro, and Small Metro) or rural (Micropolitan and Noncore). Crude death rates per 100,000 population were calculated annually for each geographic category.
Results: A total of 20,871 deaths from esophageal varices were identified over the 23-year period. Mortality rates increased substantially in both urban and rural areas, with rural regions experiencing disproportionately greater increases. The average rural crude death rate rose from 0.094 per 100,000 in 1999–2005 to 0.972 in 2017–2021, representing a 935% increase. Urban rates rose from 0.064 to 0.642 over the same periods, a 908% increase. By the most recent period, rural mortality rates were 1.51 times higher than urban rates. The COVID-19 pandemic revealed pronounced mortality spikes, with peak crude death rates in 2021 reaching 2.06 per 100,000 in rural areas compared to 1.36 in urban settings.
Discussion: Esophageal varices mortality has increased dramatically over the past two decades, with persistent and widening rural–urban disparities. Rural populations face significantly higher mortality risk, likely due to geographic barriers to specialized gastroenterology care, limited endoscopic capabilities in rural hospitals, and delays in emergency intervention. These findings highlight critical gaps in rural healthcare infrastructure and underscore the need for targeted efforts to improve access to specialized care for patients with portal hypertension and variceal bleeding in rural communities.
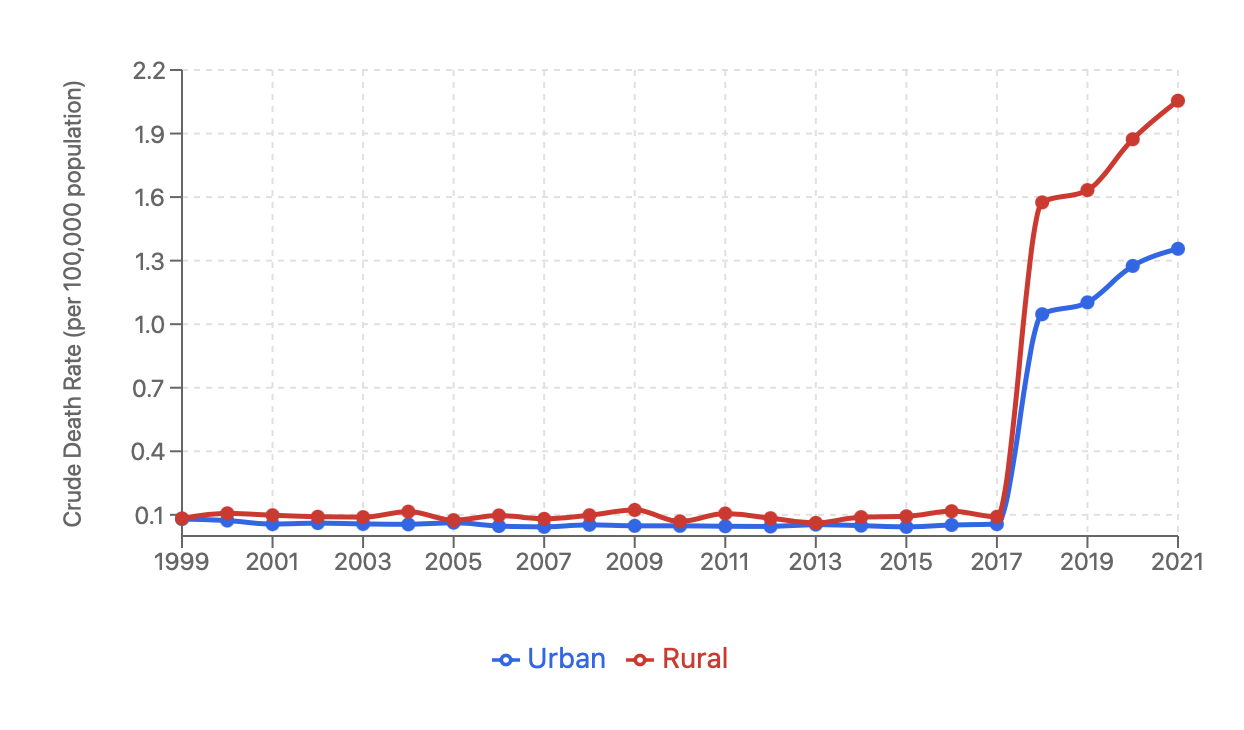
Figure: Figure 1. Crude death rates from esophageal varices by rural and urban classification in the United States, 1999–2021. Rates remained low and stable through 2017, followed by sharp increases in both settings. Rural areas experienced a steeper rise, with mortality peaking in 2021 at 2.06 per 100,000 compared to 1.36 per 100,000 in urban areas.

Figure: Table 1. Average annual crude death rates from esophageal varices (per 100,000 population) in rural and urban counties across three time periods, 1999–2021. Rural mortality increased more sharply than urban, widening the absolute mortality gap. The rural-to-urban rate ratio remained elevated throughout.
Disclosures:
John Appiah indicated no relevant financial relationships.
George Blewusi indicated no relevant financial relationships.
Richeal Asante indicated no relevant financial relationships.
Emmanuel Asiedu indicated no relevant financial relationships.
Emmanuel Asare indicated no relevant financial relationships.
John K. Appiah, MD1, George S. Blewusi, MD2, Richeal Asante, MD3, Emmanuel Asiedu, MD4, Emmanuel Asare, 5. P2736 - Rural-Urban Disparities in Esophageal Varices Mortality in the United States -- 1999-2021, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
