Monday Poster Session
Category: Esophagus
P2817 - Incidental Finding of Complete Esophageal Stricture
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Saakshi Joshi, MD (she/her/hers)
Corewell Health Farmington Hills Hospital
Farmington Hills, MI
Presenting Author(s)
Bruin Armwald, DO1, Saakshi Joshi, MD2, Joshua Steele, DO2, Mohamed Musheinesh, DO2, Olga Brushaber, DO2
1University of Wisconsin Hospitals and Clinics, Madison, WI; 2Corewell Health Farmington Hills Hospital, Farmington Hills, MI
Introduction: We present a case of external mass compression of the esophagus creating a blind pouch at the gastroesophageal (GE) junction found in a patient 8 months following EGD. Extrinsic mass compression of the esophagus is not well studied and thus there is limited epidemiological data available on this condition.
Case Description/
Methods: Our patient was a 70-year-old male with a past medical history of intracerebral hemorrhage, chronic tracheostomy and PEG tube use, and altered mentation who presented with concerns regarding fever. Initial blood cultures grew MRSA and respiratory cultures grew pseudomonas. The patient was successfully treated with antibiotics. His hospital stay was complicated by fluid leakage around his PEG tube necessitating site replacement. An EGD was performed which revealed esophageal narrowing and a blind pouch 30 cm from the incisors. Of note, the patient had an EGD 8 months prior which did not show any degree of narrowing. A neonatal scope was introduced through the PEG tube and confirmed a blind pouch above the GE junction. CT scans of the thorax showed a lesion measuring 2.8 x 3.8 cm in the subcarinal region, demonstrating extrinsic mass compression at the esophagus. Without endoscopic access, alternatives for PEG site replacement included esophageal dilation or open gastrostomy, neither of which were deemed appropriate due to the patient’s poor prognosis. As the patient’s family was not agreeable to hospice care, the existing PEG tube was replaced with one of larger size and the patient was discharged.
Discussion: Extrinsic mass compression of the esophagus was not expected in this patient as 8 months prior, the patient’s EGD revealed only GERD with esophagitis. Additionally, the patient was PEG tube dependent and unresponsive, thus the symptoms of complete stricture were not apparent. The stricture’s etiology was originally assigned to the patient’s subcarinal mass which the radiology team identified as an enlarged lymph node. This etiology was disputed, however, no other causes were identified. The patient did have a history of GERD which can contribute to esophageal stricture, although this would not explain such severe narrowing within 8 months. This case highlights extrinsic mass compression as a cause for esophageal narrowing which is not well reported on and can have a range of etiologies including mediastinal masses, vascular abnormalities, thyroid masses, and lung cancer.
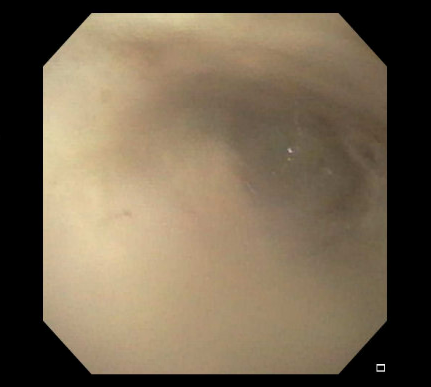
Figure: Figure 1. EGD image of esophageal stricture
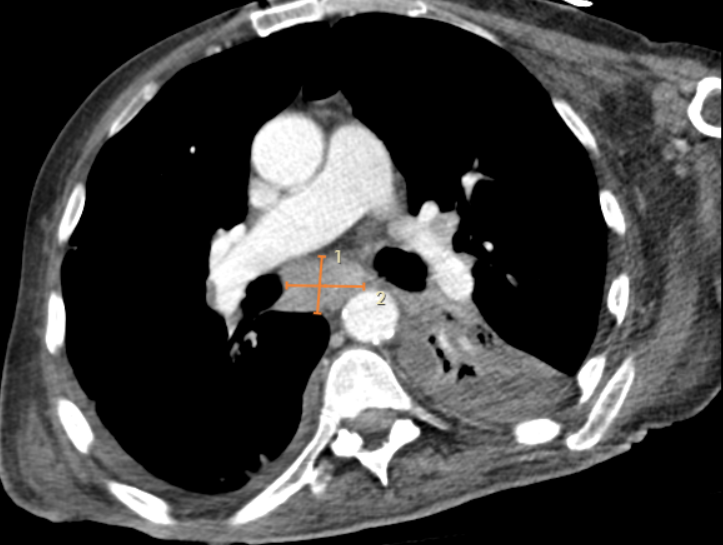
Figure: Figure 2. CT scan of subcarinal mass
Disclosures:
Bruin Armwald indicated no relevant financial relationships.
Saakshi Joshi indicated no relevant financial relationships.
Joshua Steele indicated no relevant financial relationships.
Mohamed Musheinesh indicated no relevant financial relationships.
Olga Brushaber indicated no relevant financial relationships.
Bruin Armwald, DO1, Saakshi Joshi, MD2, Joshua Steele, DO2, Mohamed Musheinesh, DO2, Olga Brushaber, DO2. P2817 - Incidental Finding of Complete Esophageal Stricture, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Wisconsin Hospitals and Clinics, Madison, WI; 2Corewell Health Farmington Hills Hospital, Farmington Hills, MI
Introduction: We present a case of external mass compression of the esophagus creating a blind pouch at the gastroesophageal (GE) junction found in a patient 8 months following EGD. Extrinsic mass compression of the esophagus is not well studied and thus there is limited epidemiological data available on this condition.
Case Description/
Methods: Our patient was a 70-year-old male with a past medical history of intracerebral hemorrhage, chronic tracheostomy and PEG tube use, and altered mentation who presented with concerns regarding fever. Initial blood cultures grew MRSA and respiratory cultures grew pseudomonas. The patient was successfully treated with antibiotics. His hospital stay was complicated by fluid leakage around his PEG tube necessitating site replacement. An EGD was performed which revealed esophageal narrowing and a blind pouch 30 cm from the incisors. Of note, the patient had an EGD 8 months prior which did not show any degree of narrowing. A neonatal scope was introduced through the PEG tube and confirmed a blind pouch above the GE junction. CT scans of the thorax showed a lesion measuring 2.8 x 3.8 cm in the subcarinal region, demonstrating extrinsic mass compression at the esophagus. Without endoscopic access, alternatives for PEG site replacement included esophageal dilation or open gastrostomy, neither of which were deemed appropriate due to the patient’s poor prognosis. As the patient’s family was not agreeable to hospice care, the existing PEG tube was replaced with one of larger size and the patient was discharged.
Discussion: Extrinsic mass compression of the esophagus was not expected in this patient as 8 months prior, the patient’s EGD revealed only GERD with esophagitis. Additionally, the patient was PEG tube dependent and unresponsive, thus the symptoms of complete stricture were not apparent. The stricture’s etiology was originally assigned to the patient’s subcarinal mass which the radiology team identified as an enlarged lymph node. This etiology was disputed, however, no other causes were identified. The patient did have a history of GERD which can contribute to esophageal stricture, although this would not explain such severe narrowing within 8 months. This case highlights extrinsic mass compression as a cause for esophageal narrowing which is not well reported on and can have a range of etiologies including mediastinal masses, vascular abnormalities, thyroid masses, and lung cancer.
Figure: Figure 1. EGD image of esophageal stricture
Figure: Figure 2. CT scan of subcarinal mass
Disclosures:
Bruin Armwald indicated no relevant financial relationships.
Saakshi Joshi indicated no relevant financial relationships.
Joshua Steele indicated no relevant financial relationships.
Mohamed Musheinesh indicated no relevant financial relationships.
Olga Brushaber indicated no relevant financial relationships.
Bruin Armwald, DO1, Saakshi Joshi, MD2, Joshua Steele, DO2, Mohamed Musheinesh, DO2, Olga Brushaber, DO2. P2817 - Incidental Finding of Complete Esophageal Stricture, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
