Monday Poster Session
Category: Esophagus
P2809 - Insights Into Esophageal Cancer: Incidence and Survival Rates - A Twenty-Year Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Silpa Choday, MD (she/her/hers)
Creighton University School of Medicine
Phoenix, AZ
Presenting Author(s)
Silpa Choday, MD1, Varun Vankesvaram, MD2, Laura Cicani, MD3, Akanksha Togra, MD4, Ramandeep Sandhu, MD1, Keng-Yu Chuang, MD5, Wael Youssef, MD1, Dalbir Sandhu, MD1
1Creighton University School of Medicine, Phoenix, AZ; 2Rwjbh Community Medical Center, Toms River, NJ; 3International University of Health Sciences, Las Vegas, NV; 4Texas Tech University Health Sciences Center, El Paso, TX; 5GI Alliance, Phoenix, AZ
Introduction: Esophageal cancer (EC) is a significant global health concern, with high mortality rates. This study aims to analyze trends in EC using Surveillance, Epidemiology, and End Results (SEER) data.
Methods: Data from the SEER database (1992–2021) were analyzed to determine age-adjusted incidence and survival rates of EC. Temporal trends were evaluated using Joinpoint log-linear regression to estimate average annual percent changes (APC). Poisson regression models were employed to compute incidence and mortality rate ratios (IRRs and MRRs).
Results: The incidence of EC is significantly higher in males compared to females (4.1 vs. 0.9 per 100,000). Non-Hispanic Whites (NHW) had the highest incidence rates while the non-Hispanic Asian (NHA)/Pacific Islanders (PI) had the lowest (2.7 vs 1.5 per 100,000). Mortality patterns mirrored incidence trends: males experienced higher mortality rates than females (3.4 vs. 0.7 per 100,000).
Longitudinal analysis revealed a significant decline in EC incidence with a greater reduction among males (APC = -1.14; p < 0.001). Among racial/ethnic groups, non-Hispanic Blacks (NHB) experienced the steepest decline in incidence (APC = -3.27; p < 0.001). Stratification by stage at diagnosis showed that patients with localized disease demonstrated a significant decrease in incidence, with rates dropping from 1% to 0.75% over time (APC [95% CI] = -2.29 [-3.73, -1.11]; p = 0.002). Cancer diagnosed at a distant stage has a 4.5-fold higher incidence compared to the in-situ cases. Males were more likely than females to be diagnosed at regional and distant stages (p < 0.001).
Age was a critical determinant of both incidence and mortality. Individuals aged 40–49 had a 5-fold increase in incidence relative to those under 20, and this increased to 16-fold among those aged 50 or older (p < 0.001). Mortality trends followed a similar pattern, compared to individuals under 20, those aged 40–49 had a 3.5-fold increase in mortality, which rose to an 11-fold increase for patients aged 50 years and older (p < 0.001). Across all age categories, females consistently exhibited a 68% reduction in both incidence and mortality compared to males (p < 0.001).
Discussion: EC incidence and mortality are significantly higher among males and increase sharply with age, particularly after 50 years. NHW exhibits the highest incidence rates, while NHA/PI have the lowest. Over time, incidence has declined, most notably among males and NHB. Advanced stage at diagnosis remains more common in males.
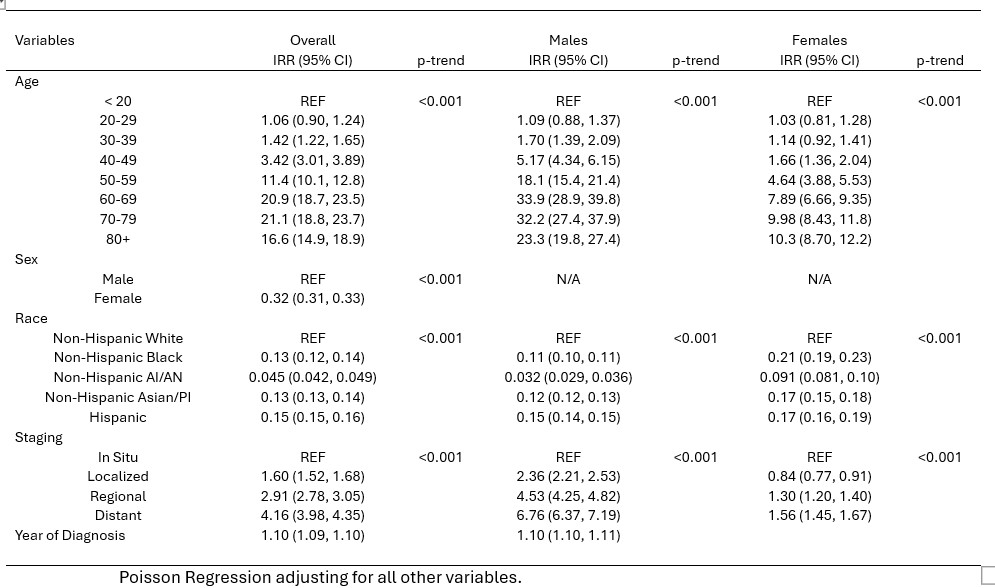
Figure: Table 1. Incidence Rate Ratios to associate the rate of Esophageal Cancer mortality with age, sex, race and stage at diagnosis.
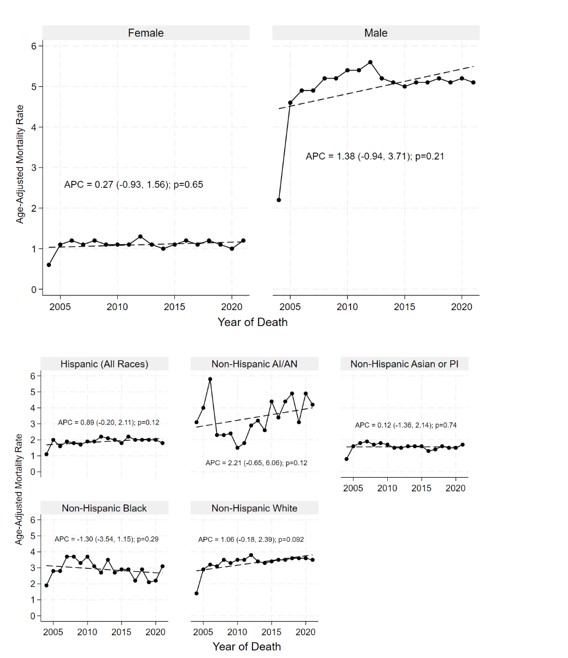
Figure: Figure 1. Annual Percent Change in Age-Adjusted Mortality Rates of Esophageal Cancer by Sex, Race/Ethnicity and Stage at Diagnosis.
Disclosures:
Silpa Choday indicated no relevant financial relationships.
Varun Vankesvaram indicated no relevant financial relationships.
Laura Cicani indicated no relevant financial relationships.
Akanksha Togra indicated no relevant financial relationships.
Ramandeep Sandhu indicated no relevant financial relationships.
Keng-Yu Chuang indicated no relevant financial relationships.
Wael Youssef indicated no relevant financial relationships.
Dalbir Sandhu indicated no relevant financial relationships.
Silpa Choday, MD1, Varun Vankesvaram, MD2, Laura Cicani, MD3, Akanksha Togra, MD4, Ramandeep Sandhu, MD1, Keng-Yu Chuang, MD5, Wael Youssef, MD1, Dalbir Sandhu, MD1. P2809 - Insights Into Esophageal Cancer: Incidence and Survival Rates - A Twenty-Year Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Creighton University School of Medicine, Phoenix, AZ; 2Rwjbh Community Medical Center, Toms River, NJ; 3International University of Health Sciences, Las Vegas, NV; 4Texas Tech University Health Sciences Center, El Paso, TX; 5GI Alliance, Phoenix, AZ
Introduction: Esophageal cancer (EC) is a significant global health concern, with high mortality rates. This study aims to analyze trends in EC using Surveillance, Epidemiology, and End Results (SEER) data.
Methods: Data from the SEER database (1992–2021) were analyzed to determine age-adjusted incidence and survival rates of EC. Temporal trends were evaluated using Joinpoint log-linear regression to estimate average annual percent changes (APC). Poisson regression models were employed to compute incidence and mortality rate ratios (IRRs and MRRs).
Results: The incidence of EC is significantly higher in males compared to females (4.1 vs. 0.9 per 100,000). Non-Hispanic Whites (NHW) had the highest incidence rates while the non-Hispanic Asian (NHA)/Pacific Islanders (PI) had the lowest (2.7 vs 1.5 per 100,000). Mortality patterns mirrored incidence trends: males experienced higher mortality rates than females (3.4 vs. 0.7 per 100,000).
Longitudinal analysis revealed a significant decline in EC incidence with a greater reduction among males (APC = -1.14; p < 0.001). Among racial/ethnic groups, non-Hispanic Blacks (NHB) experienced the steepest decline in incidence (APC = -3.27; p < 0.001). Stratification by stage at diagnosis showed that patients with localized disease demonstrated a significant decrease in incidence, with rates dropping from 1% to 0.75% over time (APC [95% CI] = -2.29 [-3.73, -1.11]; p = 0.002). Cancer diagnosed at a distant stage has a 4.5-fold higher incidence compared to the in-situ cases. Males were more likely than females to be diagnosed at regional and distant stages (p < 0.001).
Age was a critical determinant of both incidence and mortality. Individuals aged 40–49 had a 5-fold increase in incidence relative to those under 20, and this increased to 16-fold among those aged 50 or older (p < 0.001). Mortality trends followed a similar pattern, compared to individuals under 20, those aged 40–49 had a 3.5-fold increase in mortality, which rose to an 11-fold increase for patients aged 50 years and older (p < 0.001). Across all age categories, females consistently exhibited a 68% reduction in both incidence and mortality compared to males (p < 0.001).
Discussion: EC incidence and mortality are significantly higher among males and increase sharply with age, particularly after 50 years. NHW exhibits the highest incidence rates, while NHA/PI have the lowest. Over time, incidence has declined, most notably among males and NHB. Advanced stage at diagnosis remains more common in males.
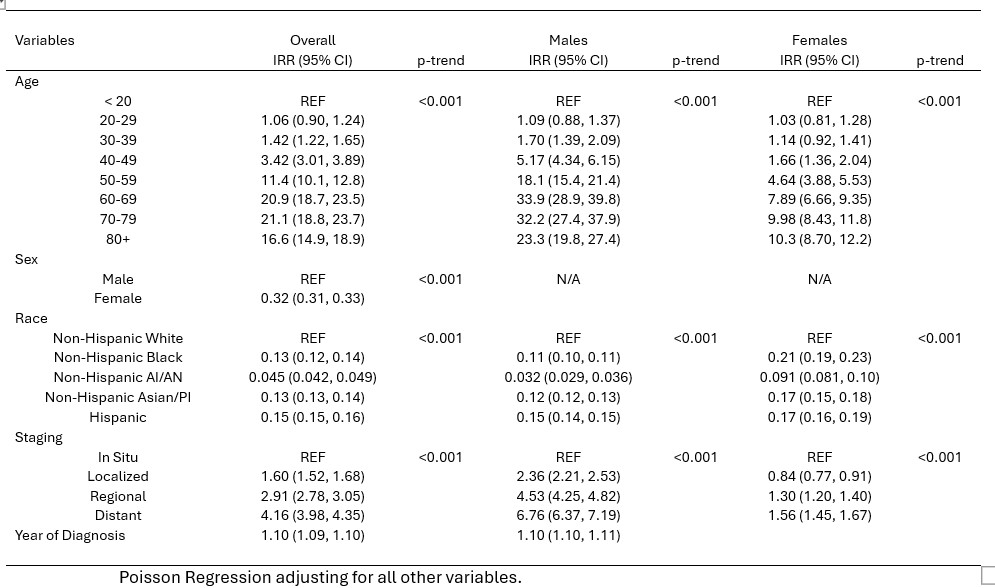
Figure: Table 1. Incidence Rate Ratios to associate the rate of Esophageal Cancer mortality with age, sex, race and stage at diagnosis.
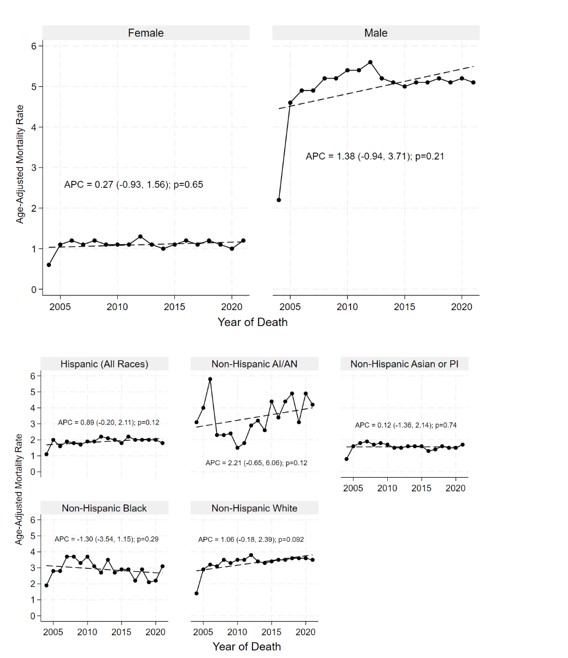
Figure: Figure 1. Annual Percent Change in Age-Adjusted Mortality Rates of Esophageal Cancer by Sex, Race/Ethnicity and Stage at Diagnosis.
Disclosures:
Silpa Choday indicated no relevant financial relationships.
Varun Vankesvaram indicated no relevant financial relationships.
Laura Cicani indicated no relevant financial relationships.
Akanksha Togra indicated no relevant financial relationships.
Ramandeep Sandhu indicated no relevant financial relationships.
Keng-Yu Chuang indicated no relevant financial relationships.
Wael Youssef indicated no relevant financial relationships.
Dalbir Sandhu indicated no relevant financial relationships.
Silpa Choday, MD1, Varun Vankesvaram, MD2, Laura Cicani, MD3, Akanksha Togra, MD4, Ramandeep Sandhu, MD1, Keng-Yu Chuang, MD5, Wael Youssef, MD1, Dalbir Sandhu, MD1. P2809 - Insights Into Esophageal Cancer: Incidence and Survival Rates - A Twenty-Year Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
