Monday Poster Session
Category: Diet, Nutrition, and Obesity
P2681 - Impact of BMI on Clinical Outcomes Following Acute Diverticulitis in the Elderly Population: Does Weight Matter? A Nationwide Perspective
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Iqra Arshad, MD, MPH (she/her/hers)
SSM Health Saint Louis University Hospital
Saint Louis, MO
Presenting Author(s)
Iqra Arshad, MD, MPH1, Umar Hayat, MD2, Mahmoud Y. Madi, MD3, Adam D. Farmer, MD, PhD1
1SSM Health Saint Louis University Hospital, Saint Louis, MO; 2Geisinger Wyoming Valley Medical Center, Wilkes-Barre, PA; 3University of Texas at Austin Dell Medical School, Austin, TX
Introduction: Diverticular disease (DD) affects approximately 65% of adults aged ≥65 years and is a leading cause of gastrointestinal-related hospitalizations. Obesity is a known risk factor for DD, but its impact on clinical and surgical outcomes in elderly adults remains unexplored. This study evaluates the association between body mass index (BMI) and outcomes in elderly patients hospitalized with acute diverticulitis (AD) using a national dataset.
Methods: Using ICD-10-CM codes from the National Inpatient Sample (2016–2020), we identified 132,900 hospitalizations of patients aged ≥65 years admitted with AD. Patients were stratified by BMI: overweight (BMI 25–< 30 kg/m², reference group), Class 1–2 obesity (BMI 30–< 40 kg/m²), and Class 3 obesity (BMI ≥40 kg/m²). The primary outcome was in-hospital mortality. Secondary outcomes included AD complications (e.g., diverticular bleeding, abscess), surgical interventions (e.g., colectomy, colostomy, abscess drainage), acute kidney injury (AKI), sepsis, ventilator support, delirium, length of stay (LOS), and hospitalization costs. Outcomes were analyzed using multivariate logistic regression. Results are reported as adjusted odds ratios (aOR) with 95% confidence intervals (CI).
Results: On multivariate analysis, class 3 obesity was associated with a trend towards higher odds of in-hospital mortality (aOR 1.66, 95% CI: 0.90–3.06; p=0.10) compared to the reference group. Compared to the overweight group, both obese groups had lower odds of surgical interventions: colectomy (Class 1–2: aOR 0.70, 95% CI: 0.61–0.80, p< 0.001; Class 3: aOR 0.46, 95% CI: 0.38–0.54, p< 0.001), colostomy (Class 1–2: aOR 0.55, 95% CI: 0.46–0.66, p< 0.001; Class 3: aOR 0.47, 95% CI: 0.38–0.59, p< 0.001), and abscess drainage (Class 3: aOR 0.50, 95% CI: 0.27–0.93, p=0.03). Class 3 obesity was associated with increased odds of AKI (aOR 1.22, 95% CI: 1.05–1.40, p=0.007). Healthcare utilization was higher in the Class 1–2 obesity group, with increased LOS (adjusted mean difference: 1.47 days, 95% CI: 1.18–1.70, p< 0.001) and total charges ($17,848, 95% CI: $13,901–$21,795, p< 0.001) compared to the reference group.
Discussion: This study suggests that higher BMI increases AD complications and AKI and conversely reduces odds of surgical interventions, LOS and healthcare costs among elderly. Given the limitations of retrospective data, prospective studies are needed to confirm these findings and make admission risk stratification strategies for elderly patients presenting with AD.
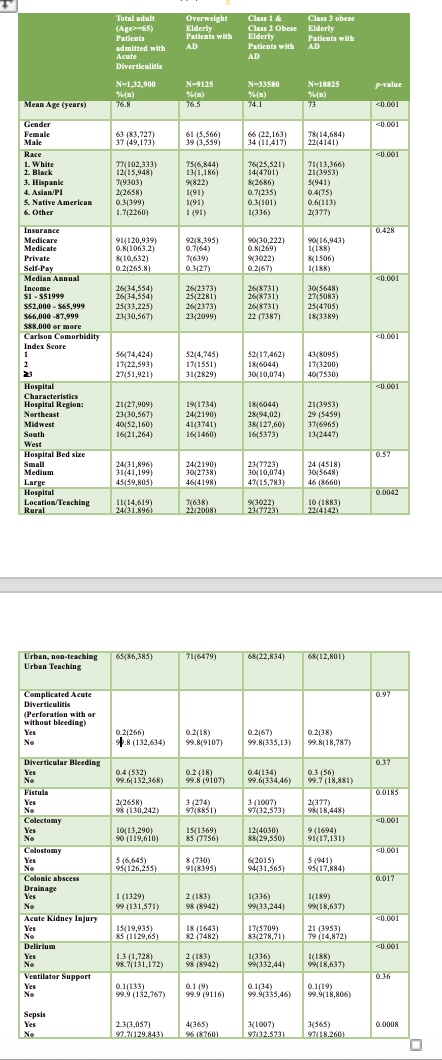
Figure: Table 1. Baseline characteristics of the study population, stratified based on BMI.
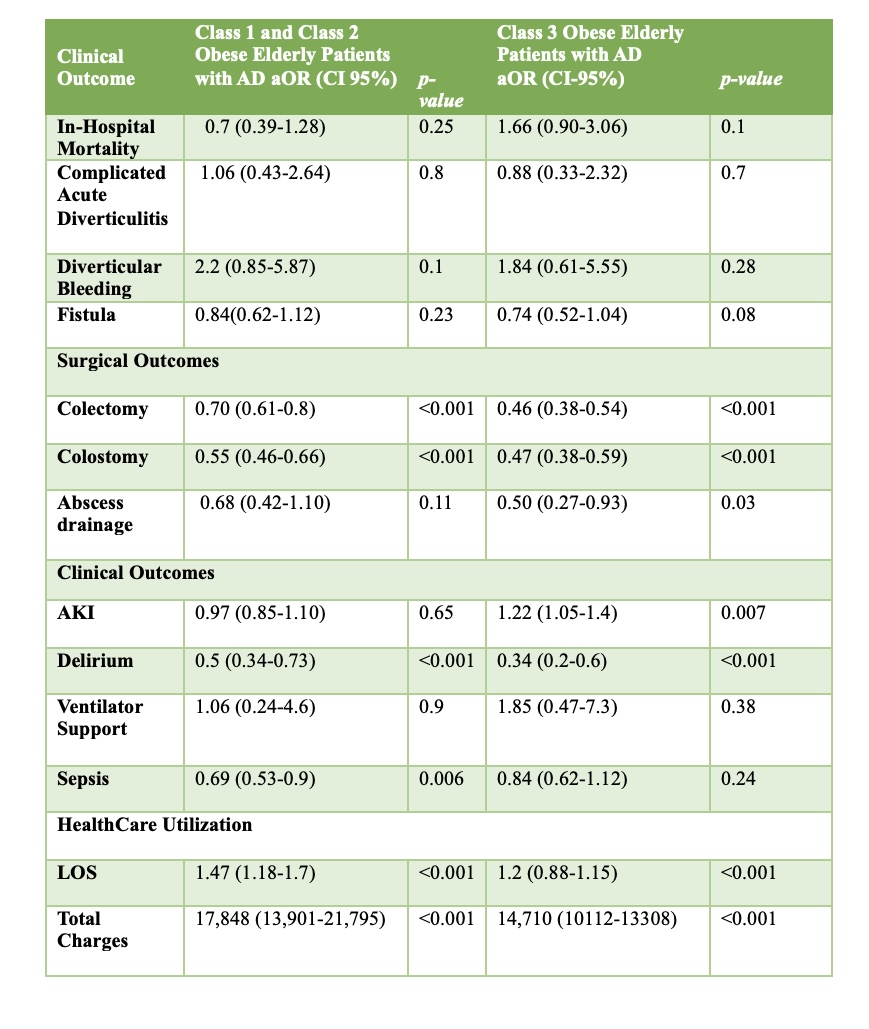
Figure: Table 2: Adjusted Clinical and Surgical Outcomes amongst Class 1-2 Obese and Class 3 Obese Elderly Patients with AD Compared to the Overweight Reference Group.
Disclosures:
Iqra Arshad indicated no relevant financial relationships.
Umar Hayat indicated no relevant financial relationships.
Mahmoud Madi indicated no relevant financial relationships.
Adam D. Farmer indicated no relevant financial relationships.
Iqra Arshad, MD, MPH1, Umar Hayat, MD2, Mahmoud Y. Madi, MD3, Adam D. Farmer, MD, PhD1. P2681 - Impact of BMI on Clinical Outcomes Following Acute Diverticulitis in the Elderly Population: Does Weight Matter? A Nationwide Perspective, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1SSM Health Saint Louis University Hospital, Saint Louis, MO; 2Geisinger Wyoming Valley Medical Center, Wilkes-Barre, PA; 3University of Texas at Austin Dell Medical School, Austin, TX
Introduction: Diverticular disease (DD) affects approximately 65% of adults aged ≥65 years and is a leading cause of gastrointestinal-related hospitalizations. Obesity is a known risk factor for DD, but its impact on clinical and surgical outcomes in elderly adults remains unexplored. This study evaluates the association between body mass index (BMI) and outcomes in elderly patients hospitalized with acute diverticulitis (AD) using a national dataset.
Methods: Using ICD-10-CM codes from the National Inpatient Sample (2016–2020), we identified 132,900 hospitalizations of patients aged ≥65 years admitted with AD. Patients were stratified by BMI: overweight (BMI 25–< 30 kg/m², reference group), Class 1–2 obesity (BMI 30–< 40 kg/m²), and Class 3 obesity (BMI ≥40 kg/m²). The primary outcome was in-hospital mortality. Secondary outcomes included AD complications (e.g., diverticular bleeding, abscess), surgical interventions (e.g., colectomy, colostomy, abscess drainage), acute kidney injury (AKI), sepsis, ventilator support, delirium, length of stay (LOS), and hospitalization costs. Outcomes were analyzed using multivariate logistic regression. Results are reported as adjusted odds ratios (aOR) with 95% confidence intervals (CI).
Results: On multivariate analysis, class 3 obesity was associated with a trend towards higher odds of in-hospital mortality (aOR 1.66, 95% CI: 0.90–3.06; p=0.10) compared to the reference group. Compared to the overweight group, both obese groups had lower odds of surgical interventions: colectomy (Class 1–2: aOR 0.70, 95% CI: 0.61–0.80, p< 0.001; Class 3: aOR 0.46, 95% CI: 0.38–0.54, p< 0.001), colostomy (Class 1–2: aOR 0.55, 95% CI: 0.46–0.66, p< 0.001; Class 3: aOR 0.47, 95% CI: 0.38–0.59, p< 0.001), and abscess drainage (Class 3: aOR 0.50, 95% CI: 0.27–0.93, p=0.03). Class 3 obesity was associated with increased odds of AKI (aOR 1.22, 95% CI: 1.05–1.40, p=0.007). Healthcare utilization was higher in the Class 1–2 obesity group, with increased LOS (adjusted mean difference: 1.47 days, 95% CI: 1.18–1.70, p< 0.001) and total charges ($17,848, 95% CI: $13,901–$21,795, p< 0.001) compared to the reference group.
Discussion: This study suggests that higher BMI increases AD complications and AKI and conversely reduces odds of surgical interventions, LOS and healthcare costs among elderly. Given the limitations of retrospective data, prospective studies are needed to confirm these findings and make admission risk stratification strategies for elderly patients presenting with AD.
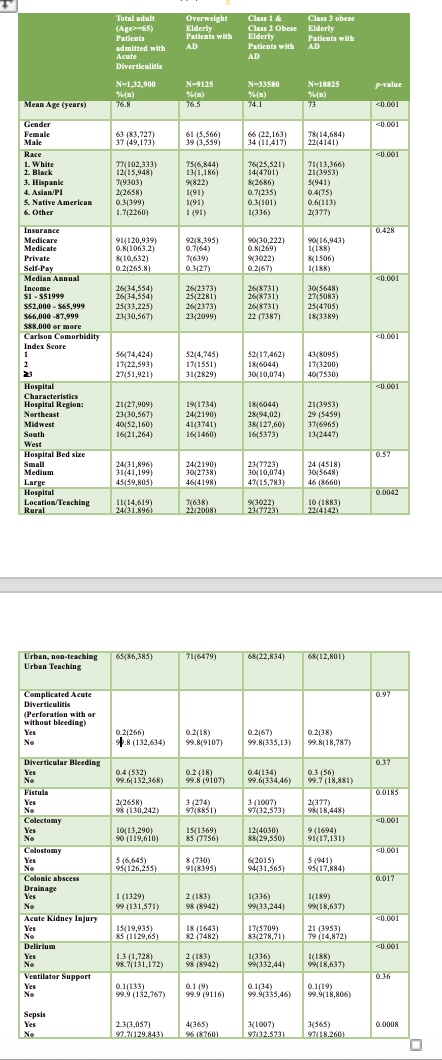
Figure: Table 1. Baseline characteristics of the study population, stratified based on BMI.
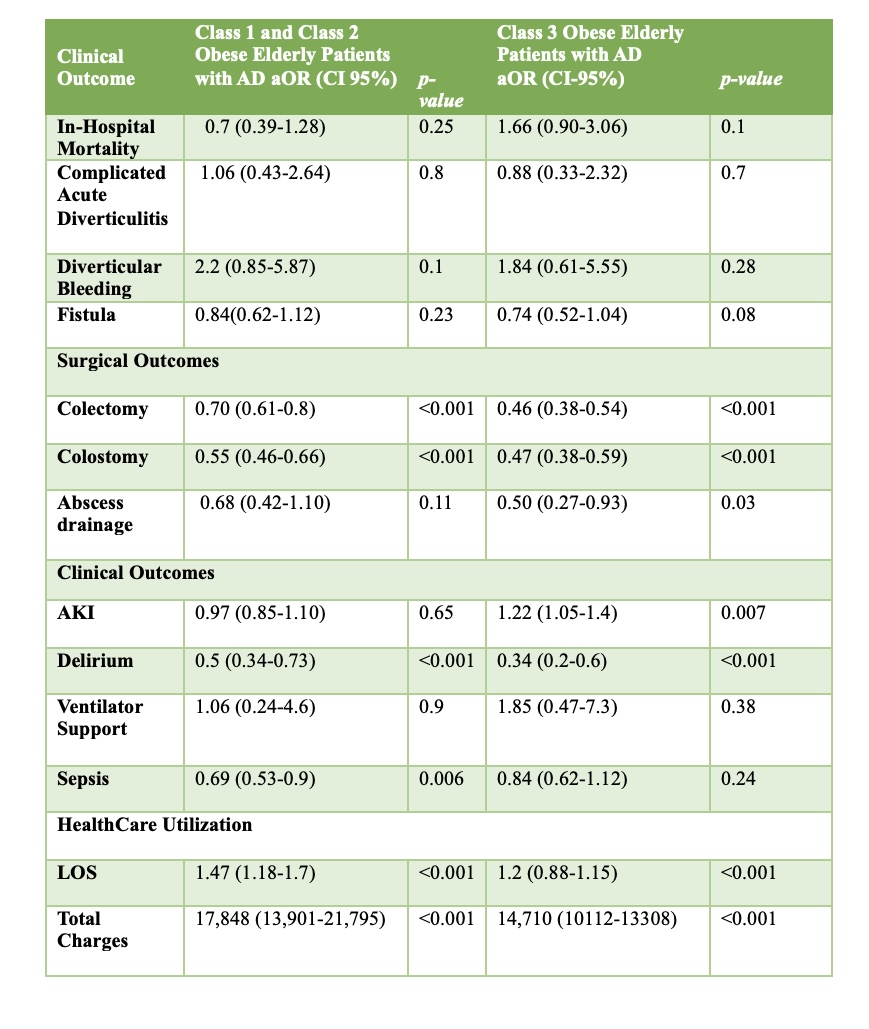
Figure: Table 2: Adjusted Clinical and Surgical Outcomes amongst Class 1-2 Obese and Class 3 Obese Elderly Patients with AD Compared to the Overweight Reference Group.
Disclosures:
Iqra Arshad indicated no relevant financial relationships.
Umar Hayat indicated no relevant financial relationships.
Mahmoud Madi indicated no relevant financial relationships.
Adam D. Farmer indicated no relevant financial relationships.
Iqra Arshad, MD, MPH1, Umar Hayat, MD2, Mahmoud Y. Madi, MD3, Adam D. Farmer, MD, PhD1. P2681 - Impact of BMI on Clinical Outcomes Following Acute Diverticulitis in the Elderly Population: Does Weight Matter? A Nationwide Perspective, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
