Monday Poster Session
Category: Colorectal Cancer Prevention
P2652 - A Dual Diagnosis, a Double Burden: Racial and Ethnic Disparities in Colorectal Cancer and Cardiovascular Diseases-Related Hospital Outcomes
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Taha Bin Arif, MBBS, MD (he/him/his)
Sinai Hospital of Baltimore, The George Washington University Regional Medical Campus
Baltimore, MD
Presenting Author(s)
Taha Bin Arif, MBBS, MD1, Muhammad Talha Maniya, MBBS2, Ali Salman, MBBS3, Umm E. Salma Shabbar Banatwala, MBBS3, Sana Murtaza, MBBS, MD4, Sara Ahmad, MBBS5, Sara Aleem, MBBS6, Sanish Abbasi, MBBS7, Fatima Naveed, MBBS8, Kashif Ali, MD9, Muhammad Hamza Shafiq, MBBS10, Sheheryar Ibrahim, MBBS2, Muhammad Tayyab Ijaz, MBBS11, Amina Arif, MBBS12, Misbah Bibi, MBBS13
1Sinai Hospital of Baltimore, The George Washington University Regional Medical Campus, Baltimore, MD; 2Ziauddin University, Karachi, Sindh, Pakistan; 3Dow University of Health Sciences, Karachi, Sindh, Pakistan; 4Punjab Medical College, Faisalabad, Punjab, Pakistan; 5University Medical and Dental College, Faisalabad, Punjab, Pakistan; 6Sialkot Medical College, Sialkot, Punjab, Pakistan; 7Peoples University of Medical and Health Sciences, Nawabshah, Sindh, Pakistan; 8Rawal Institute of Health Sciences, Islamabad, Punjab, Pakistan; 9University of Texas Rio Grande Valley, Edinburg, TX; 10Bolan Medical College, Quetta, Balochistan, Pakistan; 11CMH Lahore Medical College, Lahore, Punjab, Pakistan; 12Sharif Medical and Dental College, Narowal, Punjab, Pakistan; 13Bahria University Health Sciences Campus, Karachi, Sindh, Pakistan
Introduction: Cardiovascular disease (CVD) and colorectal cancer (CRC) are major contributors to morbidity and mortality in the United States, with evidence suggesting disproportionately adverse outcomes among racial and ethnic minorities. However, limited national data exist on how race and ethnicity influence the cardiovascular burden and related in-hospital outcomes in patients with CRC. We evaluated racial disparities in in-hospital mortality, length of stay (LOS), and healthcare costs among patients hospitalized with concurrent CRC and CVD.
Methods: A retrospective cross-sectional analysis of the National Inpatient Sample from 2018 to 2020 was conducted, identifying 232,720 adult hospitalizations with a primary diagnosis of CRC and a secondary diagnosis of at least one CVD, defined as myocardial infarction, dysrhythmia, coronary artery disease, heart failure, hypertension, or stroke. Multivariable logistic and linear regression models were used to evaluate the association between race/ethnicity and in-hospital outcomes, including mortality, LOS, and total hospitalization costs, adjusting for patient demographics, clinical comorbidities, and hospital characteristics.
Results: Among the 232,720 hospitalizations analyzed, 71.7% of patients were identified as White, 13.7% as Black, 8.3% as Hispanic, 3.3% as Asian/Pacific Islander, and 3.0% as Other. Black patients exhibited significantly higher in-hospital mortality (OR: 1.33; 95% CI: 1.12–1.58; p = 0.001), extended LOS (β = 0.97 days; 95% CI: 0.74–1.20; p < 0.001), and elevated costs (β = $4,695; 95% CI: $1,424–$7,966; p = 0.005) than Whites with CVD and CRC. Hispanics experienced the highest inflation-adjusted hospital charges (β = $20,281; 95% CI: $14,787–$25,776; p < 0.001) alongside a moderately prolonged LOS (β = 0.37 days; 95% CI: 0.10–0.64; p = 0.006). Asians were disproportionately affected by rectal cancers (22%), while their Black and Hispanic counterparts demonstrated higher rates of anus and anal canal cancers (2.6% and 2.5%, respectively). Metastatic disease prevalence was greatest amongst the Black (40%) and Asian (35%) population.
Discussion: Racial disparities in in-hospital outcomes among patients with concurrent colorectal cancer and cardiovascular disease are pronounced. Black and Hispanic patients experience significantly higher mortality, longer hospital stays, and greater healthcare costs compared to Whites. These findings highlight an urgent need for equity-focused strategies to address these structural and clinical inequities.
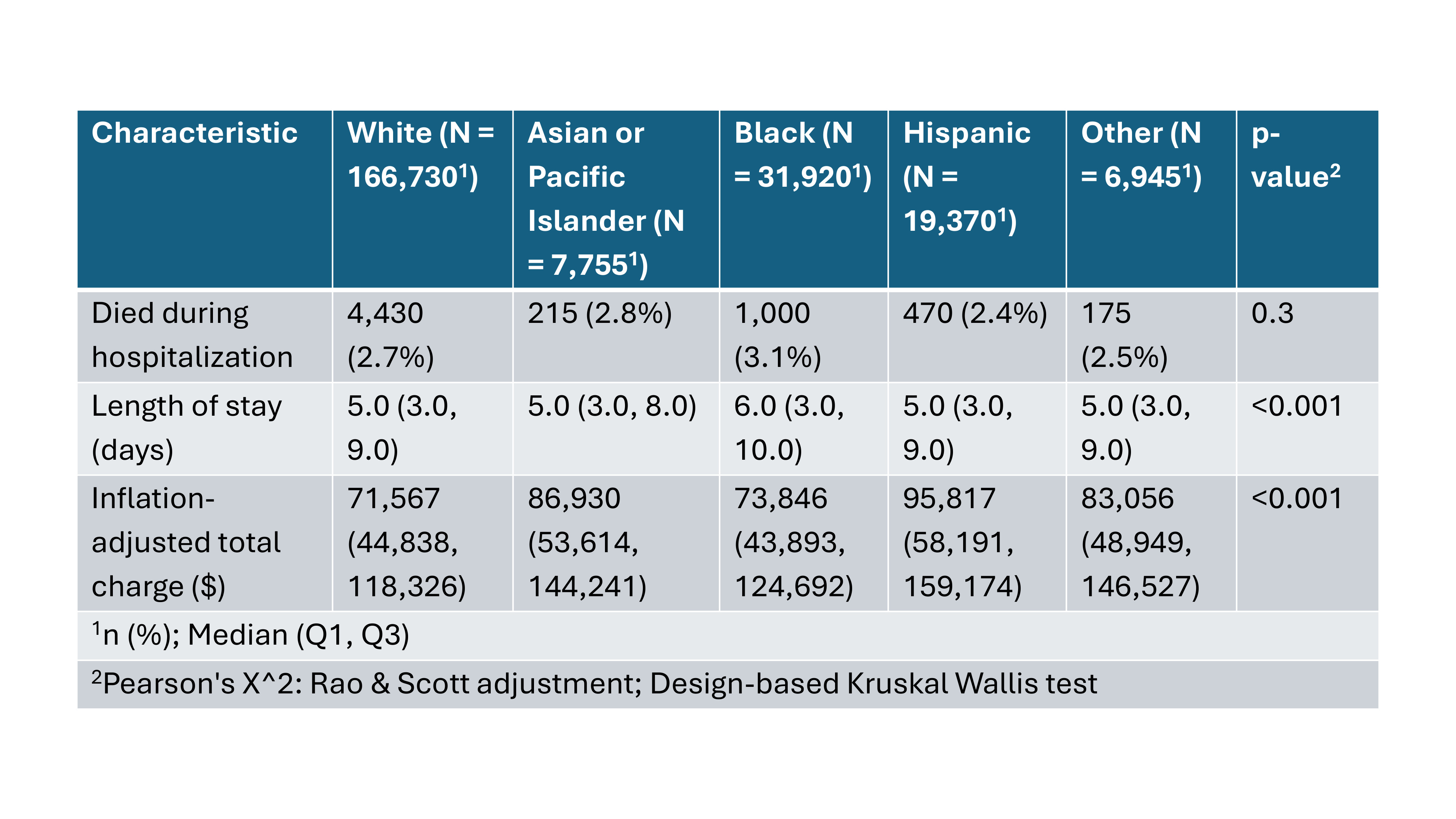
Figure: Figure 1: Hospitalization Outcomes by Racial and Ethnic Groups: Mortality, Length of Stay, and Total Charges.
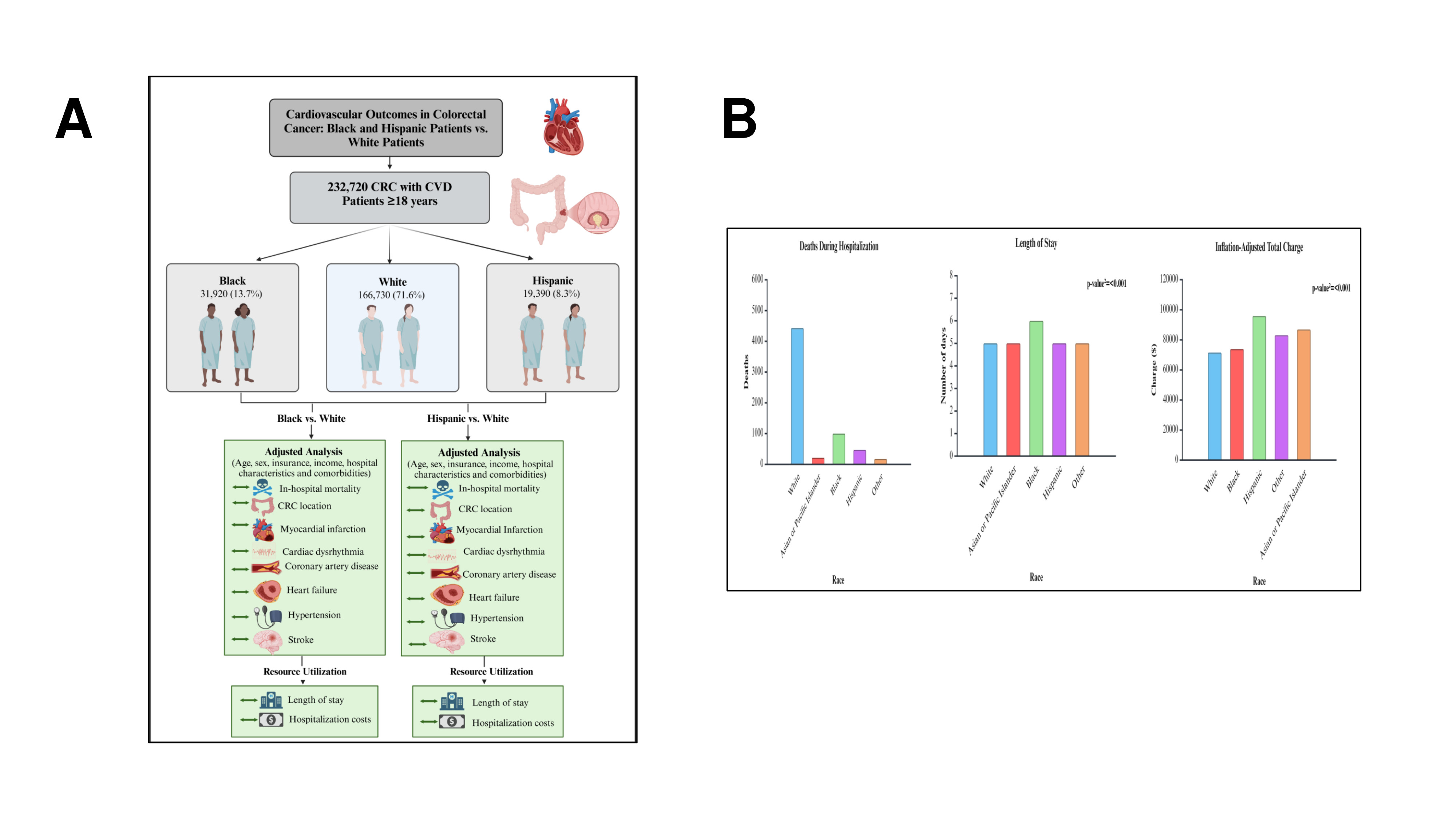
Figure: Figure 2A: Graphical Abstract; 2B: Bar graphs of deaths during hospitalization, length of stay, and inflation-adjusted total charges among different races.
Disclosures:
Taha Bin Arif indicated no relevant financial relationships.
Muhammad Talha Maniya indicated no relevant financial relationships.
Ali Salman indicated no relevant financial relationships.
Umm E. Salma Shabbar Banatwala indicated no relevant financial relationships.
Sana Murtaza indicated no relevant financial relationships.
Sara Ahmad indicated no relevant financial relationships.
Sara Aleem indicated no relevant financial relationships.
Sanish Abbasi indicated no relevant financial relationships.
Fatima Naveed indicated no relevant financial relationships.
Kashif Ali indicated no relevant financial relationships.
Muhammad Hamza Shafiq indicated no relevant financial relationships.
Sheheryar Ibrahim indicated no relevant financial relationships.
Muhammad Tayyab Ijaz indicated no relevant financial relationships.
Amina Arif indicated no relevant financial relationships.
Misbah Bibi indicated no relevant financial relationships.
Taha Bin Arif, MBBS, MD1, Muhammad Talha Maniya, MBBS2, Ali Salman, MBBS3, Umm E. Salma Shabbar Banatwala, MBBS3, Sana Murtaza, MBBS, MD4, Sara Ahmad, MBBS5, Sara Aleem, MBBS6, Sanish Abbasi, MBBS7, Fatima Naveed, MBBS8, Kashif Ali, MD9, Muhammad Hamza Shafiq, MBBS10, Sheheryar Ibrahim, MBBS2, Muhammad Tayyab Ijaz, MBBS11, Amina Arif, MBBS12, Misbah Bibi, MBBS13. P2652 - A Dual Diagnosis, a Double Burden: Racial and Ethnic Disparities in Colorectal Cancer and Cardiovascular Diseases-Related Hospital Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Sinai Hospital of Baltimore, The George Washington University Regional Medical Campus, Baltimore, MD; 2Ziauddin University, Karachi, Sindh, Pakistan; 3Dow University of Health Sciences, Karachi, Sindh, Pakistan; 4Punjab Medical College, Faisalabad, Punjab, Pakistan; 5University Medical and Dental College, Faisalabad, Punjab, Pakistan; 6Sialkot Medical College, Sialkot, Punjab, Pakistan; 7Peoples University of Medical and Health Sciences, Nawabshah, Sindh, Pakistan; 8Rawal Institute of Health Sciences, Islamabad, Punjab, Pakistan; 9University of Texas Rio Grande Valley, Edinburg, TX; 10Bolan Medical College, Quetta, Balochistan, Pakistan; 11CMH Lahore Medical College, Lahore, Punjab, Pakistan; 12Sharif Medical and Dental College, Narowal, Punjab, Pakistan; 13Bahria University Health Sciences Campus, Karachi, Sindh, Pakistan
Introduction: Cardiovascular disease (CVD) and colorectal cancer (CRC) are major contributors to morbidity and mortality in the United States, with evidence suggesting disproportionately adverse outcomes among racial and ethnic minorities. However, limited national data exist on how race and ethnicity influence the cardiovascular burden and related in-hospital outcomes in patients with CRC. We evaluated racial disparities in in-hospital mortality, length of stay (LOS), and healthcare costs among patients hospitalized with concurrent CRC and CVD.
Methods: A retrospective cross-sectional analysis of the National Inpatient Sample from 2018 to 2020 was conducted, identifying 232,720 adult hospitalizations with a primary diagnosis of CRC and a secondary diagnosis of at least one CVD, defined as myocardial infarction, dysrhythmia, coronary artery disease, heart failure, hypertension, or stroke. Multivariable logistic and linear regression models were used to evaluate the association between race/ethnicity and in-hospital outcomes, including mortality, LOS, and total hospitalization costs, adjusting for patient demographics, clinical comorbidities, and hospital characteristics.
Results: Among the 232,720 hospitalizations analyzed, 71.7% of patients were identified as White, 13.7% as Black, 8.3% as Hispanic, 3.3% as Asian/Pacific Islander, and 3.0% as Other. Black patients exhibited significantly higher in-hospital mortality (OR: 1.33; 95% CI: 1.12–1.58; p = 0.001), extended LOS (β = 0.97 days; 95% CI: 0.74–1.20; p < 0.001), and elevated costs (β = $4,695; 95% CI: $1,424–$7,966; p = 0.005) than Whites with CVD and CRC. Hispanics experienced the highest inflation-adjusted hospital charges (β = $20,281; 95% CI: $14,787–$25,776; p < 0.001) alongside a moderately prolonged LOS (β = 0.37 days; 95% CI: 0.10–0.64; p = 0.006). Asians were disproportionately affected by rectal cancers (22%), while their Black and Hispanic counterparts demonstrated higher rates of anus and anal canal cancers (2.6% and 2.5%, respectively). Metastatic disease prevalence was greatest amongst the Black (40%) and Asian (35%) population.
Discussion: Racial disparities in in-hospital outcomes among patients with concurrent colorectal cancer and cardiovascular disease are pronounced. Black and Hispanic patients experience significantly higher mortality, longer hospital stays, and greater healthcare costs compared to Whites. These findings highlight an urgent need for equity-focused strategies to address these structural and clinical inequities.
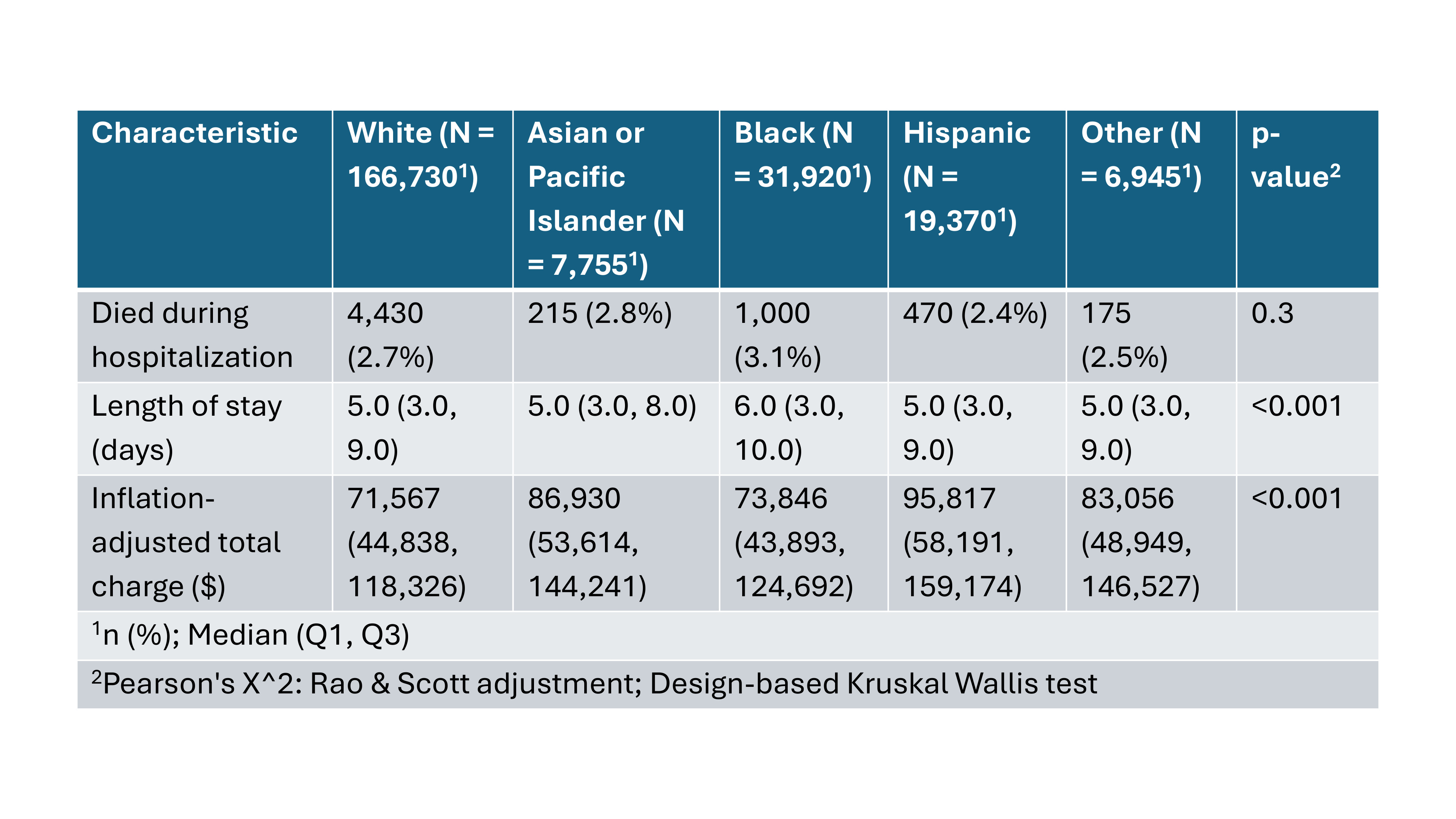
Figure: Figure 1: Hospitalization Outcomes by Racial and Ethnic Groups: Mortality, Length of Stay, and Total Charges.
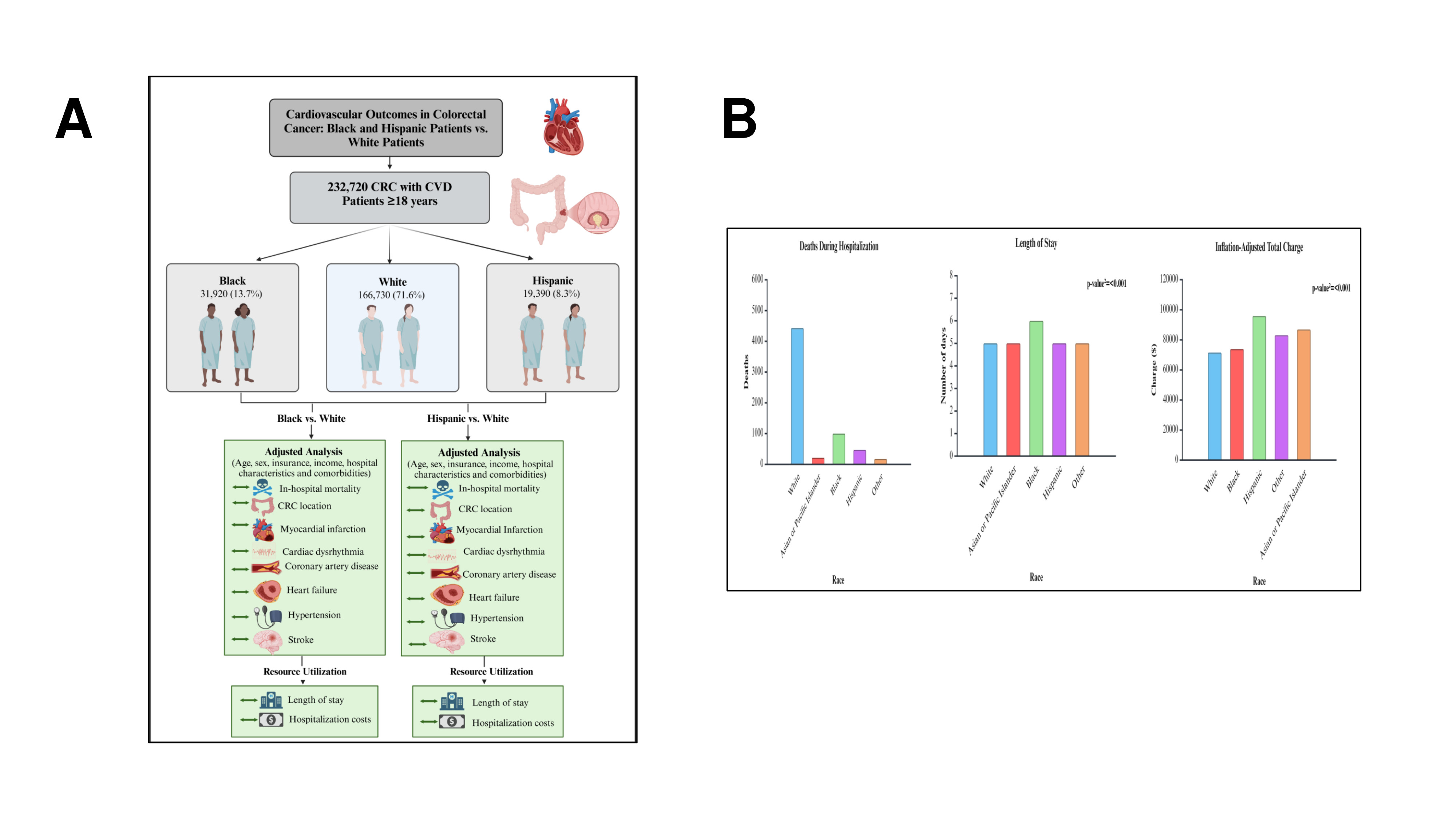
Figure: Figure 2A: Graphical Abstract; 2B: Bar graphs of deaths during hospitalization, length of stay, and inflation-adjusted total charges among different races.
Disclosures:
Taha Bin Arif indicated no relevant financial relationships.
Muhammad Talha Maniya indicated no relevant financial relationships.
Ali Salman indicated no relevant financial relationships.
Umm E. Salma Shabbar Banatwala indicated no relevant financial relationships.
Sana Murtaza indicated no relevant financial relationships.
Sara Ahmad indicated no relevant financial relationships.
Sara Aleem indicated no relevant financial relationships.
Sanish Abbasi indicated no relevant financial relationships.
Fatima Naveed indicated no relevant financial relationships.
Kashif Ali indicated no relevant financial relationships.
Muhammad Hamza Shafiq indicated no relevant financial relationships.
Sheheryar Ibrahim indicated no relevant financial relationships.
Muhammad Tayyab Ijaz indicated no relevant financial relationships.
Amina Arif indicated no relevant financial relationships.
Misbah Bibi indicated no relevant financial relationships.
Taha Bin Arif, MBBS, MD1, Muhammad Talha Maniya, MBBS2, Ali Salman, MBBS3, Umm E. Salma Shabbar Banatwala, MBBS3, Sana Murtaza, MBBS, MD4, Sara Ahmad, MBBS5, Sara Aleem, MBBS6, Sanish Abbasi, MBBS7, Fatima Naveed, MBBS8, Kashif Ali, MD9, Muhammad Hamza Shafiq, MBBS10, Sheheryar Ibrahim, MBBS2, Muhammad Tayyab Ijaz, MBBS11, Amina Arif, MBBS12, Misbah Bibi, MBBS13. P2652 - A Dual Diagnosis, a Double Burden: Racial and Ethnic Disparities in Colorectal Cancer and Cardiovascular Diseases-Related Hospital Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
