Monday Poster Session
Category: Colon
P2549 - Unmasking the Diarrhea: A Case of Mycophenolate-Induced Colitis in a Renal Transplant Patient with Crohn’s Disease and History of CMV Viremia

Rosemary Ansah, MD, MPH
University of Maryland Medical Center
Baltimore, MD
Presenting Author(s)
University of Maryland Medical Center, Baltimore, MD
Introduction:
Diarrhea is a common side effect of mycophenolate mofetil in solid organ transplant patients and mycophenolate-induced colitis in this population is well-described. For transplant patients with other medical conditions that can mimic colitis, diagnosis can be obscured by these disease presentations, often requiring extensive evaluation for a broad array of etiologies. We describe a case of diarrhea in a renal transplant patient with Crohn’s disease and recent CMV viremia initially obscuring diagnosis.
Case Description/
Methods:
A 68-year-old male with history of Crohn’s disease, renal transplant in 2023, and prior cytomegalovirus (CMV) viremia on valganciclovir presented with watery diarrhea for several weeks. He denied recent travel, food poisoning, sick contacts, over-the-counter medications or herbal supplements.
He reported adherence to his immunosuppressants including oral tacrolimus 5 mg daily, mycophenolate 720 mg bid, and prednisone 5 mg daily. Mycophenolate had been recently doubled to 720 mg twice daily for chronic T-cell mediated rejection seen on renal biopsy one month prior. Laboratory tests showed acute kidney injury (AKI) and normal gap metabolic acidosis. CT scan of his abdomen and pelvis was without acute pathology.
Infectious colitis was ruled out. Inflammatory markers and fecal calprotectin were normal. Supportive care was provided, and his mycophenolate was decreased to 360 mg TID. AKI and metabolic acidosis resolved. His diarrhea improved but did not resolve. Colonoscopy was normal aside from small diverticula in the descending and ascending colon. Random biopsies were taken.
Colon histopathology reported crypt loss and increased apoptotic bodies in the terminal ileum, ascending and descending colon suggestive of mycophenolate colitis or graft versus host disease. Increased eosinophils were more suggestive of a drug related process. There was no evidence of increased IBD activity. Immunohistochemical staining was negative for CMV.
Mycophenolate was discontinued and Azathioprine initiated. At follow-up visit, he reported diarrhea had completely resolved.
Discussion: This case exemplifies the diagnostic approach to a confounding clinical presentation. Adopting a broad and systematic approach to evaluation for diarrhea in a transplant patient is paramount to diagnosis, often beginning with non-invasive tests. Clinicians should have a high index of suspicion for mycophenolate-induced colitis in transplant recipients and perform colonoscopy early to aid in prompt diagnosis.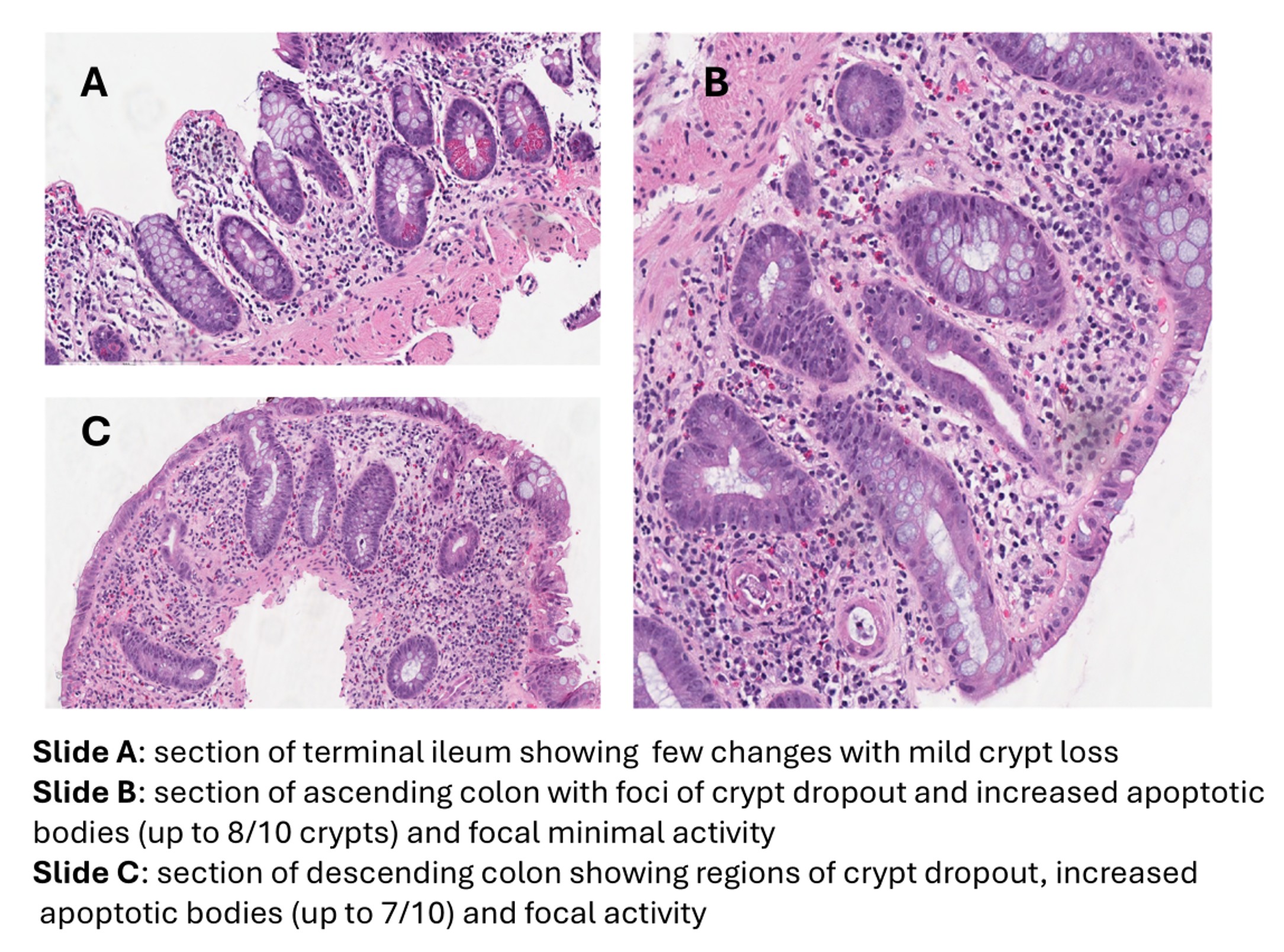
Figure: Figure 1: Histopathology slides of colon biopsy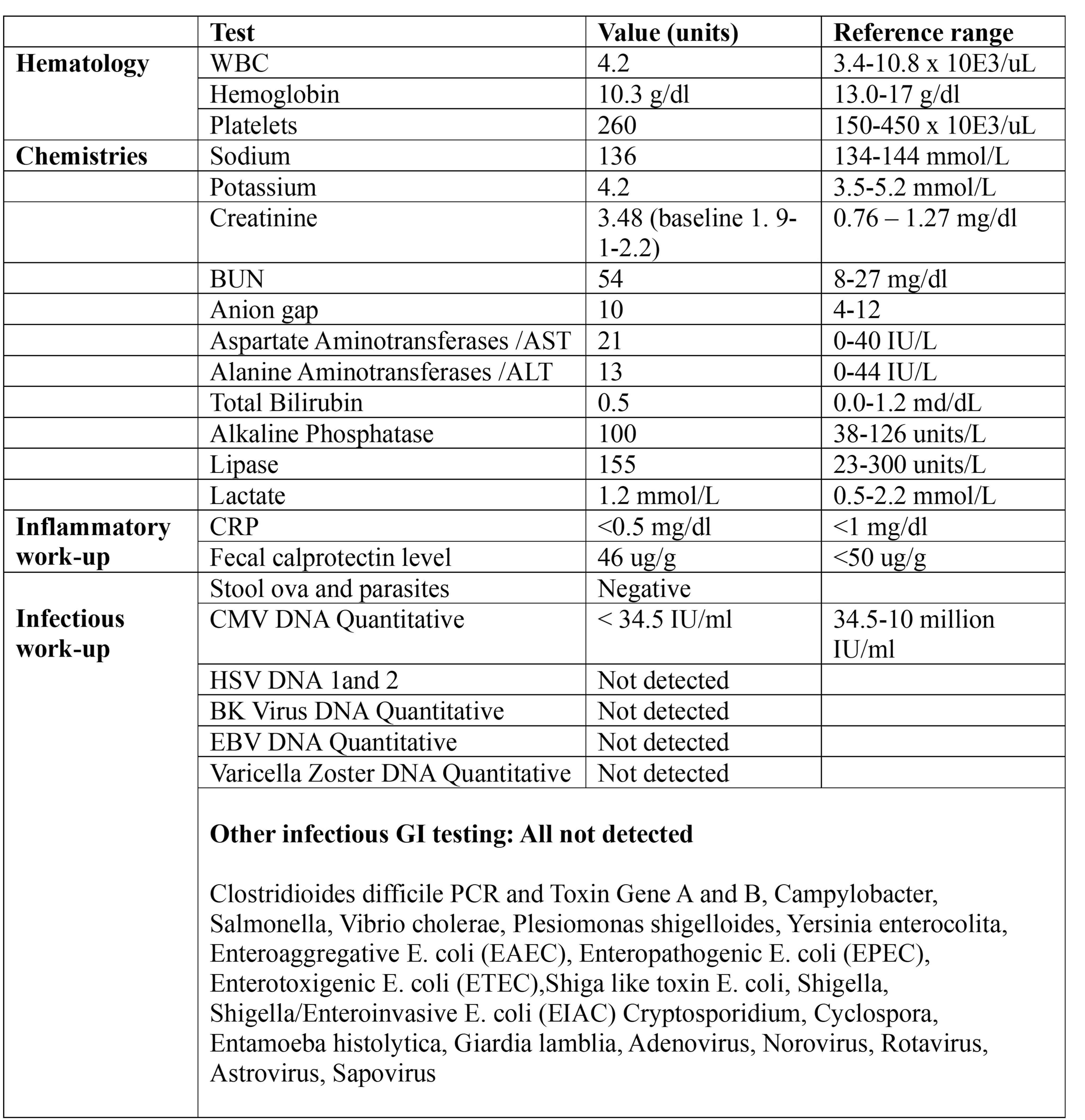
Figure: Table 1. Highlighting pertinent results
Disclosures:
Rosemary Ansah indicated no relevant financial relationships.
Ebehiwele Ebhohon indicated no relevant financial relationships.
Amy Plotkin indicated no relevant financial relationships.
Zurabi Lominadze indicated no relevant financial relationships.
Rosemary Ansah, MD, MPH, Ebehiwele Ebhohon, MBBS, MPH, MsCr, Amy Plotkin, MD, Zurabi Lominadze, MD. P2549 - Unmasking the Diarrhea: A Case of Mycophenolate-Induced Colitis in a Renal Transplant Patient with Crohn’s Disease and History of CMV Viremia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
