Monday Poster Session
Category: Colon
P2540 - A Case of Trastuzumab Deruxtecan Induced Colitis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Hannah O'Neill, MD (she/her/hers)
Houston Methodist-Weill Cornell Graduate School of Medical Sciences
Houston, TX
Presenting Author(s)
Hannah O'Neill, MD1, Rajdeepsingh Waghela, MD2, Santos A. Acosta Martinez, MD3, Malcolm Irani, DO4, Neha Mathur, MD5, Christopher Fan, MD6, Bincy Abraham, MD, MS, FACG7
1Houston Methodist-Weill Cornell Graduate School of Medical Sciences, Houston, TX; 2Houston Methodist, Houston, TX; 3Houston Methodist Hospital, Department of Pathology and Genomic Medicine, Houston, TX; 4Houston Methodist Hospital, Houston, TX; 5Houston Methodist Hospital, Division of Gastroenterology and Hepatology, Lynda K. and David M. Underwood Center for Digestive Health, Houston, TX; 6Houston Methodist Hospital, Division of Gastroenterology and Hepatology, Lynda K. and David M. Underwood Center for Digestive Health / Houston Methodist Research Institute, Department of Medicine / Weill Cornell Medical College, Cornell University, Houston, TX; 7Division of Gastroenterology & Hepatology, Houston Methodist-Weill Cornell, Houston, TX
Introduction: Trastuzumab deruxtecan (TDX-d) targeting human epidermal growth factor receptor 2 (HER2) was introduced as salvage therapy for metastatic/unresectable HER2-positive1 & HER2-negative breast cancer2. A 2022 meta-analysis confirmed known adverse events including drug-related colitis3. Phase 1 trials note colitis as a rare event4. To the best of our knowledge, this is the first reported case outside a clinical trial of TDX-d associated colitis.
Case Description/
Methods: A 49-year-old female with recurrent, metastatic triple negative breast cancer presented with diarrhea & encephalopathy after TDX-d initiation. She was admitted for hypovolemic shock, requiring ventilator support & renal replacement. She had pancytopenia, severe neutropenia, kidney injury, & liver injury. Infectious workup was negative. Computed Tomography scan showed pancolitis. She developed hematochezia and colonoscopy had extensive ulceration. Pathology revealed chronic colitis suspicious for drug-induced colitis and without cytomegalovirus or ischemia. TDX-d was discontinued. Methylprednisolone (initially 40 mg PO daily up to 60 mg twice daily) failed to provide improvement. Cyclosporine (2 mg/kg IV to 100 mg PO twice daily) was initiated with diarrhea improvement / hematochezia resolution, however, symptoms recurred 15 days later. She was transitioned to infliximab (10 mg/kg IV) and received 2 doses 2 weeks apart, however, her diarrhea and inflammation persisted. Unfortunately, in the setting of refractory colitis, deconditioning & advancing disease with brain metastasis, she was transitioned to comfort care.
Discussion: Drug induced colitis is a known complication of many medications, including irinotecan and deruxtecan6,7,8. Deruxtecan can cause apoptotic death9, and the drug class is associated with injury at the intestinal lining10. The mechanism of TDX-d induced colitis is unclear. For those on TDX-d, abdominal pain & hematochezia should raise suspicion for drug-induced colitis. Although unsuccessful in our case, TNF-a inhibition is a highly effective treatment for steroid-resistant drug-induced colitis. IL-6 inhibition may treat immune checkpoint inhibitor- associated colitis12. When drug-induced colitis is suspected, diagnosis & severity should be endoscopically confirmed13 & the causal agent discontinued. If colitis is severe / persistent, systemic glucocorticoids are first-line, & alternative immunosuppression such as those used above can be considered. In severe cases, surgical evaluation may be indicated.
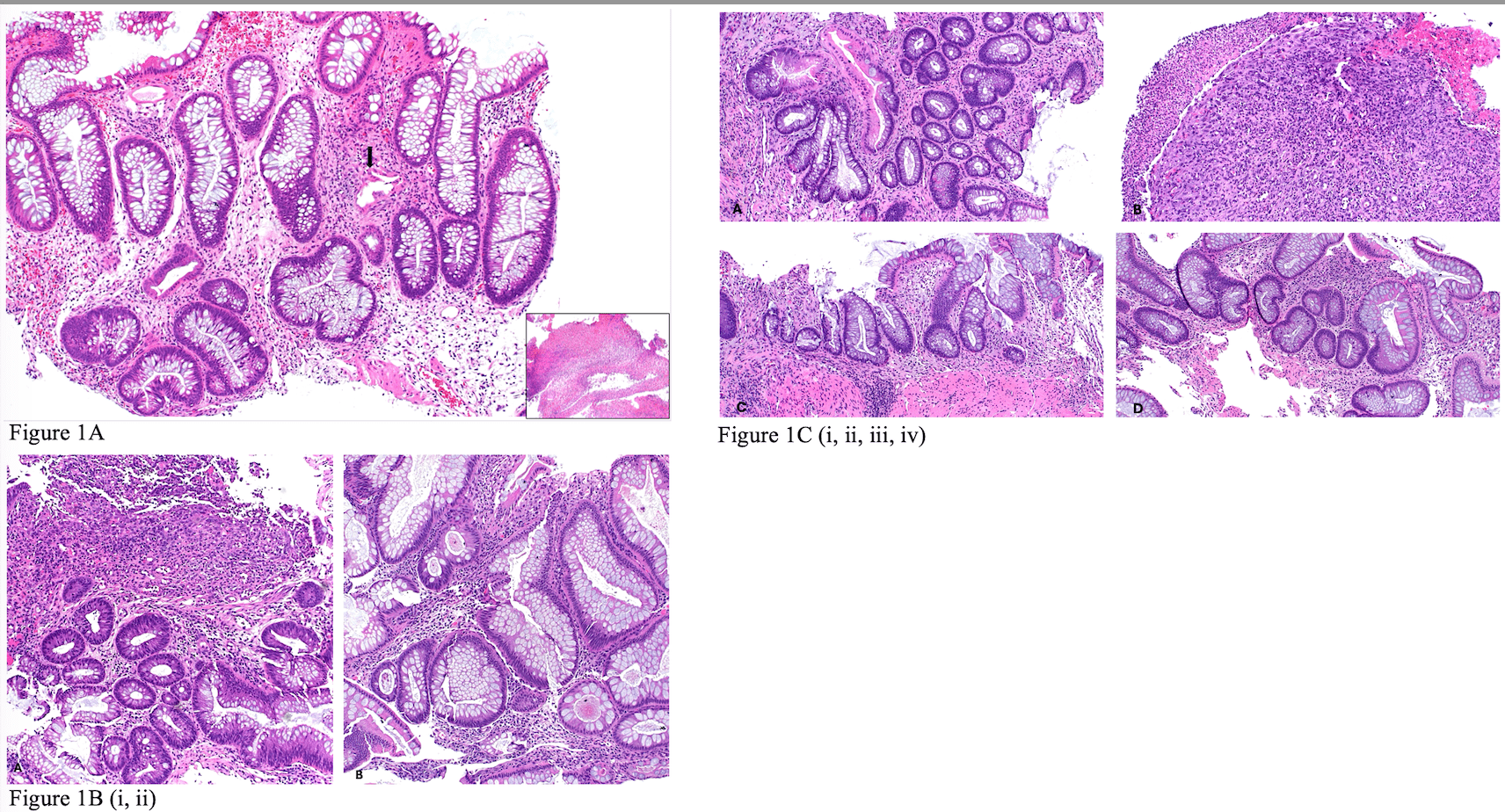
Figure: Figure 1A: First Rectosigmoid biopsy showing crypt distortion and focal dilated damaged crypt (arrow). The lamina propria shows edema and mild lymphocytic inflammation. Inset image: granulation tissue consistent with ulcer. Hematoxylin and Eosin stain. 100x
Figure 1B:
i. Sigmoid biopsy showing ulcerated mucosa with crypt distortion and crypt regenerative changes.
ii. Rectal biopsy showing crypt distortion and post-inflammatory mucinous hyperplasia. Hematoxylin and Eosin stain. 100x
Figure 1C:
Features of chronic colitis.
i. Descending colon biopsy with crypt distortion and paneth cell metaplasia.
ii. Descending colon biopsy with ulcer (granulation tissue).
iii. Sigmoid colon biopsy with crypt distortion.
iv. Rectal biopsy with crypt distortion. Hematoxylin and eosin stain. 100x
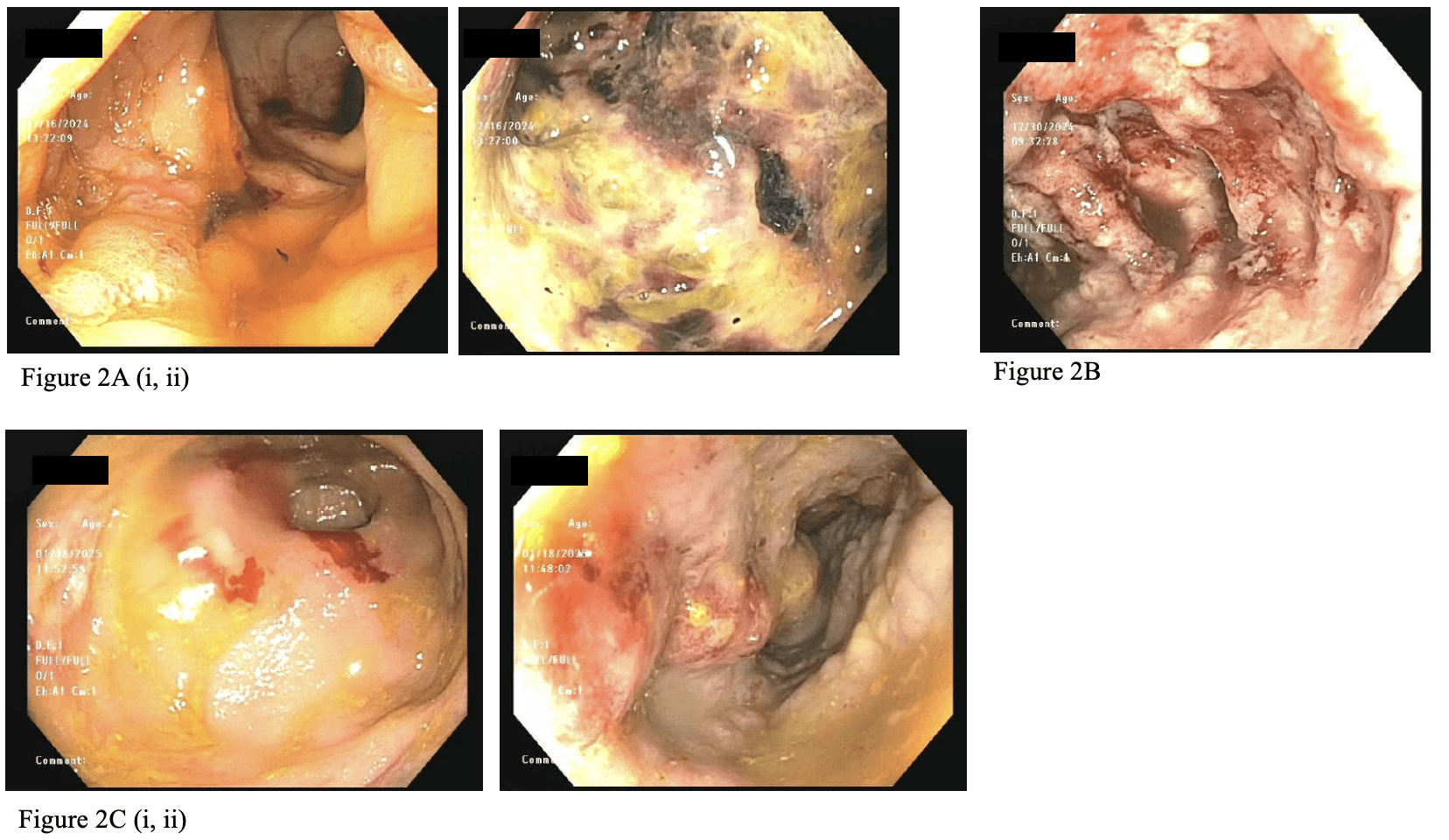
Figure: Figure 2A: Initial flexible sigmoidoscopy with diffuse areas of severely altered vascular, erythematous, eroded, friable, hemorrhagic, inflamed, nodular, and ulcerated mucosa in the rectum and recto-sigmoid colon up to 30 cm.
Figure 2B:
Diffuse area of severely congested, erythematous, friable, inflamed, nodular and ulcerated mucosa extending from the recto-sigmoid colon to the descending colon, as noted in this view of the sigmoid colon.
Figure 2C:
Segmental and patchy area of severely altered vascularity, nodular and ulcerated mucosa in the rectosigmoid colon, sigmoid colon, descending colon, splenic flexure, and transverse colon, as noted in these views of the rectum (i) and descending colon (ii).
Disclosures:
Hannah O'Neill indicated no relevant financial relationships.
Rajdeepsingh Waghela indicated no relevant financial relationships.
Santos Acosta Martinez indicated no relevant financial relationships.
Malcolm Irani: ABBVIE – Speakers Bureau.
Neha Mathur: Ardelyx – Speakers Bureau. Regeneron – Advisor or Review Panel Member, Speakers Bureau. Sanofi – Advisor or Review Panel Member, Speakers Bureau.
Christopher Fan indicated no relevant financial relationships.
Bincy Abraham: Abbvie – Consultant, Speakers Bureau. Celltrion – Consultant. Eli Lilly – Consultant, Speakers Bureau. Johnson and Johnson – Consultant, Speakers Bureau. Pfizer – Consultant. Sanofi – Consultant. Takeda – Consultant, Speakers Bureau.
Hannah O'Neill, MD1, Rajdeepsingh Waghela, MD2, Santos A. Acosta Martinez, MD3, Malcolm Irani, DO4, Neha Mathur, MD5, Christopher Fan, MD6, Bincy Abraham, MD, MS, FACG7. P2540 - A Case of Trastuzumab Deruxtecan Induced Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Houston Methodist-Weill Cornell Graduate School of Medical Sciences, Houston, TX; 2Houston Methodist, Houston, TX; 3Houston Methodist Hospital, Department of Pathology and Genomic Medicine, Houston, TX; 4Houston Methodist Hospital, Houston, TX; 5Houston Methodist Hospital, Division of Gastroenterology and Hepatology, Lynda K. and David M. Underwood Center for Digestive Health, Houston, TX; 6Houston Methodist Hospital, Division of Gastroenterology and Hepatology, Lynda K. and David M. Underwood Center for Digestive Health / Houston Methodist Research Institute, Department of Medicine / Weill Cornell Medical College, Cornell University, Houston, TX; 7Division of Gastroenterology & Hepatology, Houston Methodist-Weill Cornell, Houston, TX
Introduction: Trastuzumab deruxtecan (TDX-d) targeting human epidermal growth factor receptor 2 (HER2) was introduced as salvage therapy for metastatic/unresectable HER2-positive1 & HER2-negative breast cancer2. A 2022 meta-analysis confirmed known adverse events including drug-related colitis3. Phase 1 trials note colitis as a rare event4. To the best of our knowledge, this is the first reported case outside a clinical trial of TDX-d associated colitis.
Case Description/
Methods: A 49-year-old female with recurrent, metastatic triple negative breast cancer presented with diarrhea & encephalopathy after TDX-d initiation. She was admitted for hypovolemic shock, requiring ventilator support & renal replacement. She had pancytopenia, severe neutropenia, kidney injury, & liver injury. Infectious workup was negative. Computed Tomography scan showed pancolitis. She developed hematochezia and colonoscopy had extensive ulceration. Pathology revealed chronic colitis suspicious for drug-induced colitis and without cytomegalovirus or ischemia. TDX-d was discontinued. Methylprednisolone (initially 40 mg PO daily up to 60 mg twice daily) failed to provide improvement. Cyclosporine (2 mg/kg IV to 100 mg PO twice daily) was initiated with diarrhea improvement / hematochezia resolution, however, symptoms recurred 15 days later. She was transitioned to infliximab (10 mg/kg IV) and received 2 doses 2 weeks apart, however, her diarrhea and inflammation persisted. Unfortunately, in the setting of refractory colitis, deconditioning & advancing disease with brain metastasis, she was transitioned to comfort care.
Discussion: Drug induced colitis is a known complication of many medications, including irinotecan and deruxtecan6,7,8. Deruxtecan can cause apoptotic death9, and the drug class is associated with injury at the intestinal lining10. The mechanism of TDX-d induced colitis is unclear. For those on TDX-d, abdominal pain & hematochezia should raise suspicion for drug-induced colitis. Although unsuccessful in our case, TNF-a inhibition is a highly effective treatment for steroid-resistant drug-induced colitis. IL-6 inhibition may treat immune checkpoint inhibitor- associated colitis12. When drug-induced colitis is suspected, diagnosis & severity should be endoscopically confirmed13 & the causal agent discontinued. If colitis is severe / persistent, systemic glucocorticoids are first-line, & alternative immunosuppression such as those used above can be considered. In severe cases, surgical evaluation may be indicated.
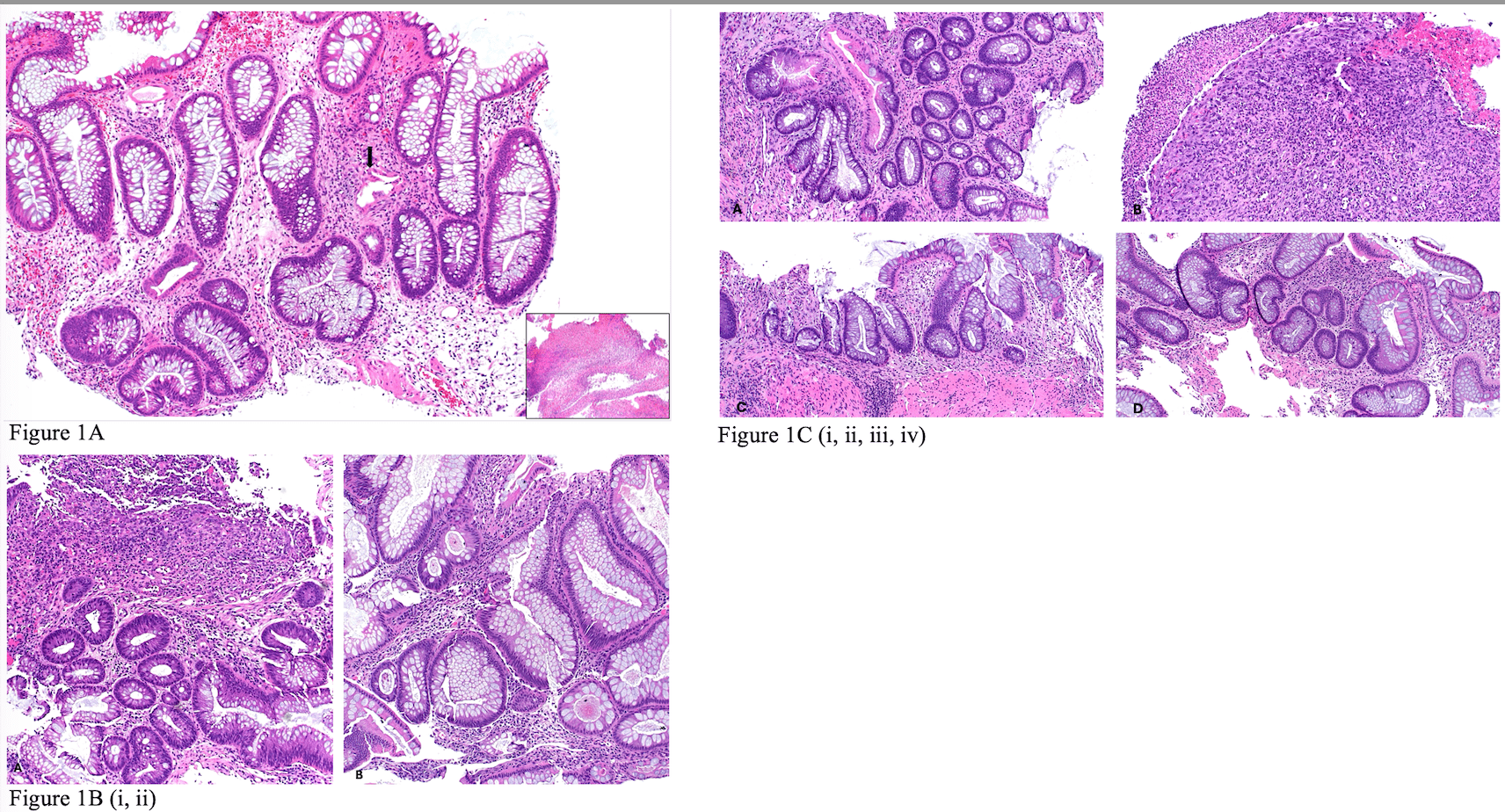
Figure: Figure 1A: First Rectosigmoid biopsy showing crypt distortion and focal dilated damaged crypt (arrow). The lamina propria shows edema and mild lymphocytic inflammation. Inset image: granulation tissue consistent with ulcer. Hematoxylin and Eosin stain. 100x
Figure 1B:
i. Sigmoid biopsy showing ulcerated mucosa with crypt distortion and crypt regenerative changes.
ii. Rectal biopsy showing crypt distortion and post-inflammatory mucinous hyperplasia. Hematoxylin and Eosin stain. 100x
Figure 1C:
Features of chronic colitis.
i. Descending colon biopsy with crypt distortion and paneth cell metaplasia.
ii. Descending colon biopsy with ulcer (granulation tissue).
iii. Sigmoid colon biopsy with crypt distortion.
iv. Rectal biopsy with crypt distortion. Hematoxylin and eosin stain. 100x
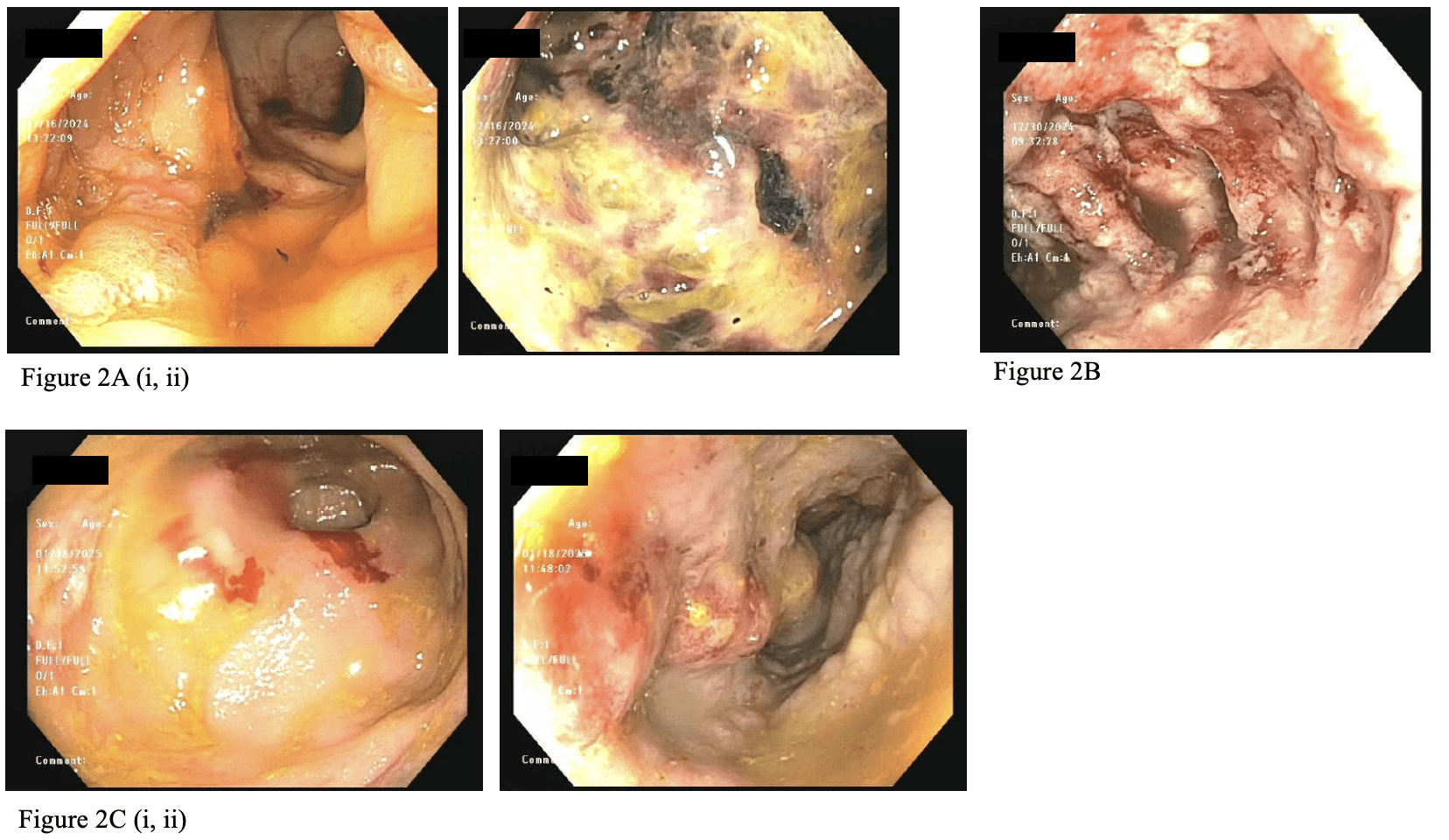
Figure: Figure 2A: Initial flexible sigmoidoscopy with diffuse areas of severely altered vascular, erythematous, eroded, friable, hemorrhagic, inflamed, nodular, and ulcerated mucosa in the rectum and recto-sigmoid colon up to 30 cm.
Figure 2B:
Diffuse area of severely congested, erythematous, friable, inflamed, nodular and ulcerated mucosa extending from the recto-sigmoid colon to the descending colon, as noted in this view of the sigmoid colon.
Figure 2C:
Segmental and patchy area of severely altered vascularity, nodular and ulcerated mucosa in the rectosigmoid colon, sigmoid colon, descending colon, splenic flexure, and transverse colon, as noted in these views of the rectum (i) and descending colon (ii).
Disclosures:
Hannah O'Neill indicated no relevant financial relationships.
Rajdeepsingh Waghela indicated no relevant financial relationships.
Santos Acosta Martinez indicated no relevant financial relationships.
Malcolm Irani: ABBVIE – Speakers Bureau.
Neha Mathur: Ardelyx – Speakers Bureau. Regeneron – Advisor or Review Panel Member, Speakers Bureau. Sanofi – Advisor or Review Panel Member, Speakers Bureau.
Christopher Fan indicated no relevant financial relationships.
Bincy Abraham: Abbvie – Consultant, Speakers Bureau. Celltrion – Consultant. Eli Lilly – Consultant, Speakers Bureau. Johnson and Johnson – Consultant, Speakers Bureau. Pfizer – Consultant. Sanofi – Consultant. Takeda – Consultant, Speakers Bureau.
Hannah O'Neill, MD1, Rajdeepsingh Waghela, MD2, Santos A. Acosta Martinez, MD3, Malcolm Irani, DO4, Neha Mathur, MD5, Christopher Fan, MD6, Bincy Abraham, MD, MS, FACG7. P2540 - A Case of Trastuzumab Deruxtecan Induced Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
