Monday Poster Session
Category: Colon
P2539 - Invasive Lobular Carcinoma With Delayed Colonic Metastasis: An Underrecognized Pattern of Spread
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Hannah Darnell, DO
University of Kentucky
Lexington, KY
Presenting Author(s)
Hannah Darnell, DO1, Neha Srinivasan, MD2, Jessica Moss, MD2, Deborah Flomenhoft, MD2
1University of Kentucky, Lexington, KY; 2University of Kentucky College of Medicine, Lexington, KY
Introduction: Breast cancer, the most common malignancy in women, typically metastasizing to the bones, lungs, liver, and brain. Metastasis to the gastrointestinal (GI) tract, particularly the colon, is rare and often diagnostically challenging. Invasive lobular carcinoma (ILC), a histologic subtype of breast cancer, is more prone to metastasize to atypical locations, including the GI tract. Such cases can mimic primary colorectal cancer or benign GI conditions, leading to diagnostic delays and worse outcomes. We present a case of colonic metastases from ILC diagnosed eight years after initial breast cancer, highlighting diagnostic challenges and the need for heightened clinical awareness even in the setting of recent colon cancer screening.
Case Description/
Methods: A 79-year-old female with an eight-year history of left-sided ER+/PR+/HER2– ILC, treated with mastectomy, axillary lymph node dissection (6 of 11 nodes positive), and long-term aromatase inhibitor therapy, presented with abdominal bloating, altered bowel habits, and rectal bleeding. Notably, she had a normal colonoscopy three years prior. Despite this, a repeat colonoscopy revealed a 10 cm rectal mass (Fig. 1), multiple areas of extrinsic compression, and nodular mucosa (Fig. 2). Biopsies from the rectum, hepatic flexure, ascending, and transverse colon confirmed metastatic lobular breast carcinoma. Imaging showed bilateral pleural effusions, peritoneal carcinomatosis, and hypermetabolic foci in the rectum, sigmoid colon, and distal esophagus. Cytology from thoracentesis and paracentesis was positive for metastatic ILC. She was treated with palliative systemic therapy; surgery was not pursued.
Discussion: Although autopsy studies report GI involvement in up to 35% of metastatic ILC cases, colonic metastases remain rare, occurring in only about 3%. GI manifestations typically appear around eight years after initial ILC diagnosis but can emerge as late as 30 years. Nonspecific symptoms and overlapping imaging findings with primary colorectal cancer make diagnosis challenging. Endoscopic biopsy with histopathology and immunohistochemistry is essential to distinguish metastatic breast cancer from primary colorectal malignancy. The median survival after colonic breast cancer metastasis is approximately 16 months. Clinicians should therefore maintain a high index of suspicion in patients with a history of ILC who present with new, unexplained GI symptoms—even years after initial treatment—as early recognition may improve outcomes.

Figure: Colonoscopy revealing a 10 cm circumferential, infiltrative rectal mass causing partial luminal obstruction. The lesion was palpable on digital rectal examination.
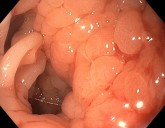
Figure: Colonoscopy showing nodular mucosa of the hepatic flexure. Biopsy revealed infiltrative carcinoma consistent with metastatic invasive lobular carcinoma.
Disclosures:
Hannah Darnell indicated no relevant financial relationships.
Neha Srinivasan indicated no relevant financial relationships.
Jessica Moss indicated no relevant financial relationships.
Deborah Flomenhoft indicated no relevant financial relationships.
Hannah Darnell, DO1, Neha Srinivasan, MD2, Jessica Moss, MD2, Deborah Flomenhoft, MD2. P2539 - Invasive Lobular Carcinoma With Delayed Colonic Metastasis: An Underrecognized Pattern of Spread, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Kentucky, Lexington, KY; 2University of Kentucky College of Medicine, Lexington, KY
Introduction: Breast cancer, the most common malignancy in women, typically metastasizing to the bones, lungs, liver, and brain. Metastasis to the gastrointestinal (GI) tract, particularly the colon, is rare and often diagnostically challenging. Invasive lobular carcinoma (ILC), a histologic subtype of breast cancer, is more prone to metastasize to atypical locations, including the GI tract. Such cases can mimic primary colorectal cancer or benign GI conditions, leading to diagnostic delays and worse outcomes. We present a case of colonic metastases from ILC diagnosed eight years after initial breast cancer, highlighting diagnostic challenges and the need for heightened clinical awareness even in the setting of recent colon cancer screening.
Case Description/
Methods: A 79-year-old female with an eight-year history of left-sided ER+/PR+/HER2– ILC, treated with mastectomy, axillary lymph node dissection (6 of 11 nodes positive), and long-term aromatase inhibitor therapy, presented with abdominal bloating, altered bowel habits, and rectal bleeding. Notably, she had a normal colonoscopy three years prior. Despite this, a repeat colonoscopy revealed a 10 cm rectal mass (Fig. 1), multiple areas of extrinsic compression, and nodular mucosa (Fig. 2). Biopsies from the rectum, hepatic flexure, ascending, and transverse colon confirmed metastatic lobular breast carcinoma. Imaging showed bilateral pleural effusions, peritoneal carcinomatosis, and hypermetabolic foci in the rectum, sigmoid colon, and distal esophagus. Cytology from thoracentesis and paracentesis was positive for metastatic ILC. She was treated with palliative systemic therapy; surgery was not pursued.
Discussion: Although autopsy studies report GI involvement in up to 35% of metastatic ILC cases, colonic metastases remain rare, occurring in only about 3%. GI manifestations typically appear around eight years after initial ILC diagnosis but can emerge as late as 30 years. Nonspecific symptoms and overlapping imaging findings with primary colorectal cancer make diagnosis challenging. Endoscopic biopsy with histopathology and immunohistochemistry is essential to distinguish metastatic breast cancer from primary colorectal malignancy. The median survival after colonic breast cancer metastasis is approximately 16 months. Clinicians should therefore maintain a high index of suspicion in patients with a history of ILC who present with new, unexplained GI symptoms—even years after initial treatment—as early recognition may improve outcomes.

Figure: Colonoscopy revealing a 10 cm circumferential, infiltrative rectal mass causing partial luminal obstruction. The lesion was palpable on digital rectal examination.
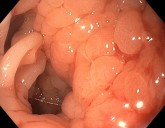
Figure: Colonoscopy showing nodular mucosa of the hepatic flexure. Biopsy revealed infiltrative carcinoma consistent with metastatic invasive lobular carcinoma.
Disclosures:
Hannah Darnell indicated no relevant financial relationships.
Neha Srinivasan indicated no relevant financial relationships.
Jessica Moss indicated no relevant financial relationships.
Deborah Flomenhoft indicated no relevant financial relationships.
Hannah Darnell, DO1, Neha Srinivasan, MD2, Jessica Moss, MD2, Deborah Flomenhoft, MD2. P2539 - Invasive Lobular Carcinoma With Delayed Colonic Metastasis: An Underrecognized Pattern of Spread, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
