Monday Poster Session
Category: Colon
P2520 - Uncommon Pathology in Uncommon Age: Colitis Cystica Profunda in the Youngest Pediatric Case to Date
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ishika A. Golakiya, MBBS (she/her/hers)
Surat Municipal Institute of Medical Education and Research
Surat, Gujarat, India
Presenting Author(s)
Riyakumari B. Patel, MBBS1, Ishika A. Golakiya, MBBS2, Yash M. Hapani, MBBS3, Pradip Vekariya, MD, DM (Gastroenterology)4, Niralkumar L. Ghevariya, MBBS5
1Surat Municipal Institute of Medical Education and Research, McKees Rocks, PA; 2Surat Municipal Institute of Medical Education and Research, Bridgeville, PA; 3Surat Municipal Institute of Medical Education and Research, Jersey City, NJ; 4Ayush Gastro and Liver Centre, Surat, Gujarat, India; 5University of Maryland School of Medicine, Baltimore, MD
Introduction: Colitis Cystica Profunda(CCP), a benign condition primarily affects the submucosal layer of the colon. Histologically, characterized by mucosal cysts that extend deep into the colonic wall, often causing distension of the colonic mucosa. While CCP is commonly seen in adults, there are very few pediatric cases . Here we present an extremely rare case of CCP in a 8-year old child, who represents the youngest patient in available literature to date.
Case Description/
Methods: A 8-year-old boy presented with 3 months of rectal bleeding and intermittent left lower quadrant pain, with no relevant medical, family, or genetic history. He was well nourished with lower abdominal tenderness; vitals and DRE were normal. Labs showed mild anemia (Hb 10.2 g/dL); CRP and coagulation were normal. Abdo-USG showed no abnormalities. Colonoscopy revealed a 4 cm pedunculated sigmoid polyp, removed via detachable end loop and snare. Post-procedure check showed no residual lesion or bleeding. Histology confirmed CCP with submucosal cysts lined by benign epithelium.
Discussion: CCP is a rare benign condition, histologically characterized by mucus filled cyst in the submucosa, often mimic malignant lesions like mucinous adenocarcinomas, mostly in rectum and sigmoid. The localized form usually presents as solitary polyp, while diffuse form usually occurs in IBD. In Pediatric cases, symptoms vary from rectal bleeding, mucorrhea, diarrhea, and colonic obstruction to indeed a pure incidental finding at imaging or colonoscopy. Pathogenesis of CCP includes combination of congenital muscularis mucosa weakness, continuous inflammation, ischemia or trauma causing epithelial herniation. It is important to diagnose and differentiate HPE from malignancies like mucinous adenocarcinomas. CT and MRI are considered for D/D by identifying cystic, non-invasive submucosal lesions. Endoscopic findings often include nodular or polypoid lesions with normal or edematous mucosa. Here, colonoscopy demonstrated a pedunculated polyp histologically confirmed as CCP. Treatment varies according to the size and symptomatology of the lesion. Localized CCP is treated conservatively, whereas CBT shows further evidence of endoscopic removal. Radicals are indicated for cases with complications like obstruction or suspicion of malignant disease. In cases of recurrence monitoring is done through follow-up colonoscopy, but it would generally mean an excellent prognosis with proper management of the condition.
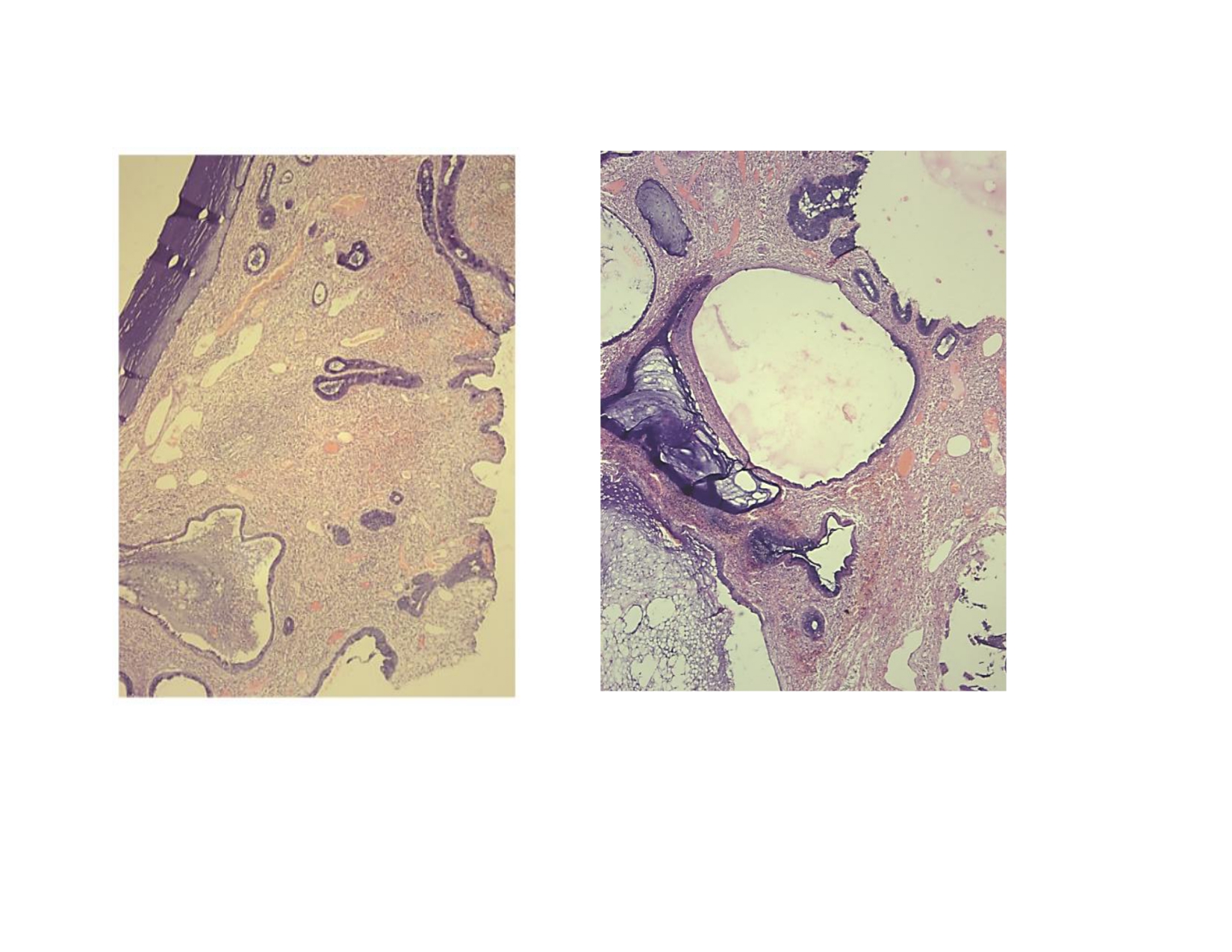
Figure: Histopathology of the Sigmoid polyp- H&E stain at low (left) and Intermediate (Right) magnification showing multiple Mucin filled Cystic spaces extending into submucosa beneath the Muscularis Mucosa. The cysts are lined by benign epithelium without dysplasia, without significant atypia, without destructive glandular invasion which shows features consistent with benign nature of CCP.
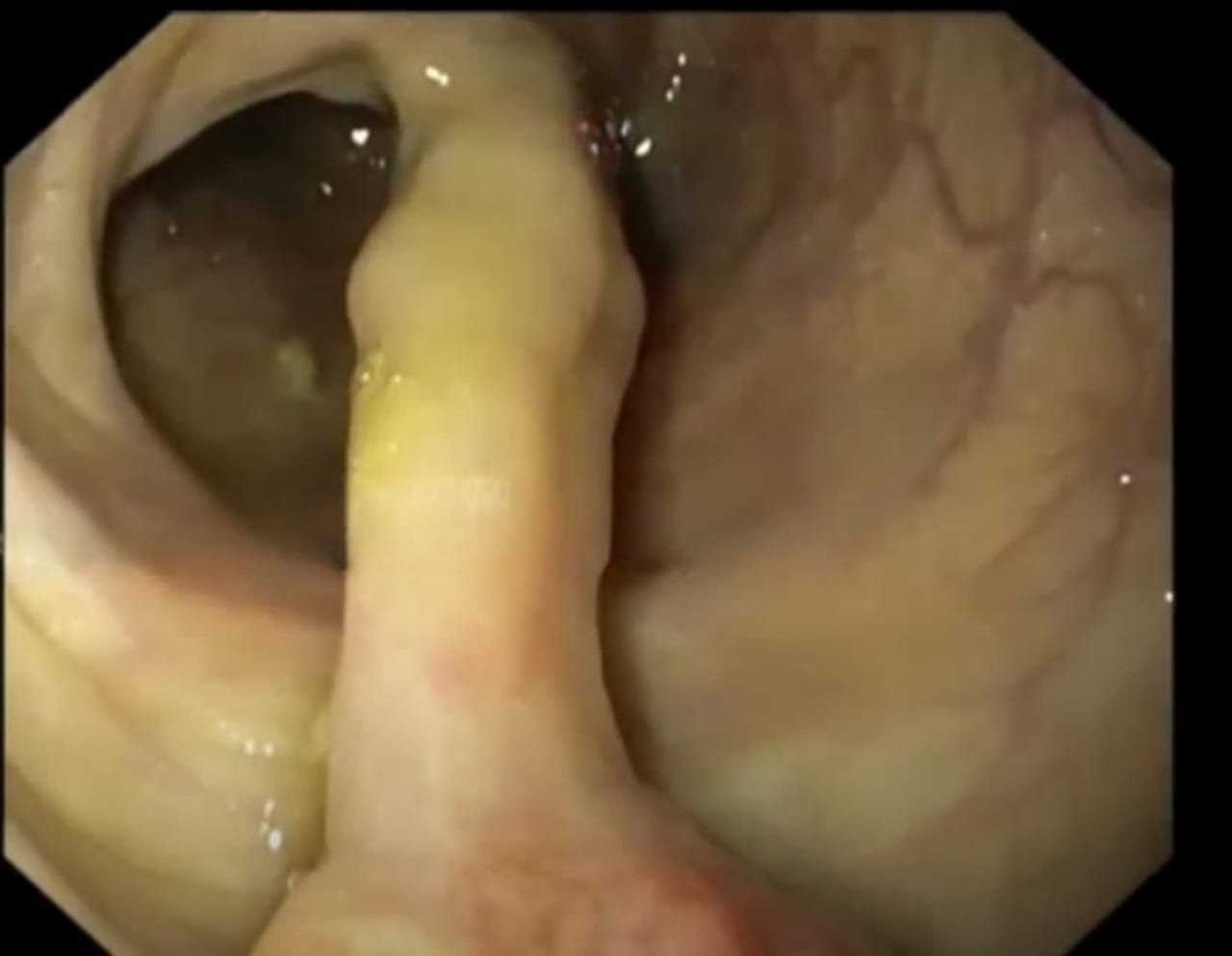
Figure: Colonoscopy showing 4 x 2 x 1.5 cm pedunculated polyp in sigmoid colon. The Polyp surface is smooth and glistening, with a mucosal appearance that is grossly intact, though a subtle yellowish discoloration and mild mucinous coating is noted-possibly reflecting underlying mucin filled Cystic spaces, which are characteristic of Colitis Cystica Profunda.
Disclosures:
Riyakumari Patel indicated no relevant financial relationships.
Ishika Golakiya indicated no relevant financial relationships.
Yash Hapani indicated no relevant financial relationships.
Pradip Vekariya indicated no relevant financial relationships.
Niralkumar Ghevariya indicated no relevant financial relationships.
Riyakumari B. Patel, MBBS1, Ishika A. Golakiya, MBBS2, Yash M. Hapani, MBBS3, Pradip Vekariya, MD, DM (Gastroenterology)4, Niralkumar L. Ghevariya, MBBS5. P2520 - Uncommon Pathology in Uncommon Age: Colitis Cystica Profunda in the Youngest Pediatric Case to Date, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Surat Municipal Institute of Medical Education and Research, McKees Rocks, PA; 2Surat Municipal Institute of Medical Education and Research, Bridgeville, PA; 3Surat Municipal Institute of Medical Education and Research, Jersey City, NJ; 4Ayush Gastro and Liver Centre, Surat, Gujarat, India; 5University of Maryland School of Medicine, Baltimore, MD
Introduction: Colitis Cystica Profunda(CCP), a benign condition primarily affects the submucosal layer of the colon. Histologically, characterized by mucosal cysts that extend deep into the colonic wall, often causing distension of the colonic mucosa. While CCP is commonly seen in adults, there are very few pediatric cases . Here we present an extremely rare case of CCP in a 8-year old child, who represents the youngest patient in available literature to date.
Case Description/
Methods: A 8-year-old boy presented with 3 months of rectal bleeding and intermittent left lower quadrant pain, with no relevant medical, family, or genetic history. He was well nourished with lower abdominal tenderness; vitals and DRE were normal. Labs showed mild anemia (Hb 10.2 g/dL); CRP and coagulation were normal. Abdo-USG showed no abnormalities. Colonoscopy revealed a 4 cm pedunculated sigmoid polyp, removed via detachable end loop and snare. Post-procedure check showed no residual lesion or bleeding. Histology confirmed CCP with submucosal cysts lined by benign epithelium.
Discussion: CCP is a rare benign condition, histologically characterized by mucus filled cyst in the submucosa, often mimic malignant lesions like mucinous adenocarcinomas, mostly in rectum and sigmoid. The localized form usually presents as solitary polyp, while diffuse form usually occurs in IBD. In Pediatric cases, symptoms vary from rectal bleeding, mucorrhea, diarrhea, and colonic obstruction to indeed a pure incidental finding at imaging or colonoscopy. Pathogenesis of CCP includes combination of congenital muscularis mucosa weakness, continuous inflammation, ischemia or trauma causing epithelial herniation. It is important to diagnose and differentiate HPE from malignancies like mucinous adenocarcinomas. CT and MRI are considered for D/D by identifying cystic, non-invasive submucosal lesions. Endoscopic findings often include nodular or polypoid lesions with normal or edematous mucosa. Here, colonoscopy demonstrated a pedunculated polyp histologically confirmed as CCP. Treatment varies according to the size and symptomatology of the lesion. Localized CCP is treated conservatively, whereas CBT shows further evidence of endoscopic removal. Radicals are indicated for cases with complications like obstruction or suspicion of malignant disease. In cases of recurrence monitoring is done through follow-up colonoscopy, but it would generally mean an excellent prognosis with proper management of the condition.
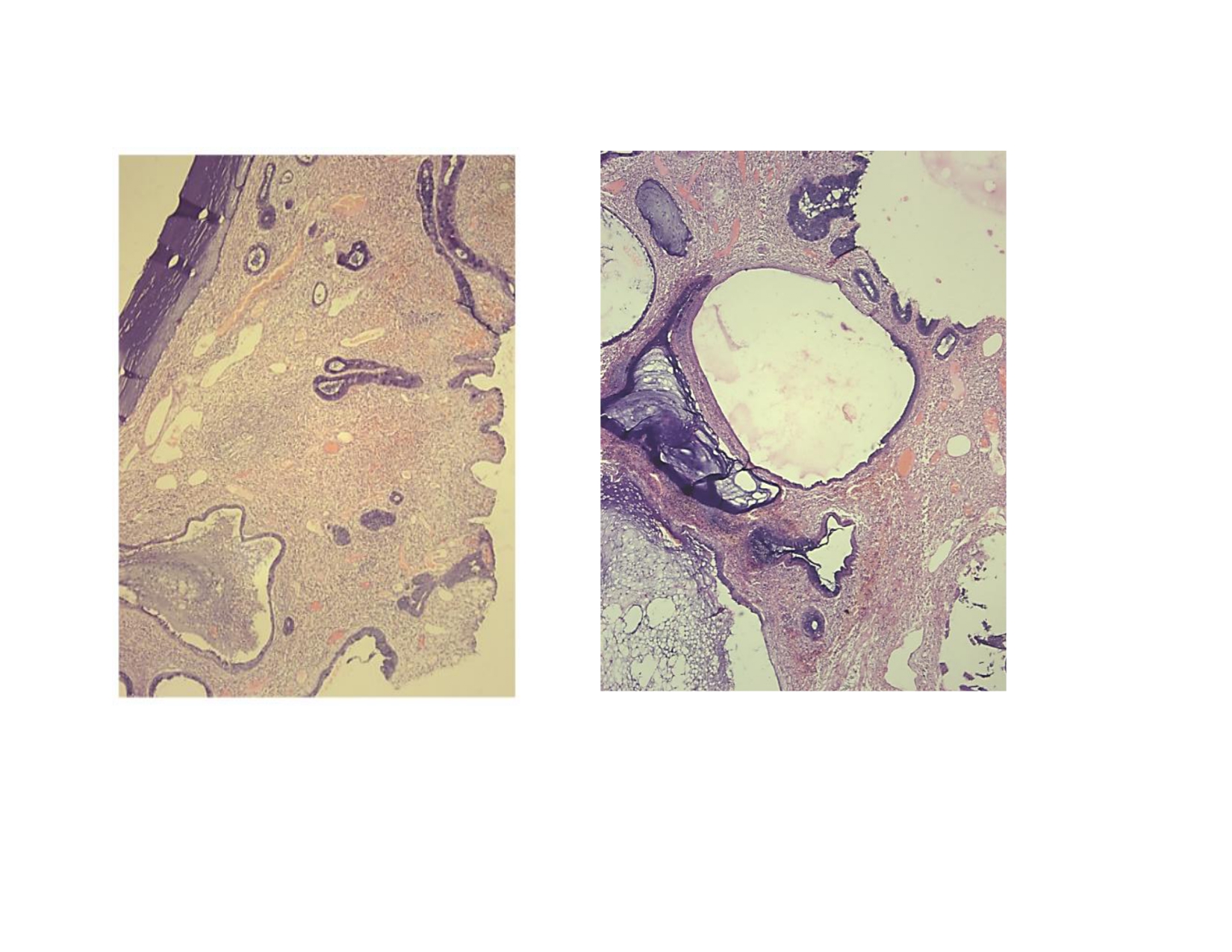
Figure: Histopathology of the Sigmoid polyp- H&E stain at low (left) and Intermediate (Right) magnification showing multiple Mucin filled Cystic spaces extending into submucosa beneath the Muscularis Mucosa. The cysts are lined by benign epithelium without dysplasia, without significant atypia, without destructive glandular invasion which shows features consistent with benign nature of CCP.
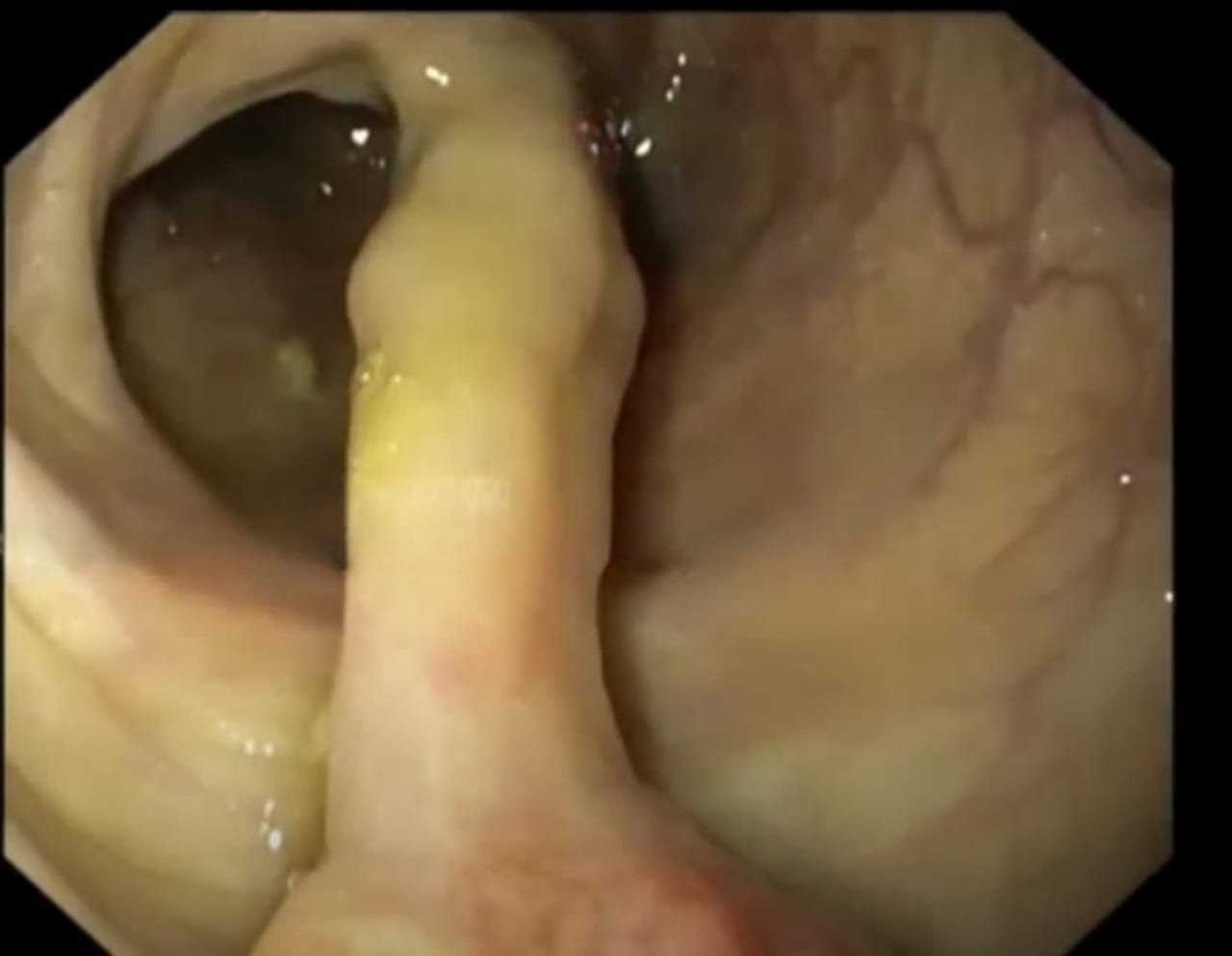
Figure: Colonoscopy showing 4 x 2 x 1.5 cm pedunculated polyp in sigmoid colon. The Polyp surface is smooth and glistening, with a mucosal appearance that is grossly intact, though a subtle yellowish discoloration and mild mucinous coating is noted-possibly reflecting underlying mucin filled Cystic spaces, which are characteristic of Colitis Cystica Profunda.
Disclosures:
Riyakumari Patel indicated no relevant financial relationships.
Ishika Golakiya indicated no relevant financial relationships.
Yash Hapani indicated no relevant financial relationships.
Pradip Vekariya indicated no relevant financial relationships.
Niralkumar Ghevariya indicated no relevant financial relationships.
Riyakumari B. Patel, MBBS1, Ishika A. Golakiya, MBBS2, Yash M. Hapani, MBBS3, Pradip Vekariya, MD, DM (Gastroenterology)4, Niralkumar L. Ghevariya, MBBS5. P2520 - Uncommon Pathology in Uncommon Age: Colitis Cystica Profunda in the Youngest Pediatric Case to Date, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
