Monday Poster Session
Category: Colon
P2469 - ICI-Mediated Lymphocytic Colitis in a Patient with Metastatic BRAF-Mutant Malignant Melanoma

Reem Matar, MBBS
Mayo Clinic
Rochester, MN
Presenting Author(s)
Mayo Clinic, Rochester, MN
Introduction:
Immune checkpoint inhibitors (ICIs) have revolutionized the treatment of metastatic cancers, but their widespread use has led to an increasing number of immune-related adverse events (irAEs). Gastrointestinal irAEs can range from diarrhea to severe immune checkpoint inhibitor induced colitis (ICI colitis). This case highlights the diagnostic approach and management of an emerging subset of ICI colitis – ICI-mediated lymphocytic colitis – in a patient with advanced BRAF-mutant melanoma.
Case Description/
Methods:
A 72-year-old male with a history of metastatic BRAF-mutant malignant melanoma (on encorafenib, binimetinib, and Opdualag) presented with two weeks of severe nausea, vomiting, and diarrhea. The patient also had a prior history of ICI-associated acute interstitial nephritis (AIN), for which he was tapering off prednisone.
Upon presenting to the emergency department (ED), the patient was hemodynamically stable. Lab results revealed elevated creatinine (2.62 mg/dL), hypokalemia (K 3.2 mmol/l), low bicarbonate level (19 mmol/l), and an elevated anion gap of 17. CT of the abdomen and pelvis revealed no acute intra-abdominal pathology. GI pathogen panel testing was negative.
Given the persistence of diarrhea despite cessation of the patient’s cancer therapies (encorafenib and binimetinib), a flexible sigmoidoscopy was performed which did not reveal any evidence of gross colitis. However, biopsy revealed lymphocytic infiltrate (Figure 1), consistent with ICI-mediated lymphocytic colitis. The patient was started on intravenous methylprednisolone 80 mg daily, which was later increased to 160 mg daily due to inadequate symptom resolution. Additionally, oral budesonide 12 mg daily was initiated. He also received one dose of infliximab 5 mg/kg due to need of high-dose steroids. The patient's symptoms improved and he was discharged after 7 days of inpatient care.
Discussion:
ICI-induced colitis is increasingly recognized as a spectrum of disease presentations, with histologic examination playing a crucial role in diagnosis. In this case, persistent diarrhea despite discontinuation of targeted therapies raised suspicion for irAE, with biopsy findings suggestive of ICI-mediated lymphocytic colitis . The patient's symptoms improved with corticosteroids, budesonide, and infliximab, emphasizing the importance of early recognition and treatment. This case contributes to the growing body of evidence supporting the careful monitoring of gastrointestinal symptoms in patients undergoing ICI therapy.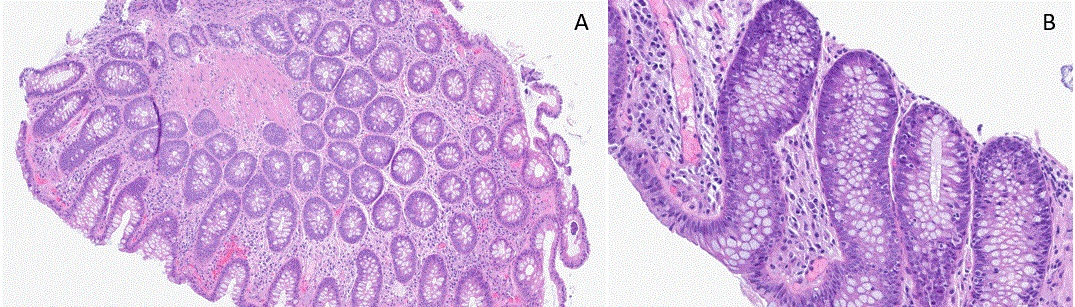
Figure: Figure 1. H&E stain of biopsy demonstrating lymphocytic colitis a) 6x magnification b) 16x magnification
Disclosures:
Reem Matar indicated no relevant financial relationships.
Samiddhi Weerasiri indicated no relevant financial relationships.
Khalid Abu-Zeinah indicated no relevant financial relationships.
Tanish Modi indicated no relevant financial relationships.
Allison Ducharme-Smith indicated no relevant financial relationships.
Reem Matar, MBBS, Samiddhi Weerasiri, MD, Khalid Abu-Zeinah, MBBCh, Tanish Modi, MBBS, Allison Ducharme-Smith, MD. P2469 - ICI-Mediated Lymphocytic Colitis in a Patient with Metastatic BRAF-Mutant Malignant Melanoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
