Monday Poster Session
Category: Biliary/Pancreas
P2365 - Synchronous Primary Pancreatic Neuroendocrine Tumor and Intrahepatic Cholangiocarcinoma Discovered During Breast Cancer Surveillance of CA 27.29
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Samee Farooqi, DO
Advocate Christ Medical Center
Oak Lawn, IL
Presenting Author(s)
Samee Farooqi, DO, Ahmad Mardini, MD, Omair Syed, DO, Krishna Shah, MD, Allison Isabelli, DO, Matthew Posen, DO, Prashant Joshi, MD
Advocate Christ Medical Center, Oak Lawn, IL
Introduction: Two separate primary malignancies presenting simultaneously in the pancreas and liver are rare and present a diagnostic and therapeutic challenge. Pancreatic neuroendocrine tumors (PNETs) and intrahepatic cholangiocarcinoma (ICC) are distinct neoplasms with differing pathology and treatment implications. Here we report a case of these two separate primary malignancies found through breast cancer surveillance of CA 27.29 tumor marker.
Case Description/
Methods: A 70-year-old woman with a history of invasive ductal carcinoma (IDC) of the left breast, diagnosed in 2018 and treated with lumpectomy and radiation therapy. She remained in remission and was monitored annually with imaging and tumor markers, including CA 27.29. In 2024, CA 27.29 rose sharply to 87.3 U/mL (normal: 0–40), prompting a PET scan that revealed a hypermetabolic right hepatic dome mass without disease recurrence in the breast.
Ultrasound-guided liver biopsy revealed moderately differentiated adenocarcinoma with immunoprofile consistent with pancreaticobiliary origin. Tumor markers revealed elevated CA 19-9 and AFP. Surgical evaluation determined the hepatic mass was unresectable due to its central location and bilobar involvement.
Further evaluation with MRCP revealed a 2.1 × 1.9 cm lesion in the pancreatic head. Additional liver lesions (up to 9.5 cm) were noted. EUS identified a 22 × 20 mm well-demarcated, hypoechoic, hypervascular pancreatic mass. FNA confirmed a grade 1 well-differentiated PNET.
The patient was started on gemcitabine, cisplatin, and durvalumab for presumed ICC. The PNET was early stage and did not require treatment. Follow-up CT at 3 months showed stable disease; however, a PET scan at 6 months revealed progression with new hypermetabolic lesions in the liver, pancreas, and lungs. Therapy was transitioned to ivosidenib, a targeted agent for IDH1-mutated cholangiocarcinoma.
Discussion: This case highlights the diagnostic challenge of elevated tumor markers in cancer surveillance. CA 27.29, while typically used for monitoring breast cancer, lacks specificity and may rise in benign conditions or other malignancies, including gastrointestinal and hepatic cancers. Its unexplained elevation should prompt broader evaluation. The rare coexistence of intrahepatic cholangiocarcinoma and pancreatic neuroendocrine tumor emphasizes the need for accurate classification, as treatment strategies vary. Comprehensive imaging, histopathology, and molecular profiling were crucial in guiding diagnosis and management.
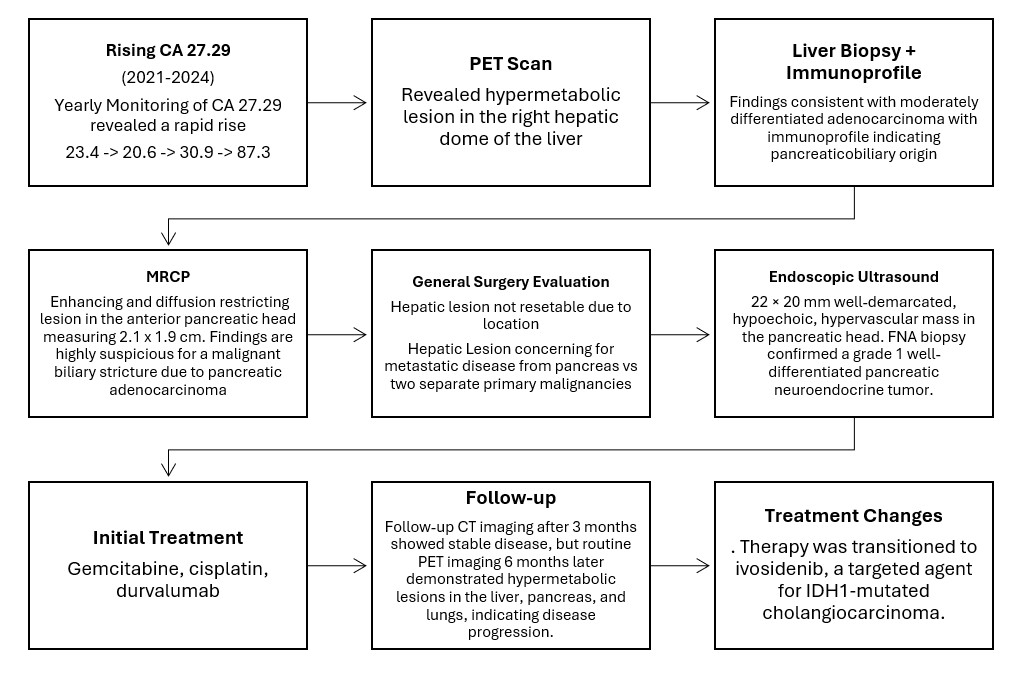
Figure: Flow chart summary of disease course.
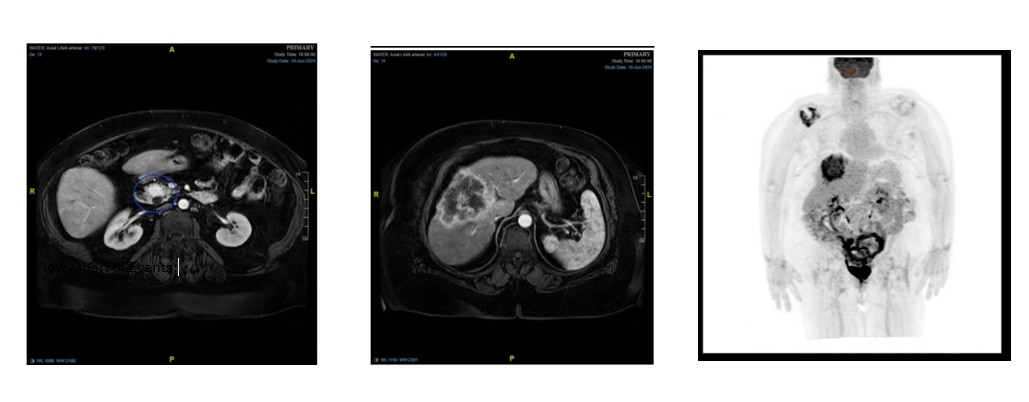
Figure: CT scan and PET images of PNET, ICC, and hypermetabolic lesions (left to right).
Disclosures:
Samee Farooqi indicated no relevant financial relationships.
Ahmad Mardini indicated no relevant financial relationships.
Omair Syed indicated no relevant financial relationships.
Krishna Shah indicated no relevant financial relationships.
Allison Isabelli indicated no relevant financial relationships.
Matthew Posen indicated no relevant financial relationships.
Prashant Joshi indicated no relevant financial relationships.
Samee Farooqi, DO, Ahmad Mardini, MD, Omair Syed, DO, Krishna Shah, MD, Allison Isabelli, DO, Matthew Posen, DO, Prashant Joshi, MD. P2365 - Synchronous Primary Pancreatic Neuroendocrine Tumor and Intrahepatic Cholangiocarcinoma Discovered During Breast Cancer Surveillance of CA 27.29, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Advocate Christ Medical Center, Oak Lawn, IL
Introduction: Two separate primary malignancies presenting simultaneously in the pancreas and liver are rare and present a diagnostic and therapeutic challenge. Pancreatic neuroendocrine tumors (PNETs) and intrahepatic cholangiocarcinoma (ICC) are distinct neoplasms with differing pathology and treatment implications. Here we report a case of these two separate primary malignancies found through breast cancer surveillance of CA 27.29 tumor marker.
Case Description/
Methods: A 70-year-old woman with a history of invasive ductal carcinoma (IDC) of the left breast, diagnosed in 2018 and treated with lumpectomy and radiation therapy. She remained in remission and was monitored annually with imaging and tumor markers, including CA 27.29. In 2024, CA 27.29 rose sharply to 87.3 U/mL (normal: 0–40), prompting a PET scan that revealed a hypermetabolic right hepatic dome mass without disease recurrence in the breast.
Ultrasound-guided liver biopsy revealed moderately differentiated adenocarcinoma with immunoprofile consistent with pancreaticobiliary origin. Tumor markers revealed elevated CA 19-9 and AFP. Surgical evaluation determined the hepatic mass was unresectable due to its central location and bilobar involvement.
Further evaluation with MRCP revealed a 2.1 × 1.9 cm lesion in the pancreatic head. Additional liver lesions (up to 9.5 cm) were noted. EUS identified a 22 × 20 mm well-demarcated, hypoechoic, hypervascular pancreatic mass. FNA confirmed a grade 1 well-differentiated PNET.
The patient was started on gemcitabine, cisplatin, and durvalumab for presumed ICC. The PNET was early stage and did not require treatment. Follow-up CT at 3 months showed stable disease; however, a PET scan at 6 months revealed progression with new hypermetabolic lesions in the liver, pancreas, and lungs. Therapy was transitioned to ivosidenib, a targeted agent for IDH1-mutated cholangiocarcinoma.
Discussion: This case highlights the diagnostic challenge of elevated tumor markers in cancer surveillance. CA 27.29, while typically used for monitoring breast cancer, lacks specificity and may rise in benign conditions or other malignancies, including gastrointestinal and hepatic cancers. Its unexplained elevation should prompt broader evaluation. The rare coexistence of intrahepatic cholangiocarcinoma and pancreatic neuroendocrine tumor emphasizes the need for accurate classification, as treatment strategies vary. Comprehensive imaging, histopathology, and molecular profiling were crucial in guiding diagnosis and management.
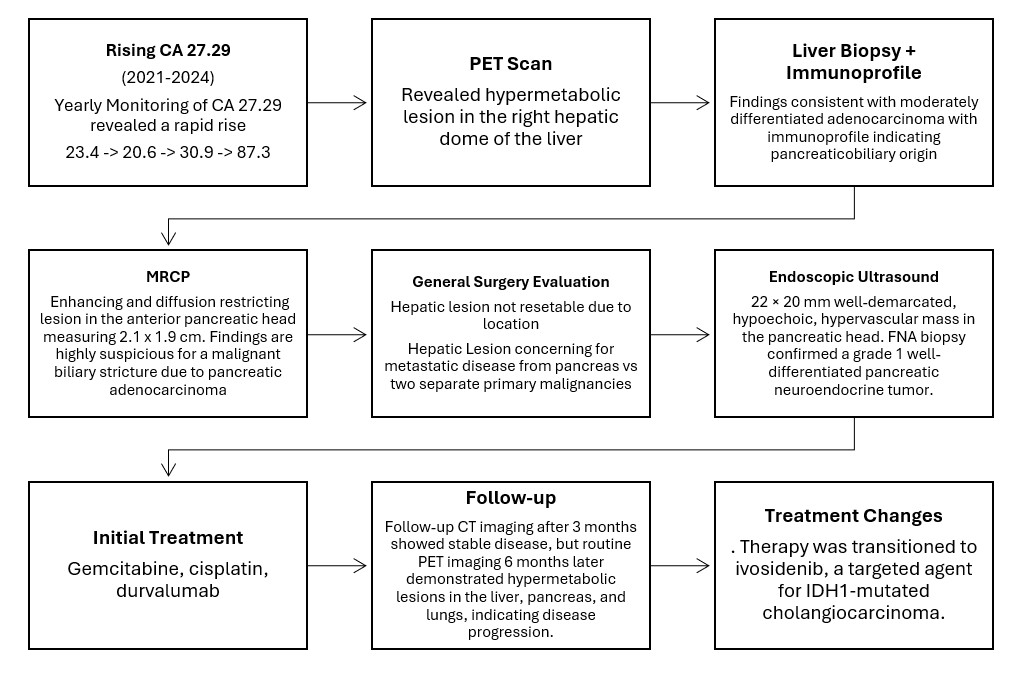
Figure: Flow chart summary of disease course.
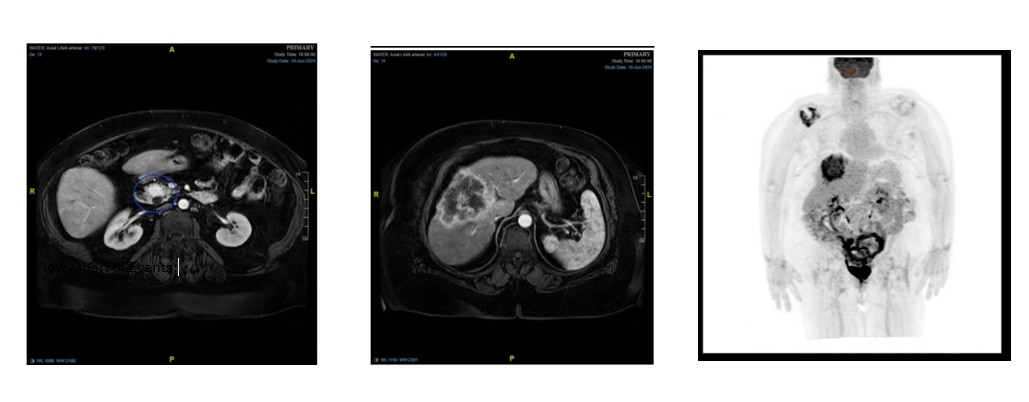
Figure: CT scan and PET images of PNET, ICC, and hypermetabolic lesions (left to right).
Disclosures:
Samee Farooqi indicated no relevant financial relationships.
Ahmad Mardini indicated no relevant financial relationships.
Omair Syed indicated no relevant financial relationships.
Krishna Shah indicated no relevant financial relationships.
Allison Isabelli indicated no relevant financial relationships.
Matthew Posen indicated no relevant financial relationships.
Prashant Joshi indicated no relevant financial relationships.
Samee Farooqi, DO, Ahmad Mardini, MD, Omair Syed, DO, Krishna Shah, MD, Allison Isabelli, DO, Matthew Posen, DO, Prashant Joshi, MD. P2365 - Synchronous Primary Pancreatic Neuroendocrine Tumor and Intrahepatic Cholangiocarcinoma Discovered During Breast Cancer Surveillance of CA 27.29, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
