Monday Poster Session
Category: Biliary/Pancreas
P2362 - Two Ducts, One Drug: Pembrolizumab-Induced Pancreatic Injury Manifesting as Double-Duct Sign
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- TA
Tareq Alsaleh, MD
Department of Internal Medicine, AdventHealth Orlando
Orlando, FL
Presenting Author(s)
Tareq Alsaleh, MD1, Mohamad Khaled Almujarkesh, MD2, Abdullah Abbasi, MD3, Mustafa Arain, MD3, John George, MD2
1Department of Internal Medicine, AdventHealth Orlando, Orlando, FL; 2Department of Gastroenterology and Hepatology, AdventHealth Orlando, Orlando, FL; 3Center for Interventional Endoscopy, AdventHealth Orlando, Orlando, FL
Introduction: Immune checkpoint inhibitors (ICIs) have utility in multiple solid and hematologic malignancies. Here, we present a rare case of ICI-induced pancreatic injury (ICI-PI) presenting as symptomatic strictures in both the pancreatic duct (PD) and common bile duct (CBD).
Case Description/
Methods: A 72-year-old female with a past medical history of renal cell carcinoma treated with left radical nephrectomy a year ago and currently on her 17th cycle of adjuvant pembrolizumab at 200 mg every 3 weeks presented to the clinic with one week of epigastric pain, nausea, and vomiting. She denied alcohol drinking, smoking, or family history of pancreatic disease.
Physical exam revealed epigastric tenderness without jaundice. Lipase was elevated at 354 U/L. Computed tomography (CT) and MRI showed dilatation of PD and CBD, with abrupt termination in the pancreatic head, consistent with “double duct sign” (Figure 1A). No distinct masses or signs of acute pancreatitis were seen.
Endoscopic ultrasound (EUS) revealed strictures in the PD and CBD, with mild upstream dilation and atrophic parenchyma in the body and tail of the pancreas. ERCP showed similar findings to EUS (Figure 1B). Cytology brushings revealed benign-appearing clusters of glandular epithelial cells (Figure 2). Next generation sequencing of the brushings was negative.
Pembrolizumab was discontinued, and on an 8-week follow-up visit she reported clinical improvement. ERCP then showed resolution of the previously seen stenosis.
Discussion: Pembrolizumab is an ICI that disinhibits T cells, facilitating a heightened immune system response with antitumor effects as well as immune-related adverse events, including ICI-PI.
ICI-PI has a wide spectrum of clinical presentations, ranging from asymptomatic elevations of pancreatic enzymes to severe necrotizing pancreatitis, but double-duct sign is an unusual finding.
ICI-PI is a diagnosis of exclusion that can be made after other potential causes are ruled out. The mainstay of management is intravenous fluid hydration, pain control, and holding the ICI. A 4–6-week steroid taper can also be used, but their benefit remains uncertain. In severe cases, ICIs should be permanently discontinued.
It is important to consider ICIs as culprits of pancreatic injury in patients taking them, even when double-duct sign, more commonly seen in malignancy, is present. Further studies are needed to better define the role of steroids and immunosuppressants in management of ICI-PI.
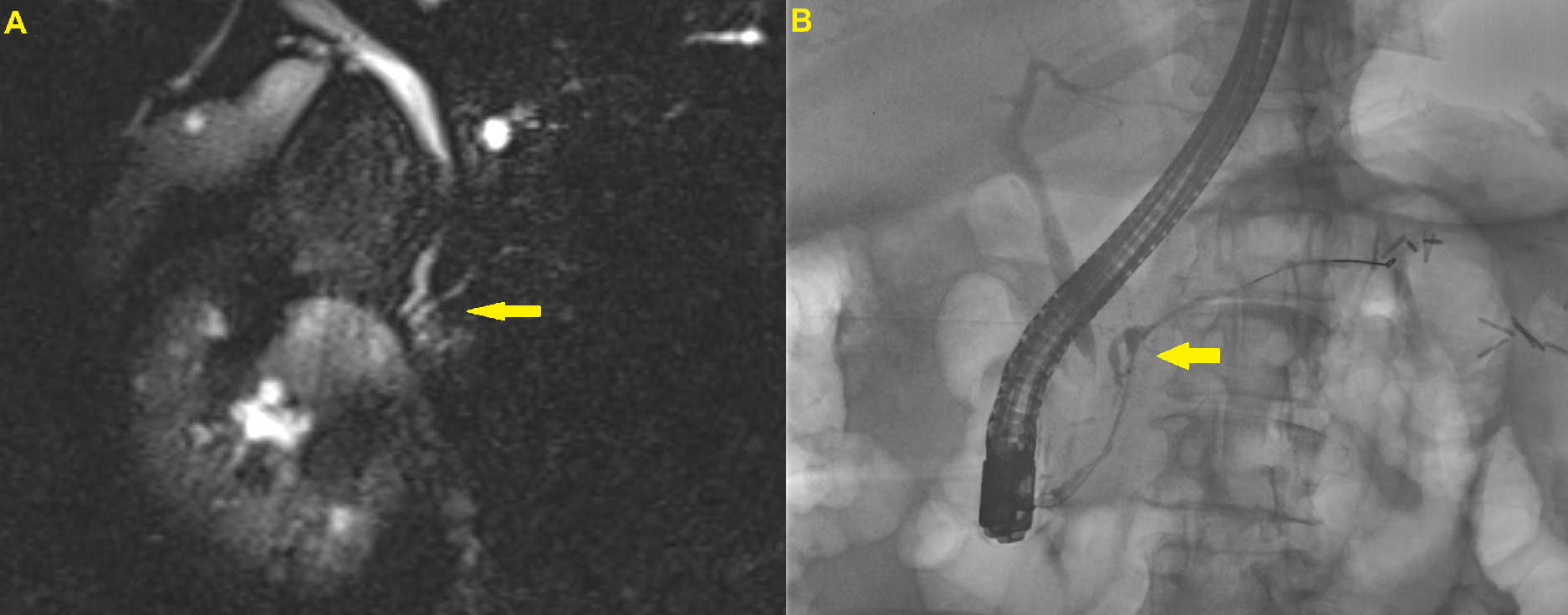
Figure: Figure 1A. Borderline dilatation in the PD and a 9 mm CBD, both abruptly terminating in the pancreatic head, consistent with “double duct sign”.
Figure 1B. Cholangiogram showed an indeterminate distal bile duct stricture, and pancreatogram showed a stricture in the neck of the pancreas with mild upstream dilation.
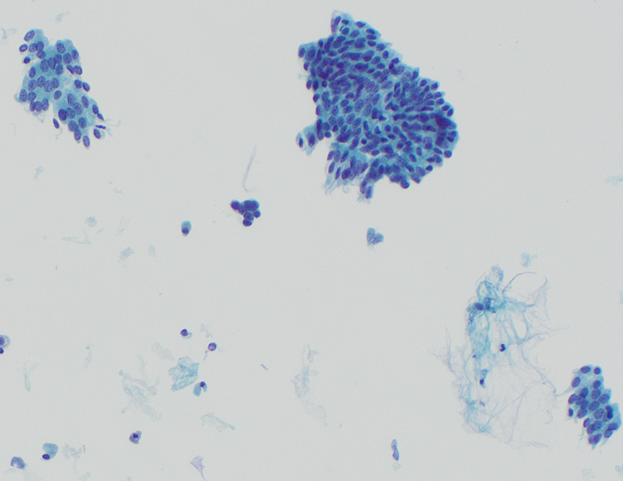
Figure: Figure 2. Benign-appearing clusters of glandular epithelial cells on cytology brushings from ERCP.
Disclosures:
Tareq Alsaleh indicated no relevant financial relationships.
Mohamad Khaled Almujarkesh indicated no relevant financial relationships.
Abdullah Abbasi indicated no relevant financial relationships.
Mustafa Arain: Boston Scientific – Consultant. Cook Endoscopy – Consultant. Olympus – Consultant.
John George indicated no relevant financial relationships.
Tareq Alsaleh, MD1, Mohamad Khaled Almujarkesh, MD2, Abdullah Abbasi, MD3, Mustafa Arain, MD3, John George, MD2. P2362 - Two Ducts, One Drug: Pembrolizumab-Induced Pancreatic Injury Manifesting as Double-Duct Sign, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Department of Internal Medicine, AdventHealth Orlando, Orlando, FL; 2Department of Gastroenterology and Hepatology, AdventHealth Orlando, Orlando, FL; 3Center for Interventional Endoscopy, AdventHealth Orlando, Orlando, FL
Introduction: Immune checkpoint inhibitors (ICIs) have utility in multiple solid and hematologic malignancies. Here, we present a rare case of ICI-induced pancreatic injury (ICI-PI) presenting as symptomatic strictures in both the pancreatic duct (PD) and common bile duct (CBD).
Case Description/
Methods: A 72-year-old female with a past medical history of renal cell carcinoma treated with left radical nephrectomy a year ago and currently on her 17th cycle of adjuvant pembrolizumab at 200 mg every 3 weeks presented to the clinic with one week of epigastric pain, nausea, and vomiting. She denied alcohol drinking, smoking, or family history of pancreatic disease.
Physical exam revealed epigastric tenderness without jaundice. Lipase was elevated at 354 U/L. Computed tomography (CT) and MRI showed dilatation of PD and CBD, with abrupt termination in the pancreatic head, consistent with “double duct sign” (Figure 1A). No distinct masses or signs of acute pancreatitis were seen.
Endoscopic ultrasound (EUS) revealed strictures in the PD and CBD, with mild upstream dilation and atrophic parenchyma in the body and tail of the pancreas. ERCP showed similar findings to EUS (Figure 1B). Cytology brushings revealed benign-appearing clusters of glandular epithelial cells (Figure 2). Next generation sequencing of the brushings was negative.
Pembrolizumab was discontinued, and on an 8-week follow-up visit she reported clinical improvement. ERCP then showed resolution of the previously seen stenosis.
Discussion: Pembrolizumab is an ICI that disinhibits T cells, facilitating a heightened immune system response with antitumor effects as well as immune-related adverse events, including ICI-PI.
ICI-PI has a wide spectrum of clinical presentations, ranging from asymptomatic elevations of pancreatic enzymes to severe necrotizing pancreatitis, but double-duct sign is an unusual finding.
ICI-PI is a diagnosis of exclusion that can be made after other potential causes are ruled out. The mainstay of management is intravenous fluid hydration, pain control, and holding the ICI. A 4–6-week steroid taper can also be used, but their benefit remains uncertain. In severe cases, ICIs should be permanently discontinued.
It is important to consider ICIs as culprits of pancreatic injury in patients taking them, even when double-duct sign, more commonly seen in malignancy, is present. Further studies are needed to better define the role of steroids and immunosuppressants in management of ICI-PI.
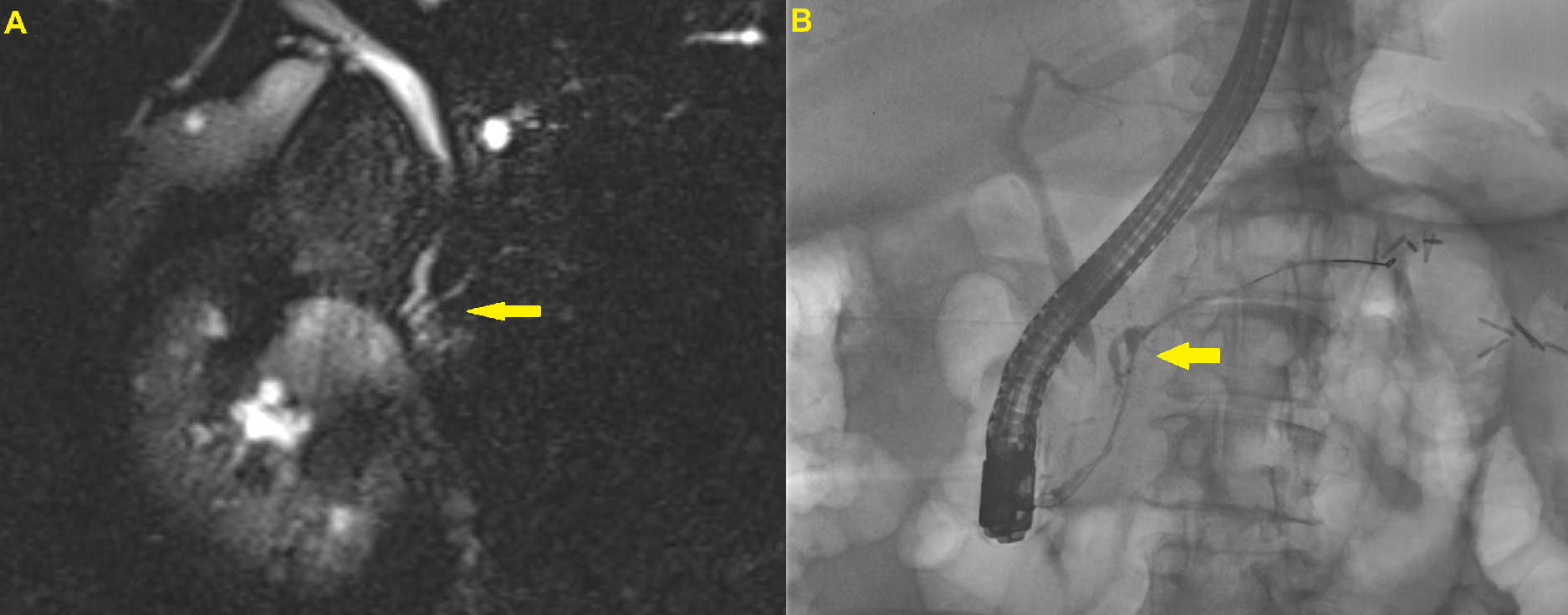
Figure: Figure 1A. Borderline dilatation in the PD and a 9 mm CBD, both abruptly terminating in the pancreatic head, consistent with “double duct sign”.
Figure 1B. Cholangiogram showed an indeterminate distal bile duct stricture, and pancreatogram showed a stricture in the neck of the pancreas with mild upstream dilation.
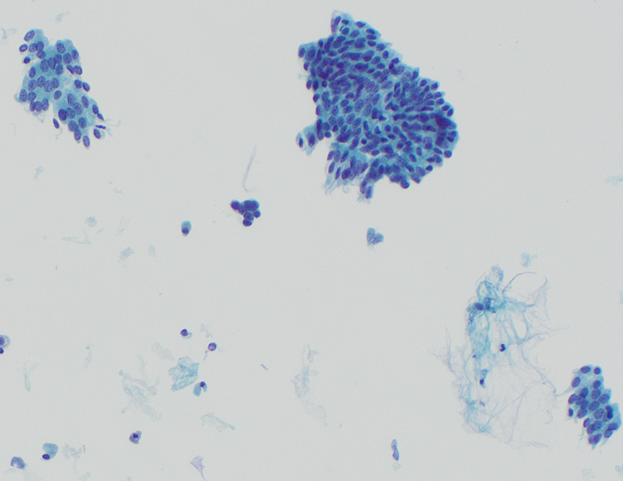
Figure: Figure 2. Benign-appearing clusters of glandular epithelial cells on cytology brushings from ERCP.
Disclosures:
Tareq Alsaleh indicated no relevant financial relationships.
Mohamad Khaled Almujarkesh indicated no relevant financial relationships.
Abdullah Abbasi indicated no relevant financial relationships.
Mustafa Arain: Boston Scientific – Consultant. Cook Endoscopy – Consultant. Olympus – Consultant.
John George indicated no relevant financial relationships.
Tareq Alsaleh, MD1, Mohamad Khaled Almujarkesh, MD2, Abdullah Abbasi, MD3, Mustafa Arain, MD3, John George, MD2. P2362 - Two Ducts, One Drug: Pembrolizumab-Induced Pancreatic Injury Manifesting as Double-Duct Sign, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
