Monday Poster Session
Category: Biliary/Pancreas
P2324 - No Stones to Overturn: An Unexpected Cause of Acute Pancreatitis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Faizan Ahmed, MD (he/him/his)
HCA Florida Healthcare
Clearwater, FL
Presenting Author(s)
Faizan Ahmed, MD1, Andrew Ondracek, DO2, Rohan Shah, MD3, Robert Ondracek, DO3, Patrick Stocker, PhD3, Olugbenga Oyesanmi, MD3
1HCA Florida Healthcare, Clearwater, FL; 2HCA Florida Largo Hospital, Largo, FL; 3HCA Florida Healthcare, Saint Petersburg, FL
Introduction: Hemorrhagic cholecystitis, bleeding into the gallbladder wall or lumen, represents < 4% of cholecystitis but can provoke pancreatitis when clot obstructs the cystic or common bile duct¹-². Trauma, malignancy, anticoagulation, cirrhosis, and renal failure increase risk³. Overlap with calculous disease delays recognition and raises mortality.
Case Description/
Methods: A 69-year-old man with atrial fibrillation on warfarin, Coronary Artery Disease (CAD), Heart Failure with Reduced Ejection Fraction (HFrEF), and gout presented with sudden diffuse abdominal pain, nausea, and diaphoresis. Vitals: heart rate 132, Mean Arterial Pressure (MAP) 58mmHg (on norepinephrine), temperature 38°C. Abdomen distended, diffusely tender, no Murphy sign. Labs: White Blood Cell (WBC) 17.4×10⁹/L, hemoglobin 11.2g/dL, platelets 212×10⁹/L, International Normalized Ratio (INR) 3.4, total bilirubin 1.8mg/dL, alanine aminotransferase 88U/L, lipase > 30 000U/L; Bedside Index of Severity in Acute Pancreatitis (BISAP) 2, 48-h Ranson 6. Right upper quadrant ultrasound showed sludge, trace pericholecystic fluid, no stones. Computed Tomography (CT) was deferred. Warfarin reversed with Prothrombin Complex Concentrate (PCC) + vitamin K. A 10-F cholecystostomy tube drained sanguineous bile, confirming hemorrhagic cholecystitis. Despite drainage and broad antibiotics, he developed encephalopathy, hypoxemia, and refractory shock requiring intubation and additional vasopressors. Organ support was weaned; he left Intensive Care Unit (ICU) on day 6 and rehab on day 10. Laparoscopic cholecystectomy at 6 weeks was uneventful; pathology showed chronic cholecystitis with organized clot. He was asymptomatic at 3 months and back on anticoagulation.
Discussion: Hemorrhagic cholecystitis should be considered when acalculous cholecystitis occurs in anticoagulated or coagulopathic patients¹-³. Doppler ultrasound may show non-shadowing echoes; contrast CT demonstrating high-attenuation content (HU > 50) supports blood². Clot migration can trigger severe pancreatitis, explaining this patient’s extreme lipase and high severity scores. Mortality rises with necrosis or perforation, so rapid recognition and drainage are crucial. While laparoscopic cholecystectomy is definitive, unstable patients benefit from temporizing cholecystostomy, which decompresses the biliary tree and permits physiologic optimization before surgery⁴. Prompt reversal of coagulopathy further improves safety.
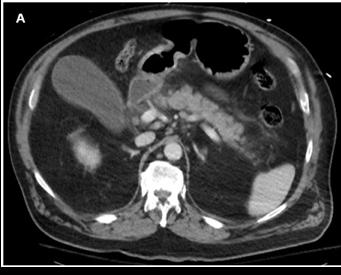
Figure: Figure 1. Computed Tomography (CT) abdomen and pelvis showed a distended gallbladder, gallbladder wall thickening, pericholecystic fluid, and inflammation of the pancreas with peri-pancreatic stranding.
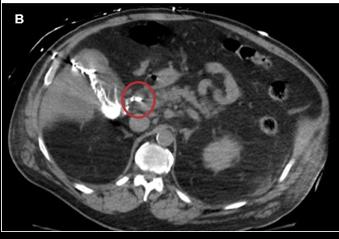
Figure: Figure 2. Confirmation of blood clot partially obstructing the common bile duct was obtained via contrast injection through the cholecystostomy tube site (Red Circle).
Disclosures:
Faizan Ahmed indicated no relevant financial relationships.
Andrew Ondracek indicated no relevant financial relationships.
Rohan Shah indicated no relevant financial relationships.
Robert Ondracek indicated no relevant financial relationships.
Patrick Stocker indicated no relevant financial relationships.
Olugbenga Oyesanmi indicated no relevant financial relationships.
Faizan Ahmed, MD1, Andrew Ondracek, DO2, Rohan Shah, MD3, Robert Ondracek, DO3, Patrick Stocker, PhD3, Olugbenga Oyesanmi, MD3. P2324 - No Stones to Overturn: An Unexpected Cause of Acute Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1HCA Florida Healthcare, Clearwater, FL; 2HCA Florida Largo Hospital, Largo, FL; 3HCA Florida Healthcare, Saint Petersburg, FL
Introduction: Hemorrhagic cholecystitis, bleeding into the gallbladder wall or lumen, represents < 4% of cholecystitis but can provoke pancreatitis when clot obstructs the cystic or common bile duct¹-². Trauma, malignancy, anticoagulation, cirrhosis, and renal failure increase risk³. Overlap with calculous disease delays recognition and raises mortality.
Case Description/
Methods: A 69-year-old man with atrial fibrillation on warfarin, Coronary Artery Disease (CAD), Heart Failure with Reduced Ejection Fraction (HFrEF), and gout presented with sudden diffuse abdominal pain, nausea, and diaphoresis. Vitals: heart rate 132, Mean Arterial Pressure (MAP) 58mmHg (on norepinephrine), temperature 38°C. Abdomen distended, diffusely tender, no Murphy sign. Labs: White Blood Cell (WBC) 17.4×10⁹/L, hemoglobin 11.2g/dL, platelets 212×10⁹/L, International Normalized Ratio (INR) 3.4, total bilirubin 1.8mg/dL, alanine aminotransferase 88U/L, lipase > 30 000U/L; Bedside Index of Severity in Acute Pancreatitis (BISAP) 2, 48-h Ranson 6. Right upper quadrant ultrasound showed sludge, trace pericholecystic fluid, no stones. Computed Tomography (CT) was deferred. Warfarin reversed with Prothrombin Complex Concentrate (PCC) + vitamin K. A 10-F cholecystostomy tube drained sanguineous bile, confirming hemorrhagic cholecystitis. Despite drainage and broad antibiotics, he developed encephalopathy, hypoxemia, and refractory shock requiring intubation and additional vasopressors. Organ support was weaned; he left Intensive Care Unit (ICU) on day 6 and rehab on day 10. Laparoscopic cholecystectomy at 6 weeks was uneventful; pathology showed chronic cholecystitis with organized clot. He was asymptomatic at 3 months and back on anticoagulation.
Discussion: Hemorrhagic cholecystitis should be considered when acalculous cholecystitis occurs in anticoagulated or coagulopathic patients¹-³. Doppler ultrasound may show non-shadowing echoes; contrast CT demonstrating high-attenuation content (HU > 50) supports blood². Clot migration can trigger severe pancreatitis, explaining this patient’s extreme lipase and high severity scores. Mortality rises with necrosis or perforation, so rapid recognition and drainage are crucial. While laparoscopic cholecystectomy is definitive, unstable patients benefit from temporizing cholecystostomy, which decompresses the biliary tree and permits physiologic optimization before surgery⁴. Prompt reversal of coagulopathy further improves safety.
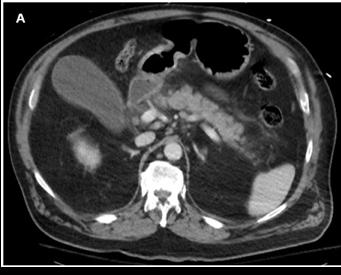
Figure: Figure 1. Computed Tomography (CT) abdomen and pelvis showed a distended gallbladder, gallbladder wall thickening, pericholecystic fluid, and inflammation of the pancreas with peri-pancreatic stranding.
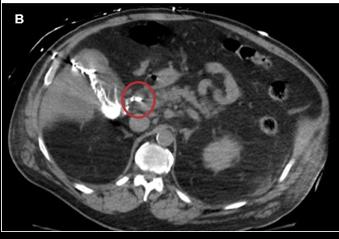
Figure: Figure 2. Confirmation of blood clot partially obstructing the common bile duct was obtained via contrast injection through the cholecystostomy tube site (Red Circle).
Disclosures:
Faizan Ahmed indicated no relevant financial relationships.
Andrew Ondracek indicated no relevant financial relationships.
Rohan Shah indicated no relevant financial relationships.
Robert Ondracek indicated no relevant financial relationships.
Patrick Stocker indicated no relevant financial relationships.
Olugbenga Oyesanmi indicated no relevant financial relationships.
Faizan Ahmed, MD1, Andrew Ondracek, DO2, Rohan Shah, MD3, Robert Ondracek, DO3, Patrick Stocker, PhD3, Olugbenga Oyesanmi, MD3. P2324 - No Stones to Overturn: An Unexpected Cause of Acute Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
