Monday Poster Session
Category: Biliary/Pancreas
P2314 - Pseudocysts and Hepatic Pseudoaneurysms: Real Culprits in a Case Investigation of Hemosuccus Pancreaticus
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Hannah Darnell, DO
University of Kentucky
Lexington, KY
Presenting Author(s)
Hannah Darnell, DO1, Ren Bryant, DO2, Seth Richardson, MD1, Patricia Santos, MD1
1University of Kentucky, Lexington, KY; 2College of Medicine, University of Kentucky, Lexington, KY
Introduction: Hemosuccus pancreaticus (HP) is a rare cause of gastrointestinal bleeding (GIB), characterized by intermittent hemorrhage into the pancreatic duct, often due to pseudoaneurysm formation following necrotizing pancreatitis. We present a 57-year-old female with recurrent, unexplained GIB. Further evaluation revealed a bleeding hepatic artery pseudoaneurysm resulting in HP. This case highlights the diagnostic challenges of HP and emphasizes the need for clinical vigilance in patients with prior pancreatitis and intermittent GIB.
Case Description/
Methods: A 57-year-old- female with a history of necrotizing pancreatitis and recent pulmonary embolism and deep venous thrombosis on apixaban presented to the hospital complaining of fatigue and hematochezia. Initial esophagogastroduodenoscopy (EGD) and colonoscopy showed no source of bleeding (Figure 1A-C). Computed tomography angiography (CTA) revealed necrotizing pancreatitis with peripancreatic fluid collections but no active bleeding (Figure 2A). Despite hemodynamic stabilization, she later experienced acute hematemesis and hemodynamic instability, prompting repeat imaging, which identified an 8mm hepatic artery pseudoaneurysm with active extravasation (Figure 2B). She underwent successful interventional radiology-guided embolization, with subsequent stabilization and resolution of GIB (Figure 2C). Follow-up imaging demonstrated reduction in pancreatic fluid collections, and she remained asymptomatic.
Discussion: HP causes less than 1% of GI hemorrhages, posing significant diagnostic and therapeutic challenges due to its intermittent nature. In 80% of cases, HP is linked to pancreatitis complications, particularly pseudoaneurysms, which develop from enzymatic vascular damage. The hepatic artery is an infrequent source of pseudoaneurysms, comprising only 2% of cases. If left untreated, the mortality rate of ruptured pseudoaneurysms approaches 90%.
CTA is the diagnostic gold standard for HP, identifying pseudoaneurysms and active bleeding. However, given HP’s intermittent bleeding nature, repeat imaging may be necessary when initial studies are negative. Endovascular embolization is the preferred treatment, boasting success rates of 60-100%, though persistent bleeding may necessitate surgical intervention.
This case underscores the importance of maintaining a high clinical suspicion for HP in patients with pancreatitis and unexplained GIB. Early recognition and prompt embolization are critical in reducing mortality and improving patient outcomes.
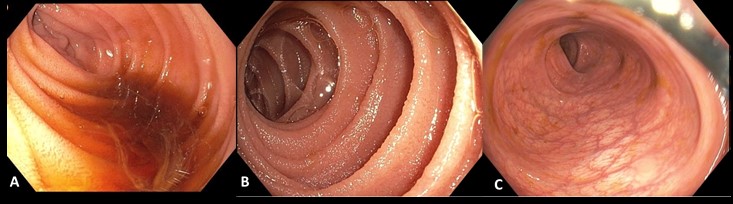
Figure: (A) EGD: 2nd part of the duodenum showing non-bloody bilious output (B) EGD: Proximal Jejunum without evidence of old blood or active bleeding (C) Colonoscopy without evidence of old blood or bleeding
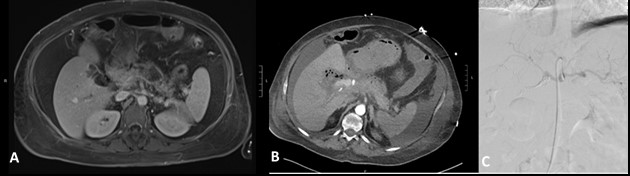
Figure: (A) MRCP revealing necrotizing pancreatitis and rim-enhancing fluid collection (B) CTA abdomen showing 8mm hepatic artery pseudoaneurysm with active extravasation (C) IR angiography at the celiac trunk following coil embolization of right hepatic artery pseudoaneurysm
Disclosures:
Hannah Darnell indicated no relevant financial relationships.
Ren Bryant indicated no relevant financial relationships.
Seth Richardson indicated no relevant financial relationships.
Patricia Santos indicated no relevant financial relationships.
Hannah Darnell, DO1, Ren Bryant, DO2, Seth Richardson, MD1, Patricia Santos, MD1. P2314 - Pseudocysts and Hepatic Pseudoaneurysms: Real Culprits in a Case Investigation of Hemosuccus Pancreaticus, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Kentucky, Lexington, KY; 2College of Medicine, University of Kentucky, Lexington, KY
Introduction: Hemosuccus pancreaticus (HP) is a rare cause of gastrointestinal bleeding (GIB), characterized by intermittent hemorrhage into the pancreatic duct, often due to pseudoaneurysm formation following necrotizing pancreatitis. We present a 57-year-old female with recurrent, unexplained GIB. Further evaluation revealed a bleeding hepatic artery pseudoaneurysm resulting in HP. This case highlights the diagnostic challenges of HP and emphasizes the need for clinical vigilance in patients with prior pancreatitis and intermittent GIB.
Case Description/
Methods: A 57-year-old- female with a history of necrotizing pancreatitis and recent pulmonary embolism and deep venous thrombosis on apixaban presented to the hospital complaining of fatigue and hematochezia. Initial esophagogastroduodenoscopy (EGD) and colonoscopy showed no source of bleeding (Figure 1A-C). Computed tomography angiography (CTA) revealed necrotizing pancreatitis with peripancreatic fluid collections but no active bleeding (Figure 2A). Despite hemodynamic stabilization, she later experienced acute hematemesis and hemodynamic instability, prompting repeat imaging, which identified an 8mm hepatic artery pseudoaneurysm with active extravasation (Figure 2B). She underwent successful interventional radiology-guided embolization, with subsequent stabilization and resolution of GIB (Figure 2C). Follow-up imaging demonstrated reduction in pancreatic fluid collections, and she remained asymptomatic.
Discussion: HP causes less than 1% of GI hemorrhages, posing significant diagnostic and therapeutic challenges due to its intermittent nature. In 80% of cases, HP is linked to pancreatitis complications, particularly pseudoaneurysms, which develop from enzymatic vascular damage. The hepatic artery is an infrequent source of pseudoaneurysms, comprising only 2% of cases. If left untreated, the mortality rate of ruptured pseudoaneurysms approaches 90%.
CTA is the diagnostic gold standard for HP, identifying pseudoaneurysms and active bleeding. However, given HP’s intermittent bleeding nature, repeat imaging may be necessary when initial studies are negative. Endovascular embolization is the preferred treatment, boasting success rates of 60-100%, though persistent bleeding may necessitate surgical intervention.
This case underscores the importance of maintaining a high clinical suspicion for HP in patients with pancreatitis and unexplained GIB. Early recognition and prompt embolization are critical in reducing mortality and improving patient outcomes.
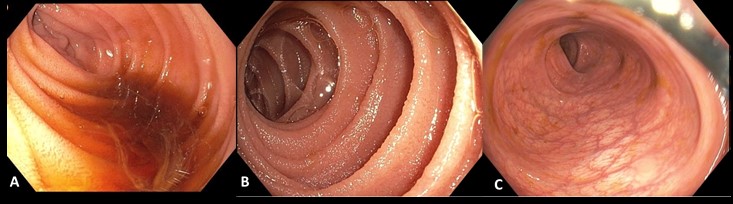
Figure: (A) EGD: 2nd part of the duodenum showing non-bloody bilious output (B) EGD: Proximal Jejunum without evidence of old blood or active bleeding (C) Colonoscopy without evidence of old blood or bleeding
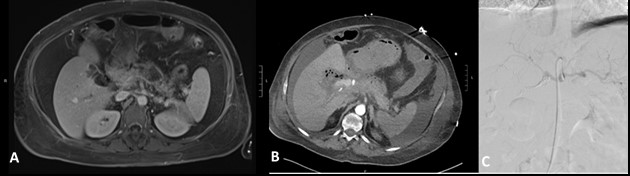
Figure: (A) MRCP revealing necrotizing pancreatitis and rim-enhancing fluid collection (B) CTA abdomen showing 8mm hepatic artery pseudoaneurysm with active extravasation (C) IR angiography at the celiac trunk following coil embolization of right hepatic artery pseudoaneurysm
Disclosures:
Hannah Darnell indicated no relevant financial relationships.
Ren Bryant indicated no relevant financial relationships.
Seth Richardson indicated no relevant financial relationships.
Patricia Santos indicated no relevant financial relationships.
Hannah Darnell, DO1, Ren Bryant, DO2, Seth Richardson, MD1, Patricia Santos, MD1. P2314 - Pseudocysts and Hepatic Pseudoaneurysms: Real Culprits in a Case Investigation of Hemosuccus Pancreaticus, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
