Monday Poster Session
Category: Biliary/Pancreas
P2302 - From Jaundice to Lymphoma: Concurrent Bile Duct and Mediastinal Lymphoma Presenting as Obstructive Jaundice
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- MA
Madhu Babu Adusumilli, MD
University of Central Florida, HCA Healthcare GME
Ocala, FL
Presenting Author(s)
Madhu Babu Adusumilli, MD1, Ashwin Rumalla, MD1, Mehak Sachdeva, MBBS2
1University of Central Florida, HCA Healthcare GME, Ocala, FL; 2University of Central Florida / HCA Florida Ocala Hospital, Ocala, FL
Introduction: Extranodal lymphoma commonly affects the GI tract, with the stomach (60%) being the most common site. Hodgkin's lymphoma (HL) of the bile duct is rare, often misdiagnosed as cholangiocarcinoma and no documented cases till now. Accurate diagnosis is crucial given the different prognoses and treatments. This case highlights the need to consider biliary lymphoma in patients with obstructive jaundice, particularly when typical risk factors for cholangiocarcinoma are absent.
Case Description/
Methods: A 32-year-old female presented with one-week nausea, vomiting, non-bloody diarrhea, and epigastric pain, with several months of weakness, shortness of breath, 20-pound weight loss, and dark urine. She had no medical history or risk factors for hepatobiliary disease. Initial liver function tests showed elevated AST 193 IU/L, ALT 441 IU/L, alkaline phosphatase 416 IU/L, total bilirubin 5.5 mg/dl, and direct bilirubin 2.9 mg/dl. CT abdomen/pelvis, gallbladder ultrasound, and MRCP showed biliary obstruction and Endoscopic ultrasound identified a mass in the distal common bile duct. Chest CT showed a mediastinal mass. Biopsy of the mediastinal mass confirmed classic Hodgkin's lymphoma. Initially Endoscopic retrograde cholangiopancreatography (ERCP) was unsuccessful as the CBD could not be cannulated. PET/CT scan revealed a large mediastinal mass and abnormal uptake in the liver region and lymph nodes, suggesting metastatic disease. Later ERCP with stenting was successful, and Fine-needle aspiration of the bile duct mass showed mature B-cells, suggesting diffuse large B-cell lymphoma or marginal zone lymphoma, but could not confirm Hodgkin's lymphoma due to lack of CD15 and CD30 testing. The patient was treated for Stage III unfavorable Hodgkin's lymphoma with chemotherapy (brentuximab + doxorubicin, vinblastine, dacarbazine) and biliary stent was removed after 7 weeks, resolving the bile duct mass and improving systemic disease and biliary obstruction.
Discussion: Definitive preoperative diagnosis of HL in the bile duct is challenging due to sampling difficulties. This case is the third reported instance of pre-operative diagnosis via ultrasound-guided biopsy among documented bile duct lymphomas. Biliary stent placement via ERCP was crucial for managing cholestasis before chemotherapy to reduce hepatotoxicity. While HL generally has a favorable prognosis, the outcome for bile duct involvement remains uncertain due to its rarity, requiring further research.
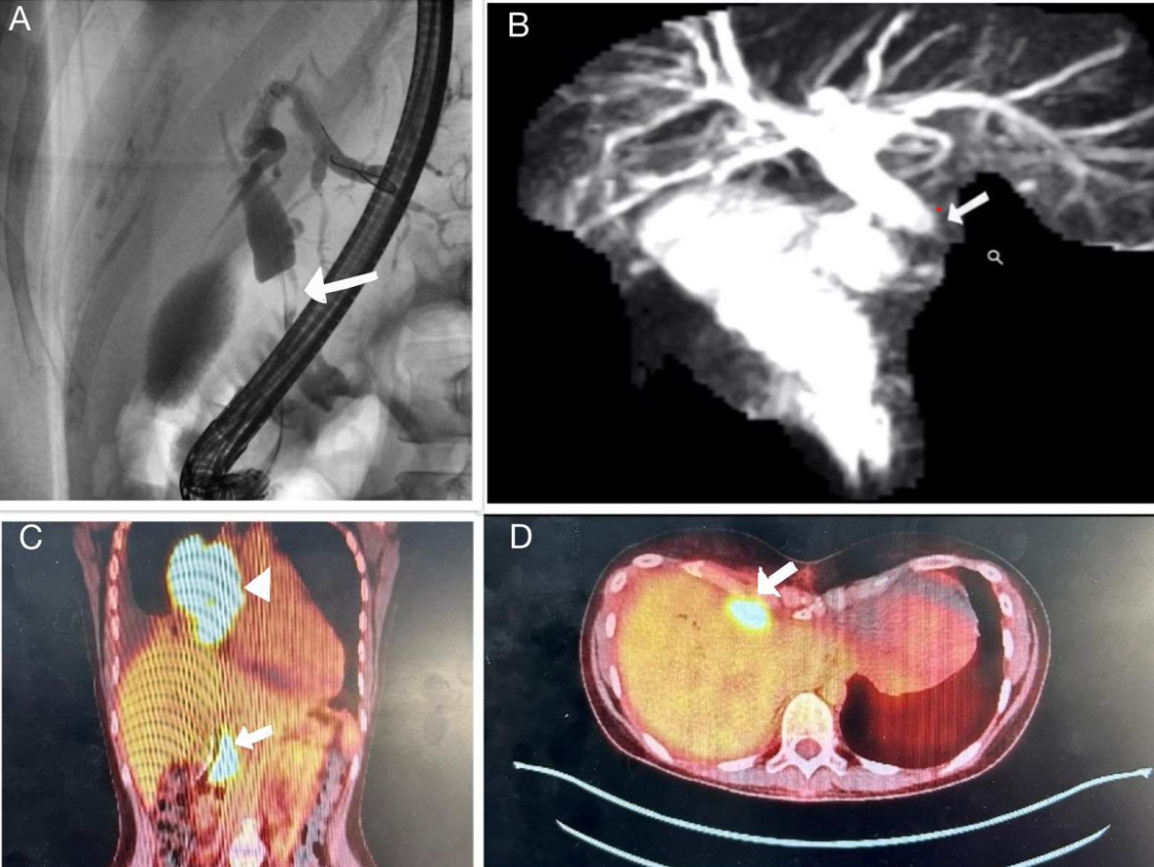
Figure: Figure A. ERCP: showing contrast filling defect at distal bile duct
Figure B. MRCP: Showing stenosis of mid portion of the common bile duct with proximal dial action of biliary tract.
Figure C. PET scan coronal view: Arrow head - mass in right mediastinum, Complete arrow - mass in bile duct
Figure D. PET scan Transverse view: Mass in bile duct.
Disclosures:
Madhu Babu Adusumilli indicated no relevant financial relationships.
Ashwin Rumalla indicated no relevant financial relationships.
Mehak Sachdeva indicated no relevant financial relationships.
Madhu Babu Adusumilli, MD1, Ashwin Rumalla, MD1, Mehak Sachdeva, MBBS2. P2302 - From Jaundice to Lymphoma: Concurrent Bile Duct and Mediastinal Lymphoma Presenting as Obstructive Jaundice, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Central Florida, HCA Healthcare GME, Ocala, FL; 2University of Central Florida / HCA Florida Ocala Hospital, Ocala, FL
Introduction: Extranodal lymphoma commonly affects the GI tract, with the stomach (60%) being the most common site. Hodgkin's lymphoma (HL) of the bile duct is rare, often misdiagnosed as cholangiocarcinoma and no documented cases till now. Accurate diagnosis is crucial given the different prognoses and treatments. This case highlights the need to consider biliary lymphoma in patients with obstructive jaundice, particularly when typical risk factors for cholangiocarcinoma are absent.
Case Description/
Methods: A 32-year-old female presented with one-week nausea, vomiting, non-bloody diarrhea, and epigastric pain, with several months of weakness, shortness of breath, 20-pound weight loss, and dark urine. She had no medical history or risk factors for hepatobiliary disease. Initial liver function tests showed elevated AST 193 IU/L, ALT 441 IU/L, alkaline phosphatase 416 IU/L, total bilirubin 5.5 mg/dl, and direct bilirubin 2.9 mg/dl. CT abdomen/pelvis, gallbladder ultrasound, and MRCP showed biliary obstruction and Endoscopic ultrasound identified a mass in the distal common bile duct. Chest CT showed a mediastinal mass. Biopsy of the mediastinal mass confirmed classic Hodgkin's lymphoma. Initially Endoscopic retrograde cholangiopancreatography (ERCP) was unsuccessful as the CBD could not be cannulated. PET/CT scan revealed a large mediastinal mass and abnormal uptake in the liver region and lymph nodes, suggesting metastatic disease. Later ERCP with stenting was successful, and Fine-needle aspiration of the bile duct mass showed mature B-cells, suggesting diffuse large B-cell lymphoma or marginal zone lymphoma, but could not confirm Hodgkin's lymphoma due to lack of CD15 and CD30 testing. The patient was treated for Stage III unfavorable Hodgkin's lymphoma with chemotherapy (brentuximab + doxorubicin, vinblastine, dacarbazine) and biliary stent was removed after 7 weeks, resolving the bile duct mass and improving systemic disease and biliary obstruction.
Discussion: Definitive preoperative diagnosis of HL in the bile duct is challenging due to sampling difficulties. This case is the third reported instance of pre-operative diagnosis via ultrasound-guided biopsy among documented bile duct lymphomas. Biliary stent placement via ERCP was crucial for managing cholestasis before chemotherapy to reduce hepatotoxicity. While HL generally has a favorable prognosis, the outcome for bile duct involvement remains uncertain due to its rarity, requiring further research.
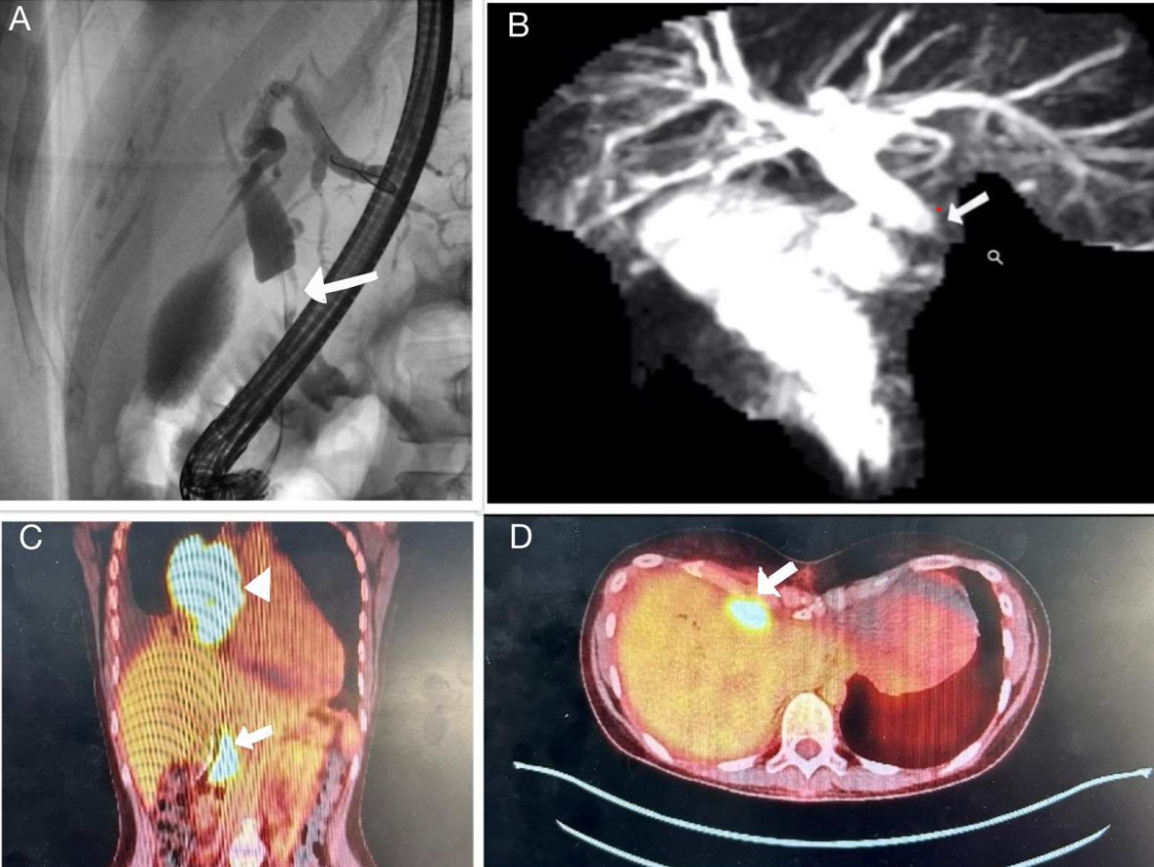
Figure: Figure A. ERCP: showing contrast filling defect at distal bile duct
Figure B. MRCP: Showing stenosis of mid portion of the common bile duct with proximal dial action of biliary tract.
Figure C. PET scan coronal view: Arrow head - mass in right mediastinum, Complete arrow - mass in bile duct
Figure D. PET scan Transverse view: Mass in bile duct.
Disclosures:
Madhu Babu Adusumilli indicated no relevant financial relationships.
Ashwin Rumalla indicated no relevant financial relationships.
Mehak Sachdeva indicated no relevant financial relationships.
Madhu Babu Adusumilli, MD1, Ashwin Rumalla, MD1, Mehak Sachdeva, MBBS2. P2302 - From Jaundice to Lymphoma: Concurrent Bile Duct and Mediastinal Lymphoma Presenting as Obstructive Jaundice, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
