Monday Poster Session
Category: Biliary/Pancreas
P2298 - Bile Peritonitis: A Post-Cholecystectomy Nightmare Secondary to Periportal and Peripancreatic Varices
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Cinthia Reyes Cruz, MD
University of Miami Miller School of Medicine at Holy Cross Hospital
Fort Lauderdale, FL
Presenting Author(s)
Cinthia Reyes Cruz, MD1, Natasha Mederos Rocha, MD2, Edina Shu, DO1, Melisa Rodriguez Suliman, MD3, Nemer Dabage-Forzoli, MD1
1University of Miami Miller School of Medicine at Holy Cross Hospital, Fort Lauderdale, FL; 2University of Miami, Fort Lauderdale, FL; 3Holy Cross Hospital, Fort Lauderdale, FL
Introduction: Bile peritonitis is a rare, severe complication resulting from bile leakage into the peritoneal cavity, typically following biliary trauma or surgery but also possible from spontaneous duct perforations or injuries. This condition is associated with a high mortality, ranging from 8-40%. Few cases have been reported secondary to mass effect and in relationship to vascular abnormalities such as varices.
Case Description/
Methods: A 47 year old man with liver cirrhosis complicated by portal hypertension, recently hospitalized for sepsis due to perforated cholecystitis status post open cholecystectomy with JP drain removal, presented to the emergency department with severe right upper quadrant pain radiating to the shoulder. On arrival, he was hemodynamically stable, but physical examination revealed an acute abdomen. Laboratory findings showed a total bilirubin of 4.3, leukocytosis, and acute kidney injury.
An abdomino-pelvic CT scan demonstrated air and fluid in the gallbladder fossa and complex right upper quadrant soft tissue changes. A hepatobiliary iminodiacetic acid scan confirmed a bile leak, prompting urgent surgical intervention and ICU admission, where he was started on broad-spectrum antibiotics. Exploratory laparotomy (ex-lap) on day 2 revealed 5 liters of old blood in the abdomen and a disrupted bile duct caused by mass effect from bleeding peri-portal and peri-pancreatic varices. A wound vacuum was placed in the open abdomen for follow-up Roux-en-Y hepatico-jejunostomy and abdominal washout, which was performed two days later.
A subsequent ex-lap with drain placements and abdominal closure with wound vac placement followed. After a normal upper gastrointestinal series, the patient’s diet was advanced as tolerated. He was safely discharged to inpatient rehabilitation with close follow-up. (Figure 2) depicts CT abdomen findings five days after discharge.
Discussion: This case highlights the importance of early recognition of bile peritonitis with prompt intervention. This is crucial to avoid progression to generalized peritonitis, sepsis, or multi-organ failure. The high mortality rate associated with this condition, should raise awareness for a low threshold for suspicion specially after surgical manipulation of biliary structures. In this specific scenario, keeping in mind liver cirrhosis as a comorbidity that puts patients at risk for varix formation alongside the biliary vasculature it’s important to recognize mass effect as a cause of bile duct damage and subsequent leak.
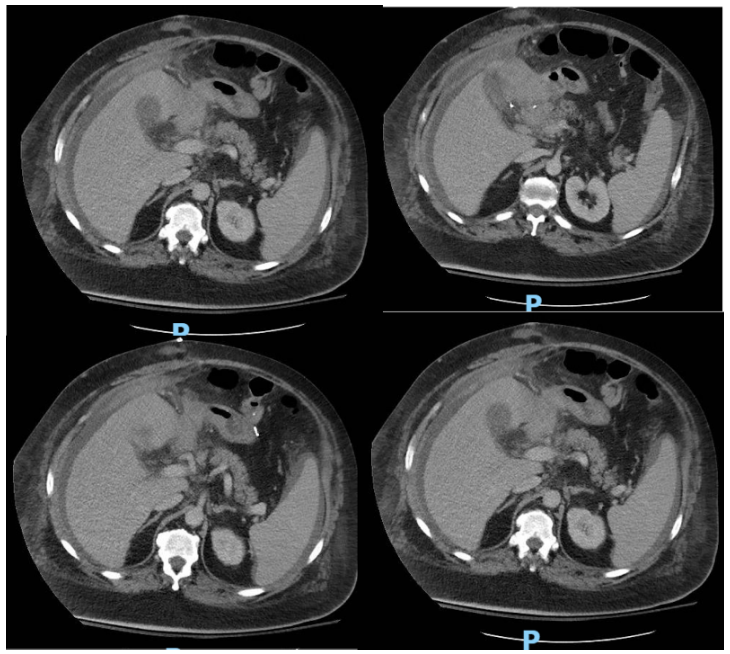
Figure: Figure 1. Abdomino-pelvic computerized (CT) scan findings on day 1 of admission.
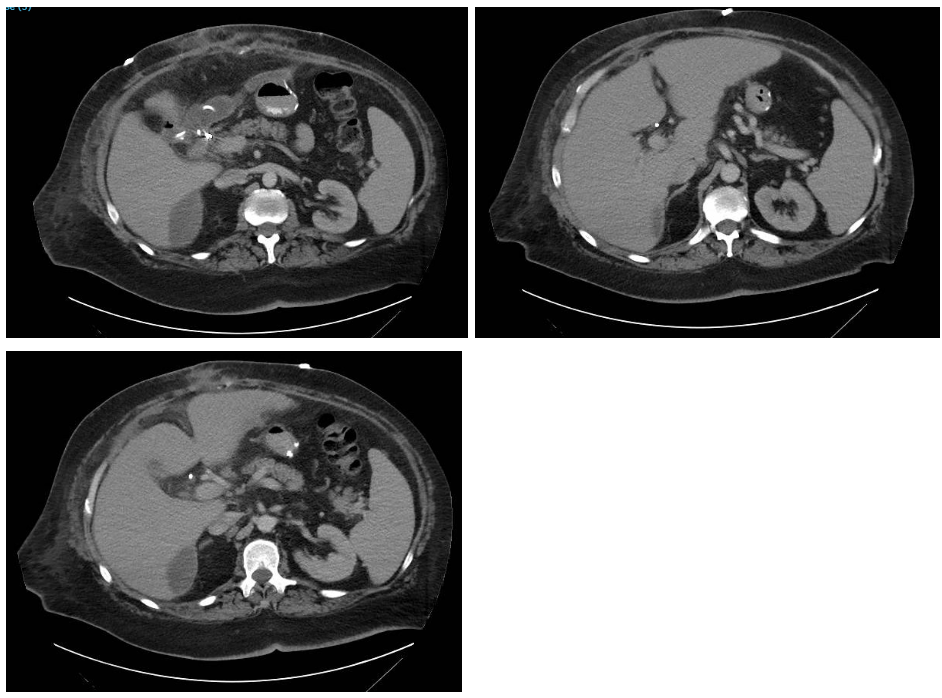
Figure: Figure 2. CT findings at day 5 after discharge
Disclosures:
Cinthia Reyes Cruz indicated no relevant financial relationships.
Natasha Mederos Rocha indicated no relevant financial relationships.
Edina Shu indicated no relevant financial relationships.
Melisa Rodriguez Suliman indicated no relevant financial relationships.
Nemer Dabage-Forzoli indicated no relevant financial relationships.
Cinthia Reyes Cruz, MD1, Natasha Mederos Rocha, MD2, Edina Shu, DO1, Melisa Rodriguez Suliman, MD3, Nemer Dabage-Forzoli, MD1. P2298 - Bile Peritonitis: A Post-Cholecystectomy Nightmare Secondary to Periportal and Peripancreatic Varices, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Miami Miller School of Medicine at Holy Cross Hospital, Fort Lauderdale, FL; 2University of Miami, Fort Lauderdale, FL; 3Holy Cross Hospital, Fort Lauderdale, FL
Introduction: Bile peritonitis is a rare, severe complication resulting from bile leakage into the peritoneal cavity, typically following biliary trauma or surgery but also possible from spontaneous duct perforations or injuries. This condition is associated with a high mortality, ranging from 8-40%. Few cases have been reported secondary to mass effect and in relationship to vascular abnormalities such as varices.
Case Description/
Methods: A 47 year old man with liver cirrhosis complicated by portal hypertension, recently hospitalized for sepsis due to perforated cholecystitis status post open cholecystectomy with JP drain removal, presented to the emergency department with severe right upper quadrant pain radiating to the shoulder. On arrival, he was hemodynamically stable, but physical examination revealed an acute abdomen. Laboratory findings showed a total bilirubin of 4.3, leukocytosis, and acute kidney injury.
An abdomino-pelvic CT scan demonstrated air and fluid in the gallbladder fossa and complex right upper quadrant soft tissue changes. A hepatobiliary iminodiacetic acid scan confirmed a bile leak, prompting urgent surgical intervention and ICU admission, where he was started on broad-spectrum antibiotics. Exploratory laparotomy (ex-lap) on day 2 revealed 5 liters of old blood in the abdomen and a disrupted bile duct caused by mass effect from bleeding peri-portal and peri-pancreatic varices. A wound vacuum was placed in the open abdomen for follow-up Roux-en-Y hepatico-jejunostomy and abdominal washout, which was performed two days later.
A subsequent ex-lap with drain placements and abdominal closure with wound vac placement followed. After a normal upper gastrointestinal series, the patient’s diet was advanced as tolerated. He was safely discharged to inpatient rehabilitation with close follow-up. (Figure 2) depicts CT abdomen findings five days after discharge.
Discussion: This case highlights the importance of early recognition of bile peritonitis with prompt intervention. This is crucial to avoid progression to generalized peritonitis, sepsis, or multi-organ failure. The high mortality rate associated with this condition, should raise awareness for a low threshold for suspicion specially after surgical manipulation of biliary structures. In this specific scenario, keeping in mind liver cirrhosis as a comorbidity that puts patients at risk for varix formation alongside the biliary vasculature it’s important to recognize mass effect as a cause of bile duct damage and subsequent leak.
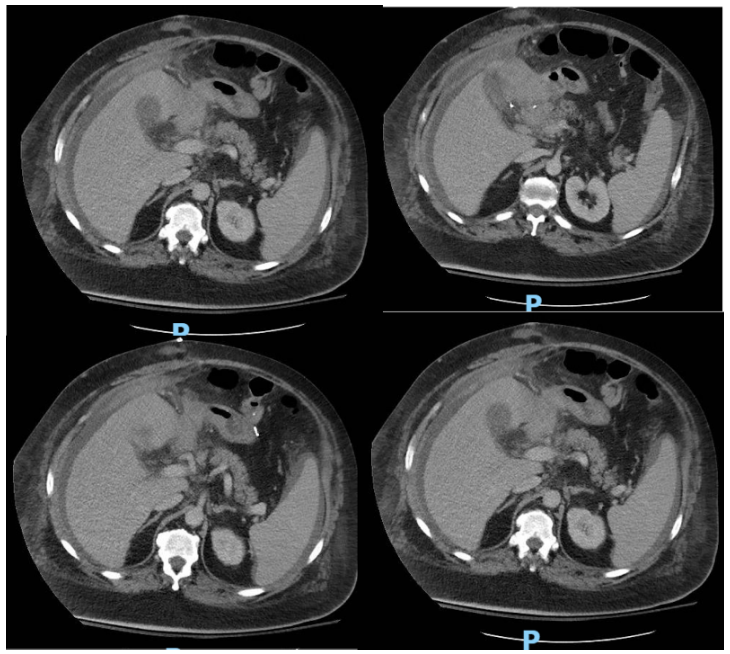
Figure: Figure 1. Abdomino-pelvic computerized (CT) scan findings on day 1 of admission.
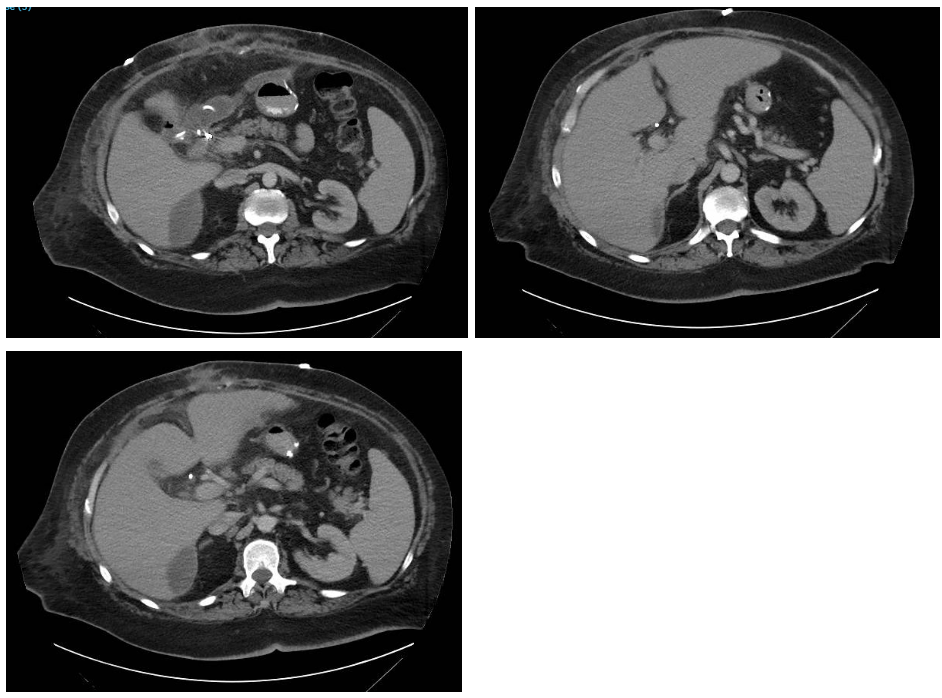
Figure: Figure 2. CT findings at day 5 after discharge
Disclosures:
Cinthia Reyes Cruz indicated no relevant financial relationships.
Natasha Mederos Rocha indicated no relevant financial relationships.
Edina Shu indicated no relevant financial relationships.
Melisa Rodriguez Suliman indicated no relevant financial relationships.
Nemer Dabage-Forzoli indicated no relevant financial relationships.
Cinthia Reyes Cruz, MD1, Natasha Mederos Rocha, MD2, Edina Shu, DO1, Melisa Rodriguez Suliman, MD3, Nemer Dabage-Forzoli, MD1. P2298 - Bile Peritonitis: A Post-Cholecystectomy Nightmare Secondary to Periportal and Peripancreatic Varices, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
